Vascular warning syndromes constitute a neurological emergency due to their associated high risk of established stroke. At present, there is no strong evidence indicating the best treatment for these patients. The aim of this paper is to describe the function of intravenous rt-PA thrombolysis in the treatment of vascular warning syndromes.
Material and methodsWe reviewed our hospital records and the literature to find patients with neurologically fluctuating profiles and who underwent intravenous rt-PA thrombolysis.
ResultsWe retrieved 3 cases from our hospital records and 19 from the literature (15 males and 7 females). Mean age was 68.7±9 years (range: 52 to 84 years). The mean number of episodes before treatment was 4 (range: 2 to 15 episodes). The maximum NIH stroke scale (NIHSS) scores ranged from 6 to 22 in different patients. We obtained 24-hour post-treatment NIHSS scores in 8 cases; of these cases, 6 (75%) had a score of 0, and the other 2 (25%) had a score of 12. The modified Rankin Score calculated at 3 months of treatment was 0 or 1 in 18 patients (81.8%); these 18 comprised 8 of the 10 patients with lacunar warning syndromes (80%), 6 of the 7 with basilar warning syndromes (85.7%), and 4 of the 5 with fluctuating non-lacunar, non-basilar warning syndromes (80%).
ConclusionsIntravenous rt-PA treatment may constitute an effective and safe therapeutic alternative for patients with neurovascular fluctuations. However, well-designed studies are needed to determine the role of intravenous rt-PA thrombolysis in cases of vascular warning syndrome.
Los síndromes de alarma vascular constituyen una situación de urgencia neurológica, debido a su alto riesgo de ictus establecido. Actualmente no existe evidencia firme sobre cuál debe ser el tratamiento de elección en estos casos. El objetivo de este trabajo es describir el papel de la trombólisis con rTPA intravenosa en el tratamiento de los síndromes de alarma vascular.
Material y métodosSe revisaron los casos propios y los existentes en la literatura en los que se hubiese tratado con rTPA intravenoso a los pacientes con clínica neurológica fluctuante.
ResultadosSe obtuvieron 3 casos propios y 19 recogidos de la literatura (15 varones y 7 mujeres). La edad media fue de 68,7±9 años (rango: 52-84 años). La frecuencia media de episodios antes del tratamiento fue de 4 (rango: 2-15 episodios). La puntuación en la escala NIH (NIHSS) máxima estuvo en un rango entre 6-22 según cada caso. Se dispuso de la NIHSS a las 24h del tratamiento en 8 de los casos: en 6 (75%) fue de 0, y en 2 (25%) de 12. La escala de Rankin modificada (ERm) a los 3 meses del tratamiento fue de 0-1 en 18 (81,8%) de los pacientes: 8/10 (80%) en los síndromes de alarma lacunar, 6/7 (85,7%) en los síndromes de alarma basilar y 4/5 (80%) en pacientes con fluctuaciones que no entraban dentro de estos 2 grupos.
ConclusionesEl tratamiento con rTPA intravenoso podría suponer una alternativa terapéutica eficaz y segura en los pacientes con clínica neurovascular fluctuante, aunque se necesitan estudios bien diseñados que establezcan de forma clara cuál es el papel real de la trombólisis intravenosa con rTPA en los síndromes de alarma vascular.
The presence of repetitive fluctuations during the acute phase of stroke has classically been associated with a high risk of recurrence and established stroke. In 1993 Donnan defined capsular warning syndrome (CWS) as repeated bursts of self-limiting motor deficit, or less frequently, sensory episodes that usually manifest as transient ischaemic attack with clinical signs of lacunar stroke.1,2 The most common lacunar syndrome is pure motor hemiparesis, in which lesions are most typically found in the internal capsule and pons. Later studies have described cases with a fluctuating course as in CWS but with established stroke localised in the pons. The term ‘pontine warning syndrome’ was coined for these cases.2–4 CWS is an uncommon entity which accounts for approximately 1.5% of all transient ischaemic attacks.5 The term ‘basilar warning syndrome’ was recently proposed to refer to those cases with a fluctuating clinical course indicating vascular involvement of the basilar artery and signalling the possibility of sudden occlusion.6 In general, all these terms indicate that such ‘warning syndromes’ must be considered neurological emergencies since they are accompanied by a high risk of established stroke, which is a life-threatening condition. In one recent study, Paul et al. determined that the risk of established stroke in the first 7 days after a CWS is 60%.5
The aim of this study is to describe our experience using intravenous thrombolysis with recombinant tissue plasminogen activator (rt-PA) to treat patients with repeated neurological fluctuations. To do this, we have grouped the descriptions of ‘warning symptoms’ regardless of the localisation of the final stroke or affected vascular territory, designating them by their common feature of being vascular entities. As a result, this study uses the term ‘vascular warning syndrome’.
