Virchow-Robin spaces (VRS) are perivascular spaces filled with interstitial fluid which surround brain blood vessels leading from the subarachnoid space through the brain parenchyma. They show similar signal intensity to CSF in all brain MRI sequences.1 It is uncertain whether VRS are a casual finding in neuroimaging or if they are linked to specific neurological diseases.
We present the case of a 55-year-old man with a history of familial HDL deficiency who was initially assessed by the psychiatric department due to behaviour and impulse control disorders, problems planning and executing actions, and a significant deterioration of psychosocial functioning. He was transferred to the neurology department due to a 6-month history of tremor in the left lower limb. When questioned directly, he reported fluctuating poor motor coordination with no hallucinations, falls, or any other symptoms. According to his family, his main symptom was apathy; they perceived no cognitive decline.
We conducted a study of higher functions. Our patient scored 28 over 30 on the Mini-Cog (the Spanish-language version of the MMSE), with errors in delayed memory, 37 on the M@T, and 32 on the Fototest. No agnosia or apraxia was observed. Speech was slow and monotonous, with marked alterations in verbal fluency. He also displayed masked facies, distal fine postural tremor in the upper limbs, no rest or action tremor, bilateral rigidity 1/4, foot tapping 1/4 on the right and 2/4 on the left, and adequate heel dropping. He was able to rise from a chair without assistance and walked with long strides, although dragging his feet slightly; no instability was seen. Our patient showed reduced arm swing and unaltered postural reflexes.
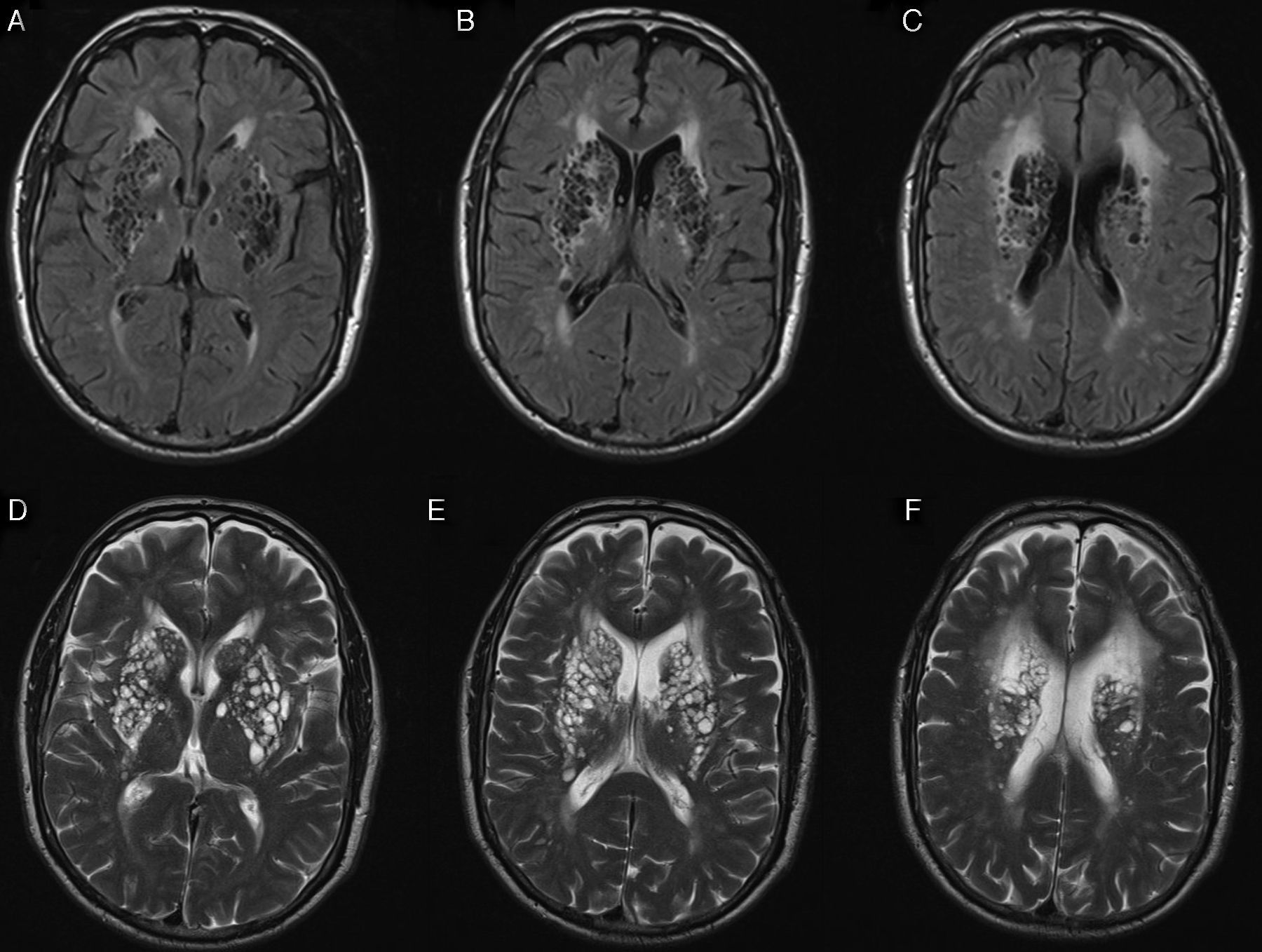
The laboratory analysis included a complete blood count, a biochemical study, a total protein test, vitamin screening, autoimmunity study (ANA, ANCA), and serological tests (HIV, Borrelia, Brucella, syphilis). All tests yielded normal results except for HDL levels (34mg/dL). Copper and ceruloplasmin levels were within normal limits. We conducted the following neuroimaging studies: (1) Brain MRI and MR angiography of the supraaortic trunks. We found dilation of VRS in the basal ganglia and both internal capsules (Fig. 1), periventricular leukoencephalopathy predominantly in the frontoparietal region bilaterally, and no alterations in the assessed cerebral vessels or the circle of Willis. (2) DaTSCAN. The patient displayed intense dopaminergic deficit bilaterally with moderate non-specific uptake.
