Convexity subarachnoid haemorrhage (cSAH) is an infrequent form of non-traumatic and non-aneurysmal subarachnoid haemorrhage. Several causes of these haemorrhages have been proposed, including cortical vein thrombosis, vascular malformations, posterior reversible leukoencephalopathy syndrome, vasculitis, amyloid angiopathy, and reversible cerebral vasoconstriction syndrome.1–3
Cases have been described of bilateral carotid artery stenosis associated with cSAH,4 and even a case associated with occlusion of the ipsilateral internal carotid artery (ICA).5
We present 3 cases of cSAH associated with ICA occlusion.
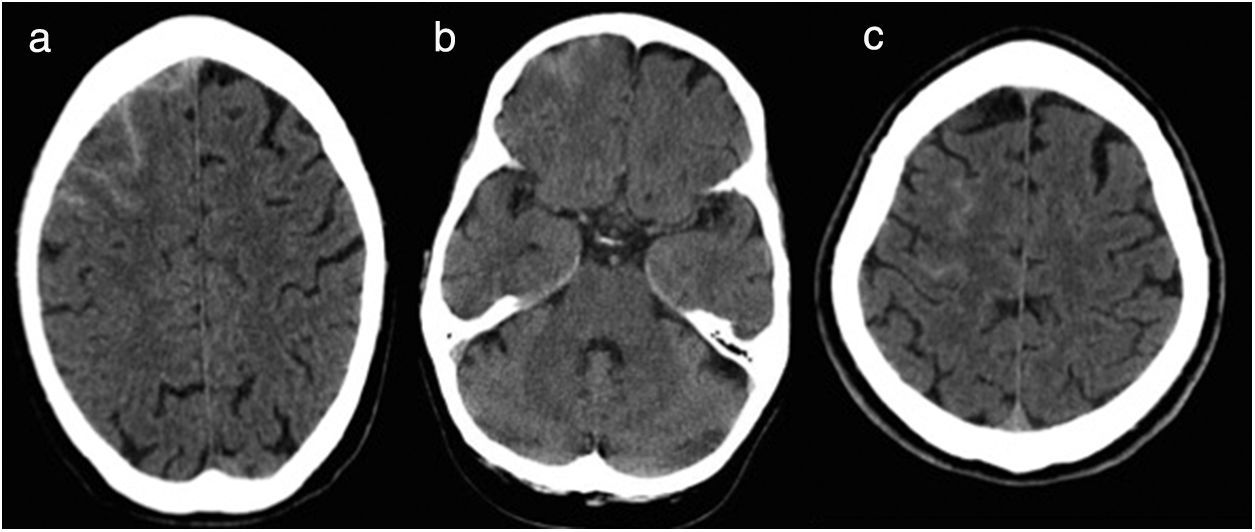
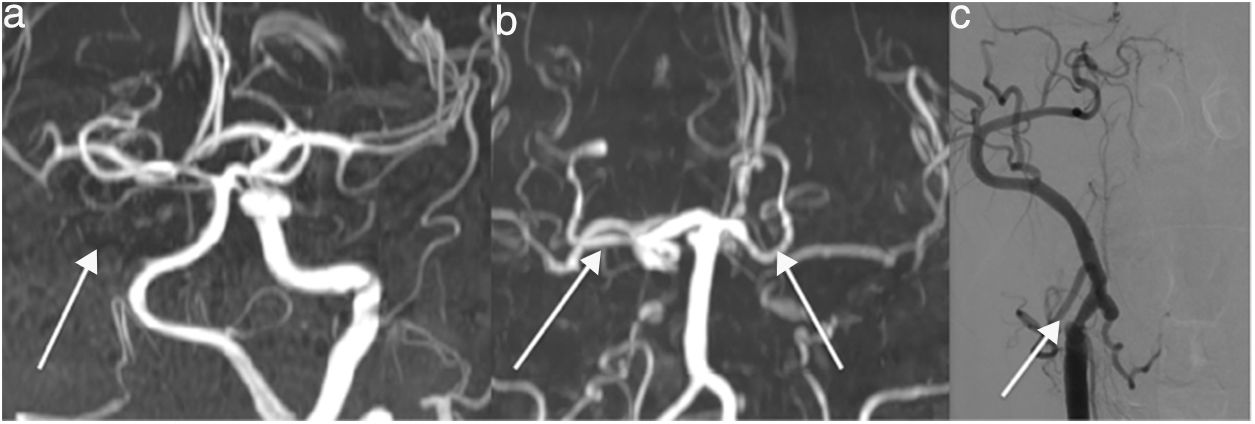
Patient 1 is a 79-year-old man with history of non-valvular atrial fibrillation with no antithrombotic treatment who was attended due to a 2-minute episode of amaurosis fugax of the right eye. He presented no history of head trauma, headache, or ingestion of toxic substances. The neurological examination yielded normal results and no neck rigidity or meningeal signs were observed. Head computed tomography (CT) (Fig. 1A) and brain magnetic resonance imaging (MRI) scans showed right frontal cortical haemorrhage with no signs of underlying ischaemic lesions. Neuroimaging studies did not reveal microbleeds, venous thrombosis, or dissection of the ICA. A Doppler ultrasonography of the supra-aortic trunks showed complete occlusion of the right common carotid artery; this was confirmed by MR angiography of the supra-aortic trunks (Fig. 2b)
Patient 2 is a 63-year-old woman with history of arterial hypertension, dyslipidaemia, and smoking (20 cigarettes/day) who was attended due to a sudden-onset episode of transient weakness of the left leg, which resolved within 15 minutes. She presented no history of headache or head trauma. A head CT scan (Fig. 1B) and brain MRI study showed a right frontal cortical subarachnoid haemorrhage. The neurological examination yielded normal findings, with no signs of neck rigidity. A Doppler ultrasonography and MR angiography of the supra-aortic trunks showed bilateral occlusion of the internal carotid artery. The study revealed no other remarkable results.