Material and methodsWe initially defined ‘vascular warning syndrome’ as the clinical manifestation of acute neurological fluctuations in which symptoms improve until resolving completely (or nearly completely), followed by an exacerbation of more than 4 points on the NIH stroke scale (NIHSS). The first condition was met when 2 or more fluctuations presented over a period of less than 6hours.
We prospectively gathered all cases treated with thrombolysis with intravenous rt-PA in our hospital and selected patients with vascular warning syndrome who had undergone that treatment.
We also reviewed published scientific literature by searching the PubMed database. The keywords used were,“intravenous thrombolysis” AND “capsular warning syndrome”, “intravenous thrombolysis” AND “pontine warning syndrome”, “intravenous thrombolysis” AND “lacunar warning syndrome”, “intravenous thrombolysis” AND “basilar warning syndrome”, “acute treatment” AND “capsular warning syndrome”, “acute treatment” AND “pontine warning syndrome”, “acute treatmen” AND “basilar warning syndrome”, “acute treatment” AND “lacunar warning syndrome”, “acute stroke”, “fluctuating stroke”, We revised related articles in all cases.
For all cases from our hospital record, we recorded the patient's sex, age, number of fluctuations, maximum score on the NIHSS, time before treatment onset, NIHSS score at 24hours of treatment onset, modified Rankin Scale (mRS) at 3 months of treatment, presence of established infarct in the baseline computed tomography (CT) scan at 24hours of treatment, and presence of haemorrhagic complications. The same variables were collected from the cases described in the literature if they were available.
Our hospital cases and those from the literature were classified into 3 groups according to the symptoms that presented: (1) lacunar warning symptoms, where clinical manifestation consists of repeated bursts of self-limiting motor and sensory deficit; (2) basilar warning syndromes, for cases with a fluctuating course indicating involvement of the basilar artery or its branches and the possibility of sudden occlusion; (3) warning syndromes not classifiable in the above groups.
ResultsWe obtained 3 cases from our hospital and 19 from the literature (15 men and 7 women). Mean age was 68.7±9 years (range, 52 – 84 years). Mean fluctuation frequency before treatment was 4 episodes (range, 2 – 15 episodes). Maximum NIHSS scores ranged from 6 to 22.
Data for the time interval between symptom onset and treatment onset were available in 5 cases, with a mean time of 171.25minutes (range, 150 – 225minutes). For cases 9 to 21, we did not have data regarding time for each patient, although in the original articles describing those 13 cases, mean time was 171minutes (range, 80 – 300minutes).7
The 3 cases from our hospital were admitted to the stroke unit. In these cases, blood pressure levels in the first 24hours ranged from 150 to 185mm Hg (systolic) and 85 to 100mm Hg (diastolic).
Of the 22 cases, 10 (45.5%) could be classified as lacunar warning syndrome, 7 (31.8%) as basilar warning syndrome, and 5 (22.7%) as warning syndromes not classifiable in the other groups.
NIHSS score at 24hours of treatment, available in 8 cases, was 0 in 6 cases (75%) and 12 in the remaining 2 cases (25%). Another case provided the NIHSS score at 8 days of treatment, which was 8.
