Chemical labyrinthectomy with gentamicin (CLG) is a minimally-invasive outpatient procedure aiming to achieve high concentrations of the drug in the cochlea with very little systemic dissemination. It is a useful treatment alternative in those patients with Meniere disease (MD) who do not respond to conventional medical treatment. Although vestibular toxicity secondary to CLG is a known adverse effect, visual alterations are rare; there are only 3 published cases of binocular vertical diplopia (BVD) with skew deviation (SD) due to this treatment. We present the fourth case of this complication, a patient with MD who developed BVD after undergoing an initial session of CLG.
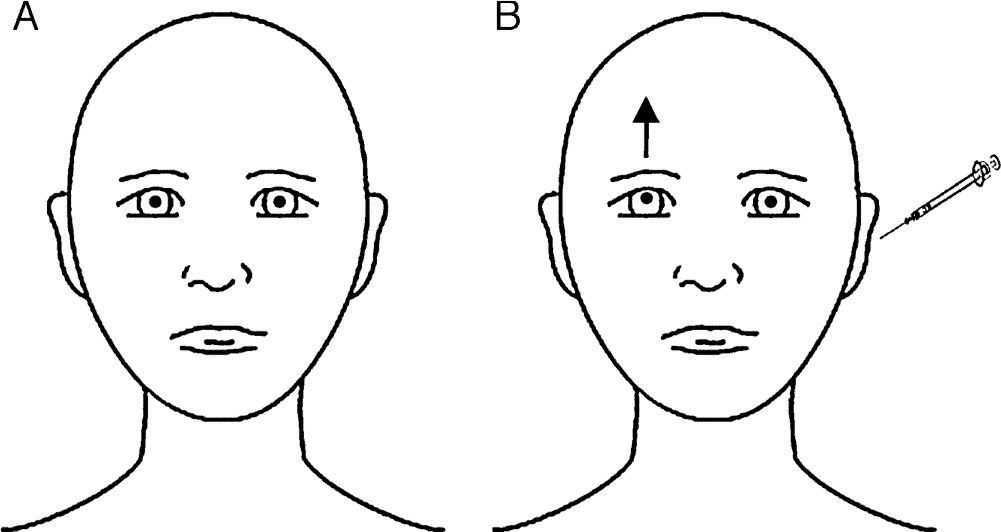
Our patient was a 79-year-old woman with a 2-year history of drug-resistant MD in the left ear. She had received an intratympanic gentamicin injection one week previously (30mg/mL; 0.5mL). Before receiving the second dose, she reported a 5-day history of gradually progressing symptoms of BVD. In view of the patient's symptoms, her otorhinolaryngologist ordered an urgent neuro-ophthalmologic assessment. The study of extraocular movements revealed right hypertropia with 3 prism dioptres in all eye positions (Fig. 1). All other tests (visual acuity, pupillary light reflex, confrontation visual field exam, saccades and smooth pursuit eye movements, Bielschowsky head-tilting test, Ishihara test, and fundus observation with slit-lamp) yielded normal results. The patient was taking her usual medication, and her vital signs, cognitive state, and clinical examination results were all normal. Despite the above, she was admitted to the neurology department due to possible CNS involvement. Analyses and a brain MRI study did not reveal any relevant results. She was finally discharged and instructed to continue with the treatment she had received during her hospital stay: alternating an eye patch every day and using prisms. After 8 weeks of follow-up by the neurology and ophthalmology departments, BVD disappeared, confirming the diagnosis of SD due to CLG.
Ocular findings in our patient with her eyes in the primary position, before (A) and immediately after (B) intratympanic gentamicin injection. At baseline, eyes were in their neutral position. After CLG, the patient experienced upward deviation of the visual axis of the right eye, whereas the left eye remained unaltered; called hypertropia, this misalignment of the eyes is present in SD and eventually leads to BVD. Skew deviation is usually caused by supranuclear alterations in the brainstem or the cerebellum. It affects vertical vestibulo-ocular tracts or, at times, the vestibular nerve or vestibular terminal organ (organ of Corti). SD is usually comitant; when incomitant, it may mimic partial paralysis of the third or fourth cranial nerves. The cause is usually vascular ischaemia in the pons or the lateral medulla oblongata (Wallenberg syndrome), probably due to involvement of the vestibular nuclei or their projections. When damage is located in the inferior area of the pons (as in our patient), the ipsilateral eye is undermost (ipsiversive SD), whereas in the case of rostral lesions at the level of the pons, the undermost eye is the contralateral eye (contraversive SD).1–3
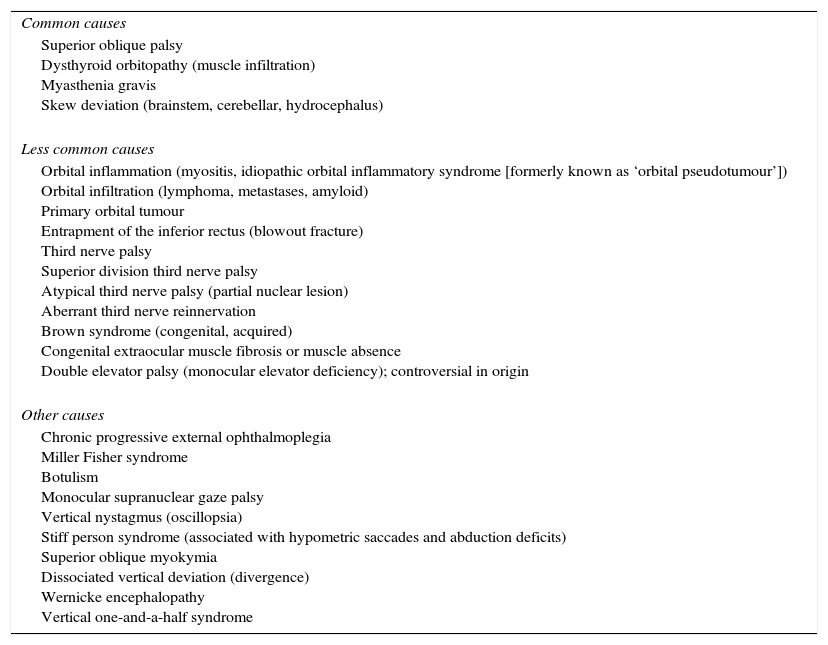
Binocular visual diplopia is a medical emergency that requires immediate neuro-ophthalmologic assessment. SD is considered one of the most frequent causes of BVD (Table 1) as well as the semiological manifestation of damage at the level of the cerebellum or brainstem. However, this clinical manifestation may also be observed in the immediate and late postoperative periods following surgery for unilateral peripheral vestibular disorders.1–5 In addition, MD is a chronic disorder of the inner ear that manifests with vertigo, tinnitus, ear fullness, and fluctuating hypoacusia. Today, CLG has replaced other invasive treatment options for MD. This treatment destroys the glycocalyx and stops endolymph production.4–8 Although numerous studies on CLG have