The artery of Percheron is a single thalamoperforating artery that supplies the bilateral medial thalami and also irrigates the midbrain to a greater or lesser extent.1 Occlusion of this variant artery is infrequent.2,3 We present 2 cases of occlusion of the artery of Percheron that resolved with endovascular treatment.
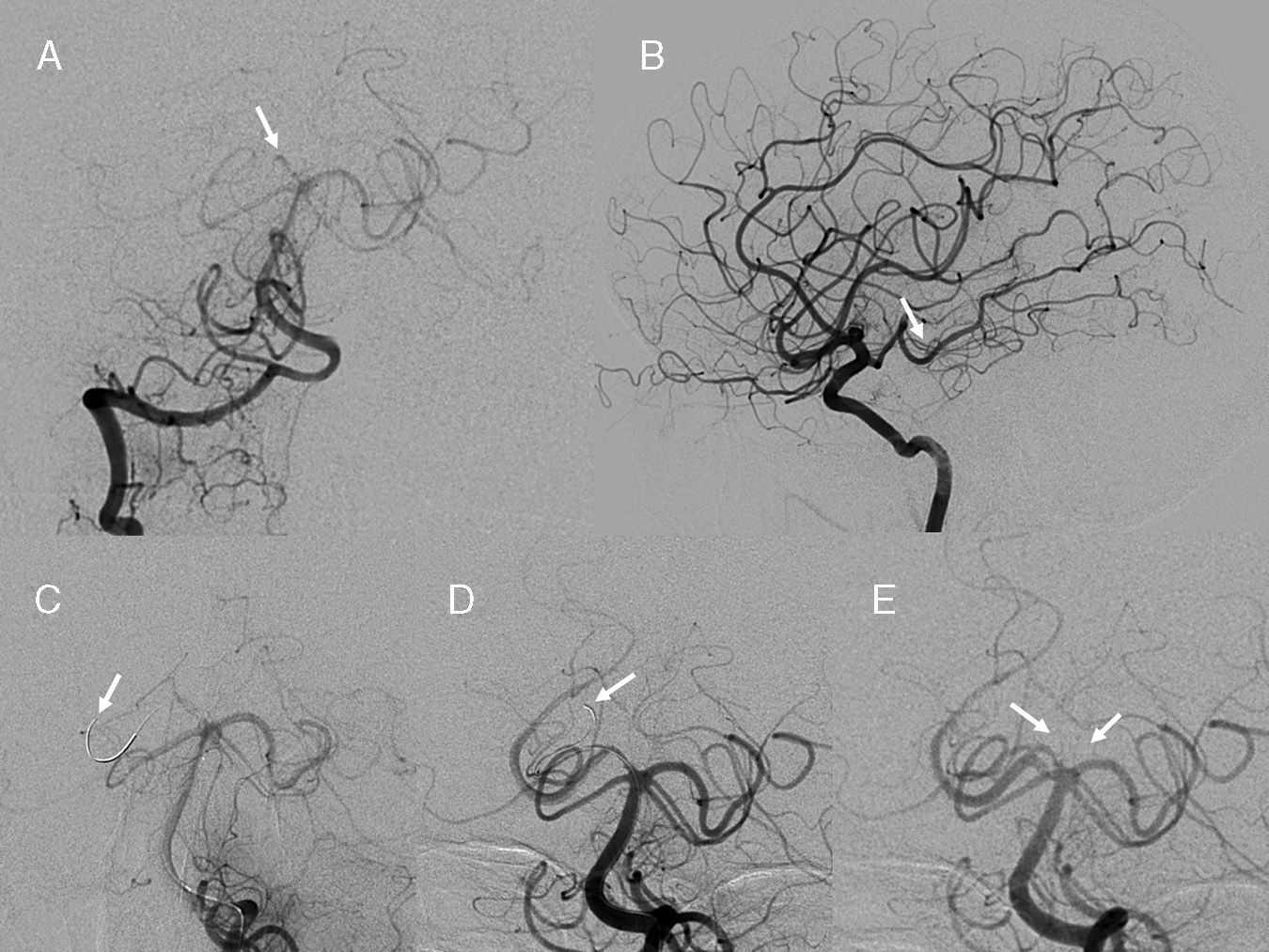
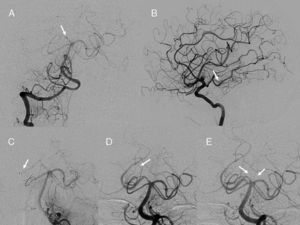
The first case was a 53-year-old man with a history of arterial hypertension, diabetes, high cholesterol levels, and obesity. During coronary catheterisation for acute myocardial infarction, he presented a decreased level of consciousness and conjugate gaze palsy. Examination revealed drowsiness, partial comprehension of commands, acute dysarthria, bilateral eyelid ptosis (more pronounced in the left eye), left-sided mydriasis with non-reactive pupil, and upgaze palsy. He was able to move his arms and legs normally. No loss of strength or lack of coordination was observed in the limbs. Computed tomography (CT) yielded no significant findings. Cerebral angiography revealed foetal origin of the right posterior cerebral artery and occlusion of the right P1 segment. A 0.10″ microguide wire was advanced as far as the right posterior cerebral artery (P2 and P3 segments) while mechanical disruption of the thrombus was being performed in the right P1 segment with a Gateway® balloon (Boston Scientific, Natick, MA, USA). The balloon measured 1.5mm×9mm and had been used previously for basilar artery angioplasty. The deflated balloon was passed through the occluded segment several times to achieve patency of the P1 segment and the single paramedian thalamic artery (artery of Percheron) (Fig. 1). Fibrinolytic treatment was not administered since the patient was anticoagulated with high doses of heparin for the cardiac catheterisation procedure. Since the calibre of the P1 segment was unknown, we did not inflate the balloon or use a stentriever device to avoid artery damage. Neurological examination after treatment showed ataxia and normal levels of consciousness. A follow-up brain CT yielded no significant findings. One week later, minimal bilateral eyelid ptosis, diplopia on upgaze, and ataxia persisted.