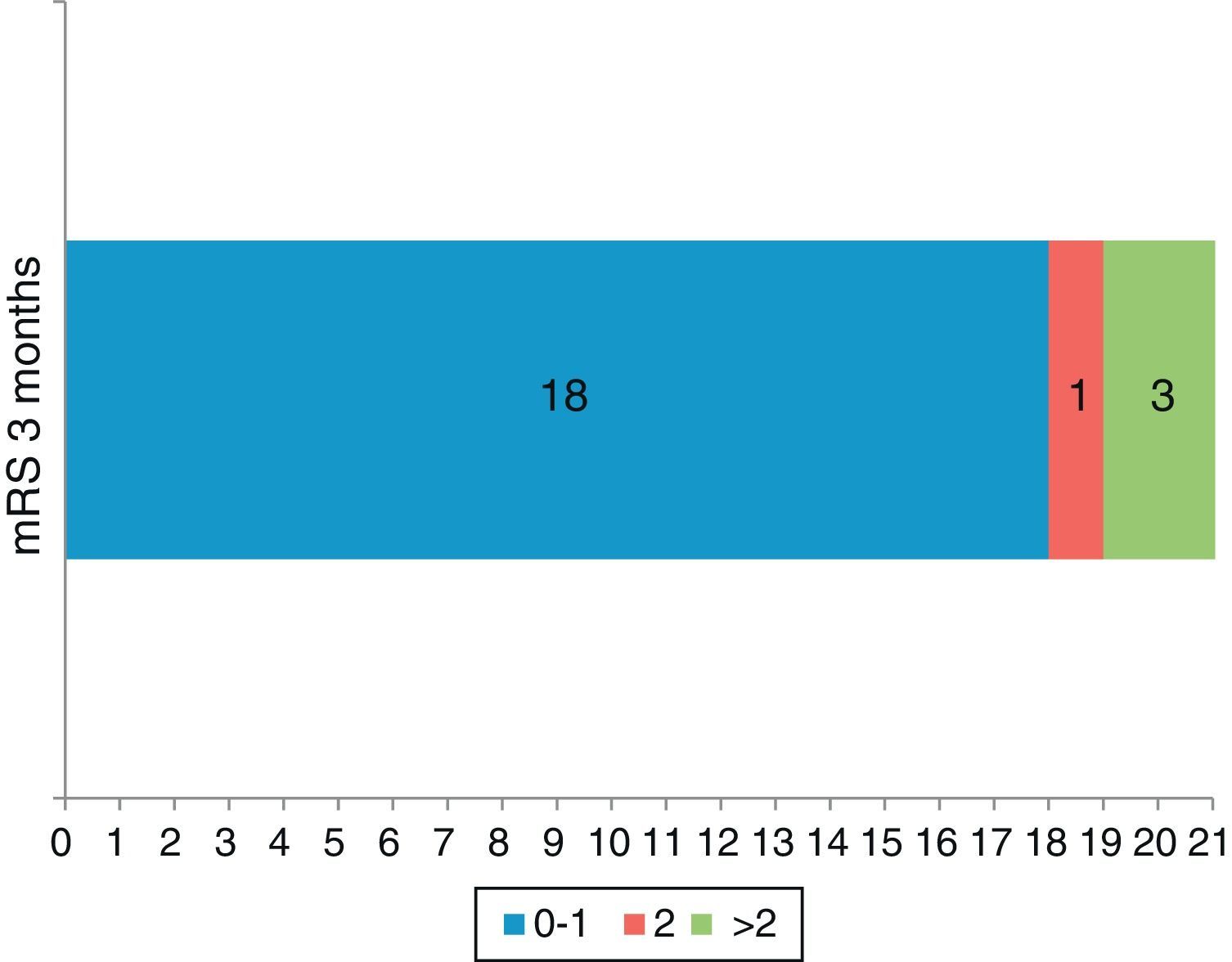
Modified RS at 3 months of treatment was 0 to 1 in 18 patients (81.8%) broken down as follows: 8/10 (80%) of patients with lacunar warning syndrome, 6/7 (85.7%) of patients with basilar warning syndrome and 4/5 (80%) of patients with fluctuations not classifiable in the above 2 groups. Modified RS score was 2 in one patient (4.5%) and mRS score at 3 months was not available in 3 cases. However, in those 3 patients, NIHSS score at 24hours was 12 in 2 cases; in the other case, measured at 8 days, NIHSS was 8 and mRS was 3. This entails a poorer functional prognosis at 3 months and these 3 patients were therefore considered dependent at 3 months of treatment for purposes of the analysis (Fig. 1).
