Our case concerns a 45-year-old smoker (10 pack/year) hospitalized with moderate respiratory distress (PaO2/FiO2 170mmHg), pleuritic pain, no fever and a three-week history of progressive shortness of breath and non-productive cough. He denied recent sick contacts, travels, inhalation exposures, reporting a history of Herpes Simplex Virus Type 2 (HSV-2) genital infection a year prior without other medical conditions. The patient had no history of high-risk sexual behavior or other sexually transmitted infections. He also reported no drug use and a weekly alcohol intake of approximately 12g.
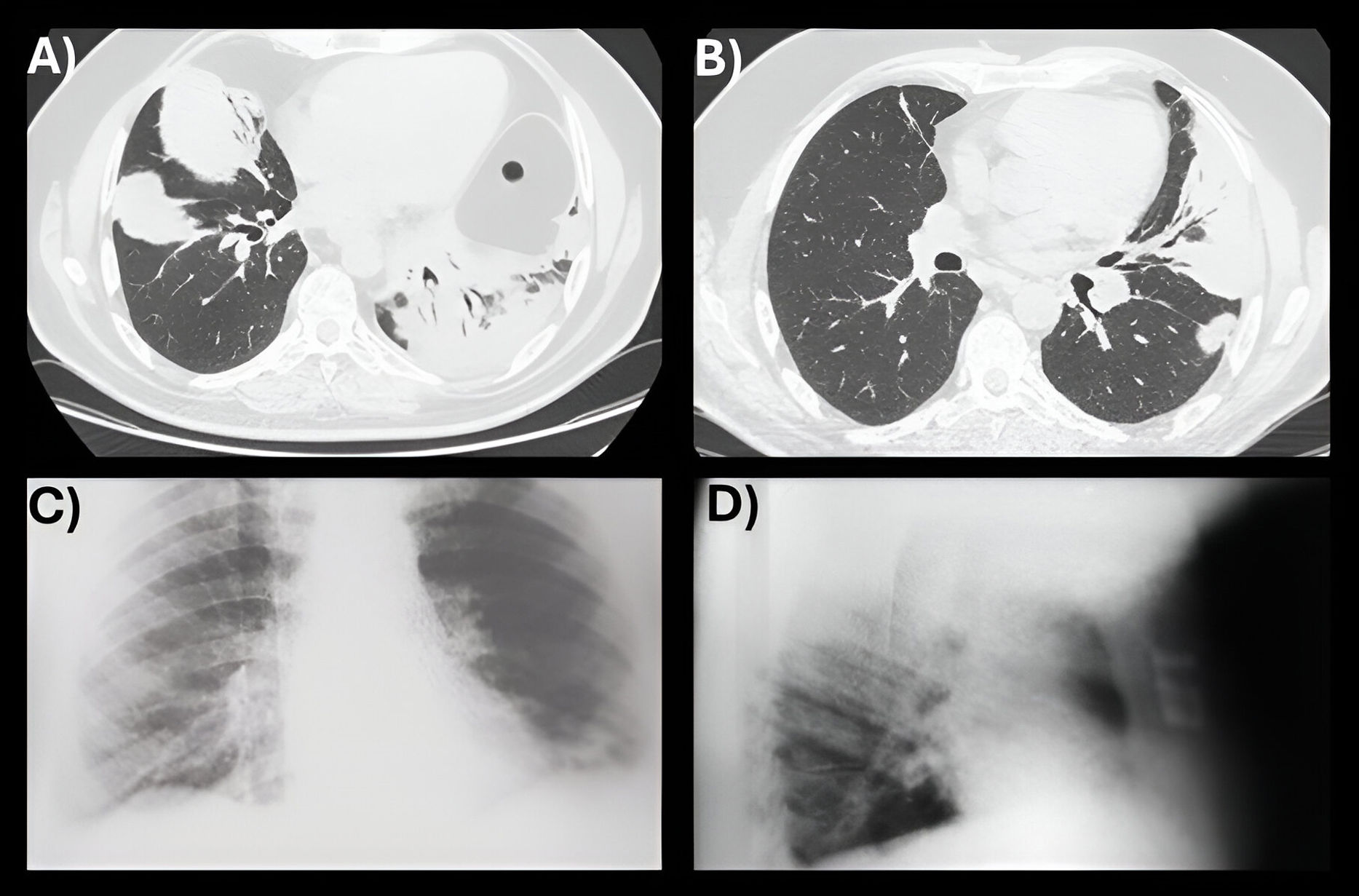
Chest computed tomography (CT) (Fig. 1A) revealed bilateral lung consolidations with a likely organizing pneumonia (OP) pattern. Serum C-reactive protein (CRP) was 14.4mg/dL. White blood cell (WBC) count was 19,700/μL with neutrophilia. Hemoglobin, coagulation parameters, serum biochemical tests, cryoglobulins, tumor markers, autoimmune antibodies, rheumatoid factor were within normal ranges. Serological tests for Hepatitis A Virus (HAV), Hepatitis B Virus (HBV), Hepatitis C Virus (HCV) and Human Immunodeficiency Virus (HIV); Legionella and pneumococcal urinary antigens; blood and sputum cultures were all negative.
