Myokymias are localised involuntary contractions that are wavelike or vermicular and propagate through affected striated muscle.1–3 They are caused by simultaneous or sequential activations of 1, 2, or more motor units of a muscle. An electromyography reading shows spontaneous muscle activity with different motor units producing brief, repetitive discharges of action potentials in rhythmic or semi-rhythmic bursts. This is followed by a short (0.5 to 3seconds) and frequently irregular interval of electric silence before the following myokymic discharge occurs.4,5
When myokymia occurs in the face, the most frequently affected muscle is the orbicularis oculi. Myokymia in this muscle results in small, visible contractions of part of the eyelid, typically the lower eyelid. Eyelid myokymias (EM) tend to be transient and self-limiting within a few days of onset. They present in young, healthy subjects with no associated diseases.3,6,7 We describe a patient in whom the presence of continuous EM resulted in a diagnosis of multiple sclerosis (MS).
The patient was a 34-year-old woman with no relevant medical history or drug use. She was examined for abnormal movements compatible with myokymias in the right lower eyelid which had been occurring for 2 months. The symptoms initially presented sporadically during the day in episodes lasting from a few minutes to an hour. As the weeks passed, their frequency and intensity had increased and muscle twitches had become continuous. The first neurological examination revealed generalised hyperreflexia; all other findings were normal.
Given the intensity of the myokymias, the patient began treatment with carbamazepine (800mg/day), but the drug had to be discontinued quickly due to the appearance of a maculopapular rash and elevated transaminases.
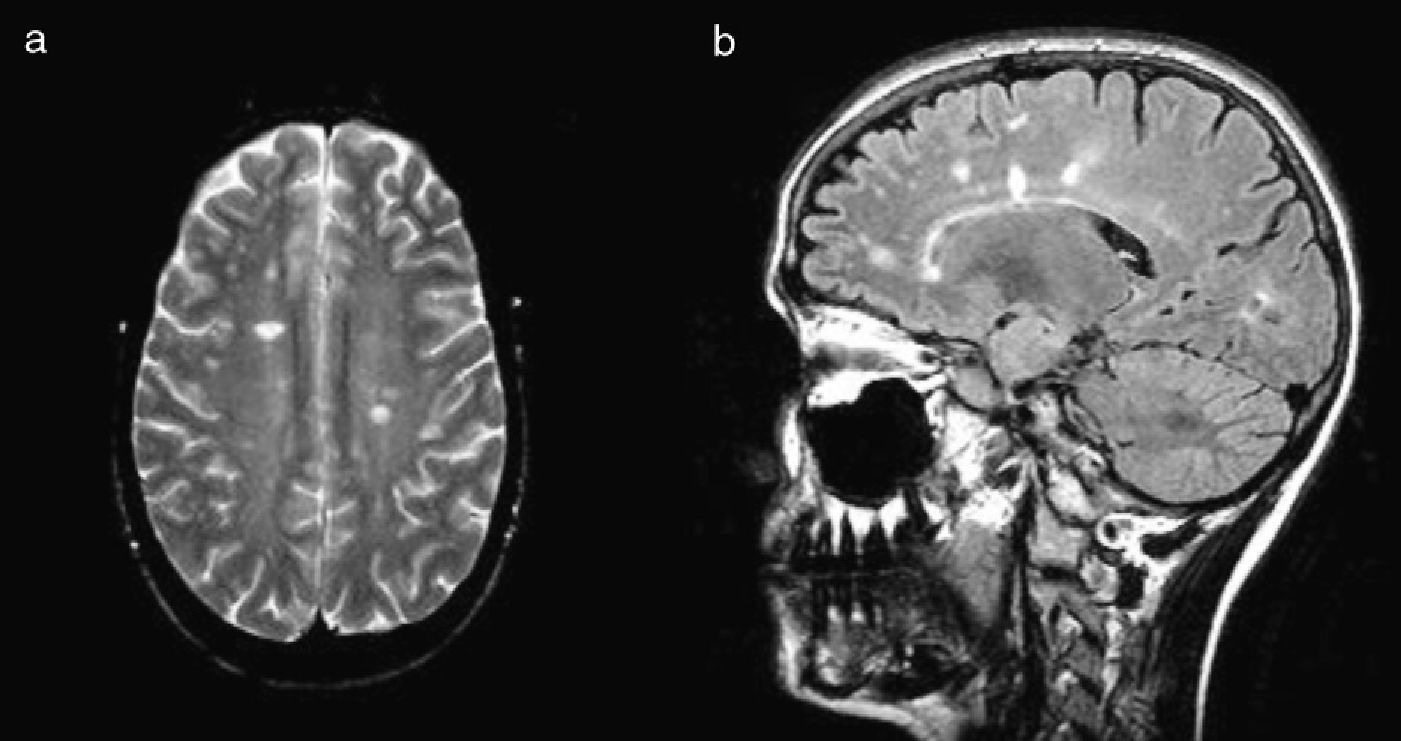
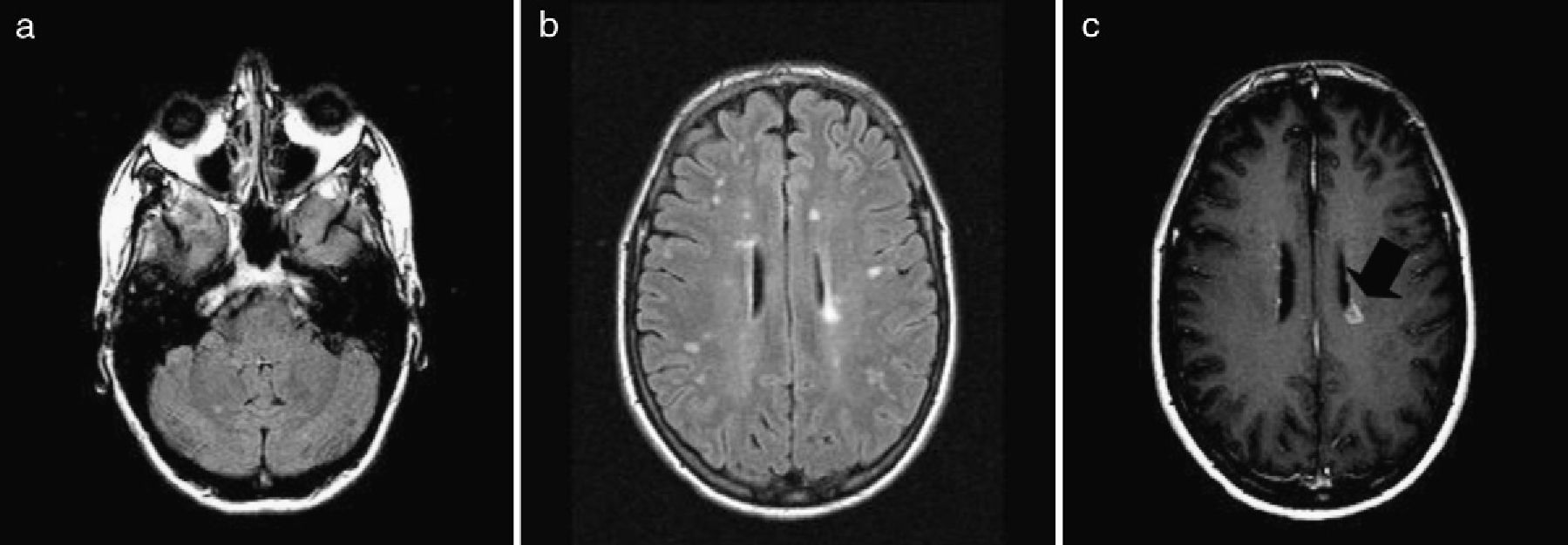
The symptoms resolved spontaneously 9 weeks after their onset. A week after EMs had become continuous, doctors performed a brain MRI which showed multiple lesions in supratentorial white matter in both hemispheres, semioval centres, and the juxtaventricular zone, plus a lesion in the posterior right frontal lobe (Fig. 1). A complete blood study including serology and autoimmune markers yielded normal results. CSF analysis indicated the presence of oligoclonal bands, although they were not found in serum. A second cranial MRI taken at 4 months revealed new lesions, including several with gadolinium uptake (Fig. 2). Based on these findings, the patient was diagnosed with MS.