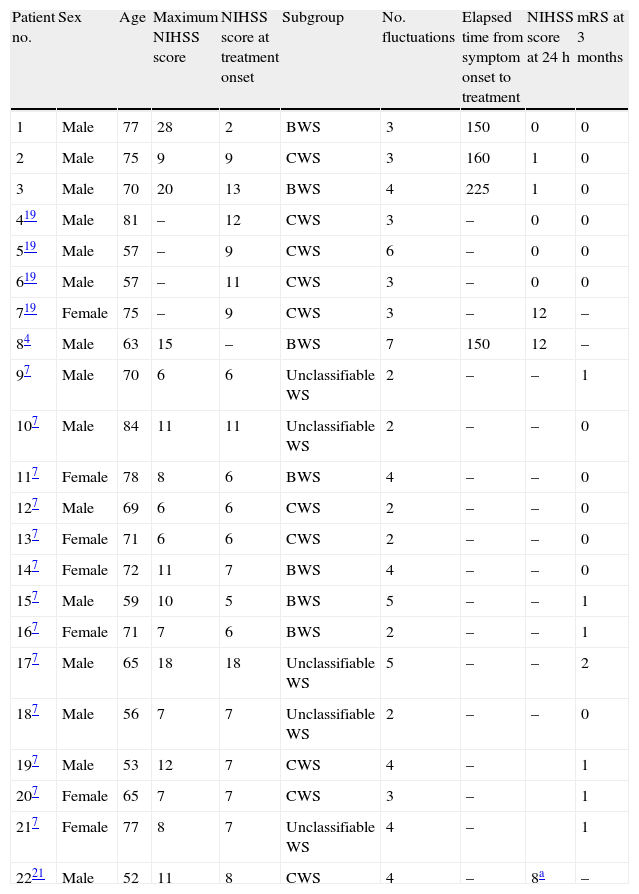
Table 1 details the clinical presentation and the outcome for the 21 cases.
Characteristics of patients included in the study.
| Patient no. | Sex | Age | Maximum NIHSS score | NIHSS score at treatment onset | Subgroup | No. fluctuations | Elapsed time from symptom onset to treatment | NIHSS score at 24h | mRS at 3 months |
| 1 | Male | 77 | 28 | 2 | BWS | 3 | 150 | 0 | 0 |
| 2 | Male | 75 | 9 | 9 | CWS | 3 | 160 | 1 | 0 |
| 3 | Male | 70 | 20 | 13 | BWS | 4 | 225 | 1 | 0 |
| 419 | Male | 81 | – | 12 | CWS | 3 | – | 0 | 0 |
| 519 | Male | 57 | – | 9 | CWS | 6 | – | 0 | 0 |
| 619 | Male | 57 | – | 11 | CWS | 3 | – | 0 | 0 |
| 719 | Female | 75 | – | 9 | CWS | 3 | – | 12 | – |
| 84 | Male | 63 | 15 | – | BWS | 7 | 150 | 12 | – |
| 97 | Male | 70 | 6 | 6 | Unclassifiable WS | 2 | – | – | 1 |
| 107 | Male | 84 | 11 | 11 | Unclassifiable WS | 2 | – | – | 0 |
| 117 | Female | 78 | 8 | 6 | BWS | 4 | – | – | 0 |
| 127 | Male | 69 | 6 | 6 | CWS | 2 | – | – | 0 |
| 137 | Female | 71 | 6 | 6 | CWS | 2 | – | – | 0 |
| 147 | Female | 72 | 11 | 7 | BWS | 4 | – | – | 0 |
| 157 | Male | 59 | 10 | 5 | BWS | 5 | – | – | 1 |
| 167 | Female | 71 | 7 | 6 | BWS | 2 | – | – | 1 |
| 177 | Male | 65 | 18 | 18 | Unclassifiable WS | 5 | – | – | 2 |
| 187 | Male | 56 | 7 | 7 | Unclassifiable WS | 2 | – | – | 0 |
| 197 | Male | 53 | 12 | 7 | CWS | 4 | – | 1 | |
| 207 | Female | 65 | 7 | 7 | CWS | 3 | – | 1 | |
| 217 | Female | 77 | 8 | 7 | Unclassifiable WS | 4 | – | 1 | |
| 2221 | Male | 52 | 11 | 8 | CWS | 4 | – | 8a | – |
No haemorrhagic complications were observed in any of the patients from our hospital or from the literature search.