Patient 3 is a 60-year-old man with history of arterial hypertension, type 2 diabetes mellitus, dyslipidaemia, and smoking (30 cigarettes/day). He was attended due to an episode of dysarthria and weakness of the arm, resolving within 10 minutes, with no associated headache. Upon arrival at the emergency department, the patient did not present neck rigidity or any other relevant sign. A CT scan showed right cSAH (Fig. 1C). A Doppler ultrasonography of the supra-aortic trunks revealed right carotid artery occlusion and critical stenosis of the left ICA, which was confirmed by an angiography study (Fig. 2C).
All 3 patients presented good clinical progress and symptoms fully resolved; they were discharged with antiplatelet and statin treatment and have presented no further episodes of neurological deficit. Follow-up head CT scans showed complete resolution of the SAH in all 3 patients.
Non-traumatic cSAH is an infrequent condition, and the most frequently reported causes in large patient series are cerebral vasoconstriction syndrome and amyloid angiopathy.2 Non-traumatic cSAH has been described in cases of moyamoya disease, intracranial stenosis,1 and some cases of ipsilateral carotid artery occlusion,4 which is a frequent cause, according to one series.3 However, it is an infrequent cause in most registries; for example, a Spanish registry of 1000 consecutive patients with cerebrovascular disease reports no case of cSAH associated with carotid artery occlusion.6
The pathophysiological mechanism of subarachnoid haemorrhage secondary to carotid artery occlusion may be related to haemodynamic alterations provoking the rupture of fragile, dilated cortical pial vessels as a compensatory mechanism.4,5,7
The cases described above demonstrate the usefulness of imaging studies of cervical and intracranial vessels (Doppler ultrasonography, CT angiography, MR angiography, or angiography) for diagnosing carotid artery stenosis and occlusion as a cause of cSAH, once imaging studies have ruled out other aetiologies.
Please cite this article as: Santamaria-Cadavid M, Rodiguez-Castro E, Lopez-Dequidt I, Arias-Rivas S. Hemorragia subaracnoidea de la convexidad asociada a oclusión carotídea ipsilateral. Neurología. 2020;35:538–540.