Facial myokymias that occur continuously and affect all the muscles on one side of the face have often been described in association with different types of lesions of the ipsilateral pontine tegmentum,1–6,9 especially tumours (gliomas or metastasis),1,5 cysticercosis,8 and MS. In MS, myokymias may occur either throughout the duration of the disease2,9,10 or appear as its first symptom.6 Other entities with which EM is less frequently associated are subarachnoid haemorrhage,11 multiple system atrophy, and Guillain-Barré syndrome.2,3,5 In MS, facial myokymias tend to be self-limiting in the course of a few weeks (typically between 2 weeks and 6 months)5,10,12 and they rarely last as long as a year.9 However, myokymias secondary to malignant tumours typically last several years and resolve with treatment of the neoplasia.1,5,10
Unlike facial myokymias, those limited to the eyelid only tend to appear in healthy young subjects. They are associated with stress, fatigue, exercise, and excessive caffeine use.3,7,12 On rare occasions, they may be associated with underlying disease or extend to other facial muscles. In a typical presentation, they are unilateral and transient, appearing in episodes lasting a few minutes at a time over the course of a few days or weeks. It is very uncommon for EMs to appear continuously during periods spanning months, and they would still be considered benign even in such cases.3,7 However, available evidence is scarce. There is only 1 study evaluating persistent long-term EM,3 and this study found that only 1 of its study population of 15 developed clinically defined MS. It concluded that associations between long-term EM and other neurological diseases are uncommon. As we were unable to identify any of the trigger factors described for EM in our patient, and the condition persisted, we performed 2 cranial MRI scans and a lumber puncture which resulted in a diagnosis of MS.
Cranial MRI study of our patient was unable to show any lesions specific to the ipsilateral pons. Some cases of hemifacial myokymias are described in which cranial MRI scans did not show typical lesions in the pons.2,6,9 One possible reason is that the lesion causing facial myokymia in MS tends to resolve when clinical symptoms have stopped appearing.9 This was observed in a study that used cranial MRI to re-examine patients in whom typical lesions had previously been detected and whose symptoms had resolved. In 6 of the 8 patients, the lesions had disappeared within periods ranging from 1 week to 44 months.9 A cranial MRI was performed on our patient a week after her referral to our unit. Another possible mechanism could be hyperexcitability of the intra-axial part of facial nerve fibres due to possible functional deafferentation of inhibitory pathways of the facial nerve nucleus caused by demyelinating lesions on the supranuclear level.2,9,13 As a result, myokymias would not necessarily have to be caused by lesions in the pons.
In conclusion, we feel that while EM is a benign entity, it may be indicative of an underlying neurological disease, such as MS, if it persists over an extended period of time. We recommend conservative treatment for these patients at first, and elimination of known triggers such as caffeine, tobacco, and alcohol. If the EM continues, imaging studies should be completed in order to rule out any underlying lesions.