DiscussionManagement during the acute phase of ‘vascular warning syndromes’ remains controversial. In these cases, blood pressure control is vital to avoid hypoperfusion of the distal branches of the perforating arteries.8 In our 3 cases, patients were admitted to the stroke unit, where their blood pressure control was monitored strictly. Blood pressure remained within the range accepted for treatment of acute ischaemic stroke. One of the most common measures applied in daily practice is anticoagulation with sodium heparin to reduce risk of established motor deficit, but data are not sufficiently robust to support the efficacy of anticoagulants during the acute phase of CWS.1,2,9,10 There is anecdotal evidence of apparently good results from other alternatives, such as oral clopidogrel,11,12 but more data are needed to establish the true role of treatments in these cases.
Intravenous thrombolysis with rt-PA is currently the only thrombolytic treatment approved for stroke at less than 4.5hours from onset for patients who fulfil the established inclusion criteria and have no contraindications for that treatment. Furthermore, efficacy of thrombolysis with rt-PA has been demonstrated for all aetiological subtypes of ischaemic stroke.13 Intravenous rt-PA treatment for patients who experience clinical improvement remains a controversial subject. Up to 1/3 of patients who initially present a rapid recovery will later develop a neurological exacerbation.14,15 It has also been demonstrated that treatment with intravenous rt-PA is safe in patients who experience rapid improvement before treatment. This situation is associated with a positive outcome at discharge.16
Although this topic has long been a matter of debate, IV thrombolysis with rt-PA has been linked to good results in the different aetiological subtypes of stroke, including lacunar infarcts.17,18 Although lacunar infarcts are associated with lipohyalinosis, several mechanisms by which fibrinolysis with IV rt-PA could be an effective treatment for this type of stroke have been put forward. Firstly, up to 20% of lacunar syndromes might be due to infarcts of other aetiologies, which could favour the effectiveness of IV rt-PA. Furthermore, lacunar infarct may be due to distal intracranial stenosis, and thrombolysis with IV rt-PA can prevent unstable thrombotic lesions on intracranial plaque. Thirdly, IV thrombolysis with rt-PA can improve distal blood flow in spite of the lipohyalinosis mechanism. Several recent studies have described experiences using thrombolytic treatment with intravenous rt-PA in patients with fluctuations during the acute phase of ischaemic stroke6 and in patients with capsular and basilar syndromes.5,19–21 In our series, practically half of the cases corresponded to a lacunar warning syndrome. It was interesting to note, based on an analysis of our hospital cases and those from the literature, that intravenous thrombolysis with rt-PA has a favourable efficacy profile in cases that might be regarded as vascular warning syndromes. Nearly 82% of these patients achieve independence by 3 months. This situation, at least initially, is associated with few haemorrhagic complications, which could be explained by the absence of established infarct and the resulting lack of necrotic tissue. These safety and efficacy profiles remain if we perform separate analyses for ‘capsular warning symptoms’ (80%), ‘basilar warning syndromes’ (85.7%), and syndromes not classifiable in the other groups (80%).
It is obvious that not all cases of patients experiencing marked neurological fluctuations during the acute phase of ischaemic stroke present the same risk of established infarct. Nevertheless, we believe that the existence of several fluctuations within a short time period should keep us watchful, as this could be indicative of an unstable flow that might stop at any time. In these cases, intravenous thrombolysis can restore patency to a partially occluded artery, thereby re-establishing the optimal blood flow.
We acknowledge the limitations of these types of studies, which may present selection and positive outcome biases. However, we believe that the data obtained should be considered since they may point towards a safe and efficient treatment method in patients for whom the most appropriate treatment has yet to be established. On this basis, we believe it necessary to design appropriate studies that will provide reliable information about the true role of thrombolysis in vascular warning syndromes. Several published studies confirm that this is a potentially acute disease that may lead to poor functional outcomes in the medium and long term; developing a clear definition of the optimal treatment would therefore be very beneficial.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: González Hernández A, Fabre Pi Ó, Cabrera Naranjo F, López Veloso A.C. Trombólisis intravenosa con activador tisular del plasminógeno recombinante en los síndromes de alarma vascular. Neurología. 2014;29:334–338.