(A) Chest CT at the time of admission showing bilateral, non-segmental airspace consolidation with bronchogram, consistent with OP. (B) Chest CT at 15 days follow-up showing bilateral reduction of consolidations after oral acyclovir and intravenous corticosteroids treatment. (C, D) Anteroposterior and lateral chest X-rays at 12 months follow-up demonstrating normal findings.
Amoxicillin–clavulanic and azithromycin were started without significant improvement. Bronchoalveolar lavage (BAL) cultures for fungi, bacteria, mycobacteria; multiplex respiratory Polymerase Chain Reaction (PCR) panel for Influenza Virus Types A and B, Respiratory Syncytial Virus (RSV), Human Metapneumovirus (hMPV), Adenovirus, Parainfluenza Virus (PIV), Rhinovirus/Enterovirus, Coronavirus, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), Human Bocavirus (HBoV), Human Parainfluenza Virus (HPIV), Human Coronavirus (HCoV), Herpes Simplex Virus Types 1 and 2 (HSV-1/2), Cytomegalovirus (CMV) and Mycoplasma pneumoniae; Aspergillus galactomannan, β-3-glucan returned negative results.
Transbronchial lung biopsy (TBLB) samples were insufficient for histological evaluation. BAL cytology excluded malignancy. BAL cell count indicated OP with a mixed pattern, showing lymphocytosis (35%), neutrophilia (10%), and CD4/CD8 of 0.8. Clinical conditions rapidly deteriorated (PaO2/FiO2 80mmHg), precluding TBLB repetition for histological confirmation.
Considering the history of HSV-2 infection, HSV-1/2 serology was performed despite the absence of genital lesions, revealing IgM titer of 1.3 and negative IgG (both negative if <0.9). We initiated oral acyclovir at 800mg twice daily for 10 days, resulting in clinical improvement (PaO2/FiO2 190mmHg), seroconversion to negative HSV-1/2 IgM and positive IgG titers (9.26). Subsequently, we commenced intravenous methylprednisolone at 40mg daily, yielding significant enhancement in clinical (PaO2/FiO2 332mmHg) and radiological findings (Fig. 1B). The patient was discharged on two-month-tapering course of oral prednisone, starting at 50mg daily, remaining recurrence-free for 12 months (Fig. 1C, D).
The organizing pneumonia (OP), characterized by intra-alveolar fibroblasts and collagen, is an inflammatory condition reversible with corticosteroids.1 OP has been anecdotally described as secondary immune response to diverse viral infections in immunocompromised hosts or those with severe comorbidities.2–4 Etiological hypotheses include prolonged viral shedding or T-cell immunity dysfunction.2,4 While histology is the diagnostic gold standard, BAL cell count, and radiology are crucial when TBLB results are inconclusive.1 HSV pneumonia is a rare, severe illness primarily affecting immunocompromised individuals, with a 1–5% incidence in patients with hematologic malignancies.5 The prevalence in the immunocompetent hospitalized population with severe respiratory illness round about 2%, often as a secondary colonizer rather than the primary pathogen, with approximatively 6 cases reported in literature.4,5 Diagnosis requires viral detection via PCR in BAL, the gold standard test.4
Based on anamnesis and serologic findings, we initiated acyclovir with rapid improvement, further enhanced by corticosteroids. Diagnosing subclinical HSV-2 reactivation via urethral swabs is difficult. PCR is highly sensitive (98%) and specific (97%), but due to intermittent viral shedding, a negative result doesn’t rule out the virus. Proper timing or serological assays are needed for confirmation.6 In our case serology assays were chosen as the initial, less invasive diagnostic approach.
On the other hands, a false negative in PCR for HSV from BAL is highly improbable, with the test showing a sensitivity typically ranging between 96% and 100% in various studies and 100% specificity.4,5 Initial recovery with antiviral therapy supported the diagnosis of OP secondary to extrapulmonary HSV subclinical activation,4,5 likely inducing a lung immune reaction.2,4,5 Acyclovir plausibly eliminated the immunological trigger.4,5 HSV pneumonia and OP can coexist, with few cases reported.4 However, to the best of our knowledge, no previous reports of OP secondary to asymptomatic HSV viral shedding have been documented. The case underscores the importance of considering OP as potentially related to extrapulmonary viral infections, even in atypical scenarios of comorbidity-free hosts, as shown by our findings. Supported by clinical-anamnestic data, it suggests incorporating viral serology as supplementary diagnostic tool for OP etiology.
Informed consentInformed consent was obtained for the publication of this paper.
FundingThere was not funding source for this study.
Authors’ contributionsAnna Michela Gaeta drafted the manuscript.
All authors critically reviewed and revised the manuscript draft for important intellectual content and approved the final version for submission.
Conflicts of interestThe authors declare that they have not conflict of interest.