(A) Right vertebral artery prior to thrombolysis: right hypoplastic P1 segment with occlusion (arrow) is observed. (B) Lateral view of right carotid artery with adequate filling of the right posterior cerebral artery. (C) Microguide wire in the right posterior cerebral artery prior to balloon placement (arrow). (D) The end of the microguide wire was left in the posteromedial choroidal artery after several manoeuvres with the balloon deflated (arrow). (E) Both paramedian arteries have a common origin in the right P1 artery (arrows); recanalisation of the right P1 segment connected to the right posterior cerebral artery can be seen.
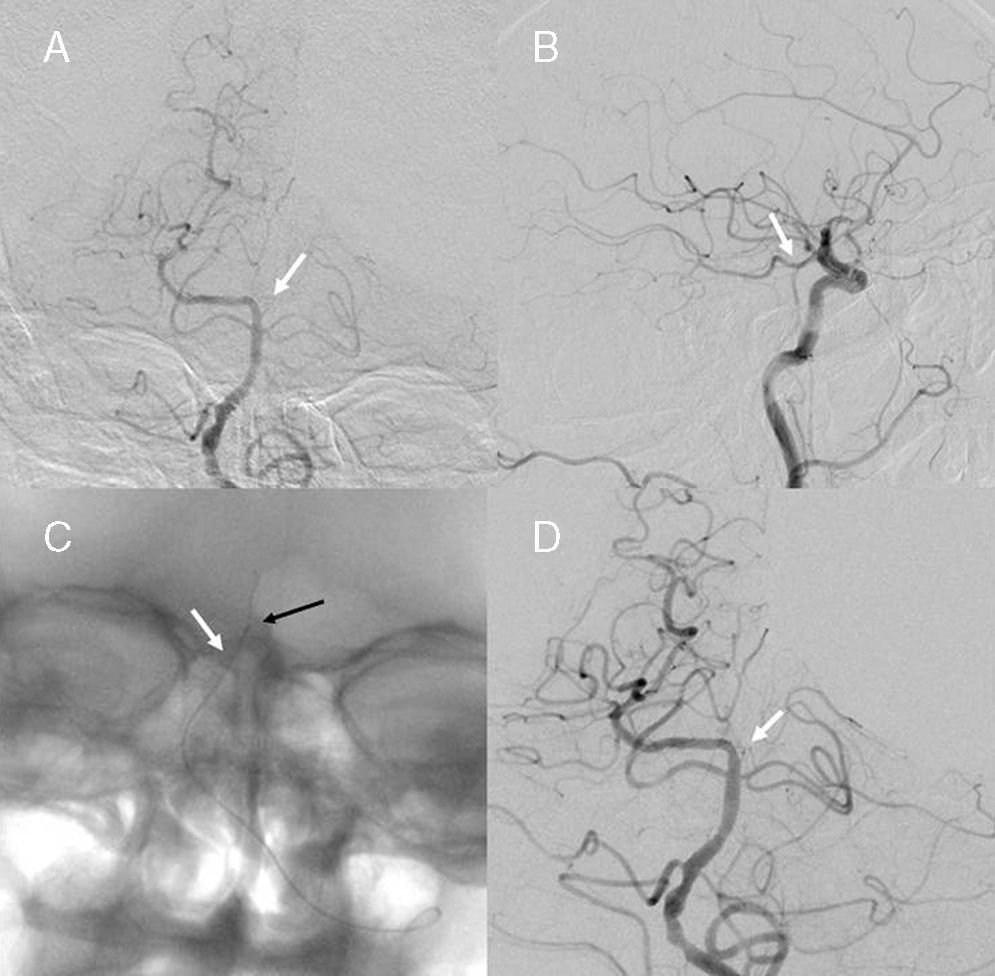
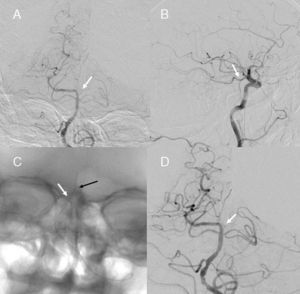
The second patient was an 81-year-old man with Meniere disease and convergent strabismus. Six hours before he was admitted, the patient presented dizziness similar to that occurring in Meniere disease, with drowsiness, lack of verbal response, and poor motor coordination of the right limbs. The patient was comatose and presented complex ophthalmoplegia with miosis at time of admission. Pain stimuli elicited flexion of the left limbs, whereas the right limbs showed no response. The patient displayed an extensor response to right-sided plantar stimulation (Babinski sign). Cranial CT yielded normal results; intravenous thrombolysis was not performed since first symptoms appeared 6hours before admission. Arteriography revealed foetal origin of the left posterior cerebral artery with left hypoplastic P1 segment which presented a filling defect. A Mirage® microguide wire measuring 0.08″ (ev3, Irvine, CA, USA) was passed through the P1 segment to break up the clot, but catheterisation was not possible. Consequently, 500000IU urokinase was administered at a rate of 10000IU/min at the origin of the P1 segment, resulting in patency of the P1 segment and of the artery of Percheron, which was detected after fibrinolysis treatment (Fig. 2). After the procedure, neurological examination (excluding gait) revealed a previously observed tendency of the eyes to converge, involuntary eye closure, and hypoacusia. Three days later, results from the neurological examination were normal. Brain MRI scans at 72hours yielded normal results.
(A) Left atherosclerotic vertebral artery with occlusion of the left P1 segment (arrow). (B) Filling defect on the left posterior cerebral artery from the left posterior communicating artery. (C) Microguide wire inside the left P1 segment (black arrow) and microcatheter inside basilar artery (white arrow). (D) Recanalisation of the left P1 segment with filling of the artery of Percheron (arrow).