been conducted, there is no consensus on dosing schedules. Weekly dosing plus follow-up hearing tests is an increasingly common approach. Although relatively safe, CLG is also associated with a number of complications, including instability, exacerbation of vertigo, and worsening of hearing impairment. There are also several published cases of ataxia accompanied by oscillopsia, which may be due to the CNS being unable to compensate fully for vestibular suppression secondary to CLG.4–9 SD, on the other hand, is a vertical misalignment of the eyes due to damage to prenuclear vestibular inputs to the ocular motor nuclei. The most recent hypotheses suggest that SD linked to CLG is caused by asymmetrical, unilateral damage to the utricle at the level of neural integration for vertical eye movements in the midbrain (those involving oculomotor neurons and the interstitial nucleus of Cajal).5,8,9 Delayed onset of SD after CLG is due to the pharmacodynamic properties of intracochlear gentamicin. After gentamicin is injected into the middle ear, the drug concentration in the inner ear peaks in about the first 16hours and gradually decreases during the following 16 to 24hours. Toxicity affecting vestibular ciliated cells is likely to accumulate during a similar period of time, and SD occurs when vestibular denervation reaches a critical level.6–8 Fortunately, this condition usually resolves within 6 to 8 weeks.8 Lastly, the recently developed video Head Impulse Test (vHIT) is a valuable complementary tool for identifying vestibular deficits and preventing iatrogenic effects.10,11 In conclusion, development of BVD secondary to CLG has previously been reported in 2 articles published in otorhinolaryngology journals,8,9 but never in a neurological journal. This entity is probably underdiagnosed. Our case shows that CLG may cause reversible BVD. This statement is supported by the Naranjo algorithm for adverse drug reactions: our patient scored 7 out of 13 points, which suggests that CLG was the most likely cause of BVD.12 Clinicians should therefore be on the lookout for this rare adverse drug reaction; it may resemble CNS damage and treating it requires an interdisciplinary approach. It is still to be determined if CLG has a more extensive biochemical effect on the CNS. Prospective studies describing more cases should be conducted for a better understanding of this entity.
Causes of binocular vertical diplopia.
| Common causes |
| Superior oblique palsy Dysthyroid orbitopathy (muscle infiltration) Myasthenia gravis Skew deviation (brainstem, cerebellar, hydrocephalus) |
| Less common causes |
| Orbital inflammation (myositis, idiopathic orbital inflammatory syndrome [formerly known as ‘orbital pseudotumour’]) Orbital infiltration (lymphoma, metastases, amyloid) Primary orbital tumour Entrapment of the inferior rectus (blowout fracture) Third nerve palsy Superior division third nerve palsy Atypical third nerve palsy (partial nuclear lesion) Aberrant third nerve reinnervation Brown syndrome (congenital, acquired) Congenital extraocular muscle fibrosis or muscle absence Double elevator palsy (monocular elevator deficiency); controversial in origin |
| Other causes |
| Chronic progressive external ophthalmoplegia Miller Fisher syndrome Botulism Monocular supranuclear gaze palsy Vertical nystagmus (oscillopsia) Stiff person syndrome (associated with hypometric saccades and abduction deficits) Superior oblique myokymia Dissociated vertical deviation (divergence) Wernicke encephalopathy Vertical one-and-a-half syndrome |
The authors have no conflicts of interest to declare.
We would like to thank Drs. Victoria Galán Sánchez-Seco, José Tejeiro Martínez, Francisco Cabrera Valdivia, María Molina Sánchez, and María Henedina Torregrosa Martínez.
Please cite this article as: León Ruiz M, Izquierdo Esteban L, Parra Santiago A, Benito-León J, Nieto Altuzarra AE, García-Albea Ristol E. Diplopía vertical binocular tras laberintectomía química con gentamicina. A propósito de un caso y revisión de la literatura. Neurología. 2016;31:503–505.