We considered starting levodopa, but given our patient's psychiatric symptoms (behaviour and impulse control disorders) and mild motor dysfunction, we decided to delay treatment onset.
VRS may appear in up to 75% of all adult patients at any age; however, they are thought to become more frequent as age increases.2,3
They usually present in groups and in 3 typical locations: (1) surrounding the lenticulostriate arteries in the basal ganglia (type I; this is the most common location in cases with large dilations); (2) in the perforating arteries of the corona radiata and semioval centres (type II); and (3) in the brainstem (type III).1,2,4,5 VRS have been linked to alterations in the surrounding white matter, which in turn are associated with reactive gliosis.6
In many cases, VRS are incidental findings in neuroimaging studies; however, depending on their size and location, they are thought to be responsible for numerous symptoms including headache, parkinsonism, dizziness, memory impairment, instability, and seizures.5,6
We hypothesise that the parkinsonian symptoms and altered higher functions in our patient may be linked to VRS. One plausible explanation is that changes in the adjacent parenchyma secondary to major bilateral dilation of these spaces may be involved; they would alter cortical-subcortical connections and involve the corticostriatal fibres, thereby contributing to cognitive impairment and parkinsonism, respectively. In view of the DaTSCAN findings, we cannot rule out such other disorders as Parkinson's disease or Lewy body dementia which are associated with dilated VRS; these spaces may have contributed to an earlier onset of the symptoms of these disorders. Another possibility is vascular parkinsonism, which gives rise to structural lesions that may also alter DaTSCAN images.
Some authors suggest that perivascular spaces, regardless of their characteristics, are asymptomatic and constitute a merely casual finding.7
Only isolated descriptions appear in the literature, which makes it difficult to determine the pathophysiology of VRS and whether they are associated with certain clinical presentations.8–11