The variant in which a single paramedian artery arises from a single P1 segment is called artery of Percheron.2 Occlusion of the artery of Percheron causes bilateral paramedian thalamic and rostal midbrain infarctions with a relatively symmetrical distribution.3,4 The classic triad of symptoms of bilateral infarction in this territory comprises altered level of consciousness, oculomotor symptoms, and neuropsychological symptoms. Eye movements are altered and the most characteristic neurological signs are partial/complete limitation of vertical gaze, loss of convergence, bilateral internuclear ophtalmoplegia, pseudopalsy of the abducens nerve, and intolerance to light.5–8 Pupils are frequently abnormal. Pupil size varies depending on involvement of the Edinger-Westphal nucleus or oculomotor fascicles, descending sympathetic fibres, or some combination of these structures.9,10 Likewise, thalamic regions related to memory may be affected.11 These bilateral thalamic lesions are often associated with midbrain lesions causing mesencephalothalamic or thalamopeduncular syndrome. Therefore, hemiplegia, cerebellar ataxia, or movement disorders may appear in addition to the classic symptoms. Theoretically, if the P1 segment of a posterior cerebral artery is absent, paramedian thalamic arteries should arise from the ipsilateral P1 segment and cross the midline.5,12 However, a P1 segment that cannot be visualised does not necessarily mean that the artery of Percheron arises from the ipsilateral P1 segment. This is demonstrated by our 2 cases. Diagnosis is frequently achieved several hours after symptom onset. At this stage, thrombolytic therapy is not effective.12,13 In our cases, intravenous treatment was contraindicated. The first patient had already received a high dose of heparin; the second patient's symptoms were still progressing more than 4.5hours after symptom onset. In conclusion, suspected infarction due to occlusion of the artery of Percheron should be considered if clinical symptoms are compatible. If intravenous thrombolysis cannot be performed, the intra-arterial pathway can be used. Absence of a P1 segment in an arteriography does not prove absence of a paramedian artery with foetal origin of the posterior cerebral artery and paramedian infarction caused by the occlusion of the artery of Percheron.
Please cite this article as: Jiménez Gómez E, Bravo Rey I, Ochoa-Sepúlveda JJ, Bravo-Rodríguez FdA. Ictus de territorio posterior. Tratamiento endovascular en pacientes con oclusión de la arteria de Percheron. Neurología. 2015;30:378–380.