To describe the epidemiology and CT findings for nontuberculous mycobacterial lung infections and outcomes depending on the treatment.
Material and methodsWe retrospectively studied 131 consecutive patients with positive cultures for nontuberculous mycobacteria between 2005 and 2016. We selected those who met the criteria for nontuberculous mycobacterial lung infection. We analysed the epidemiologic data; clinical, microbiological, and radiological findings; treatment; and outcome according to treatment.
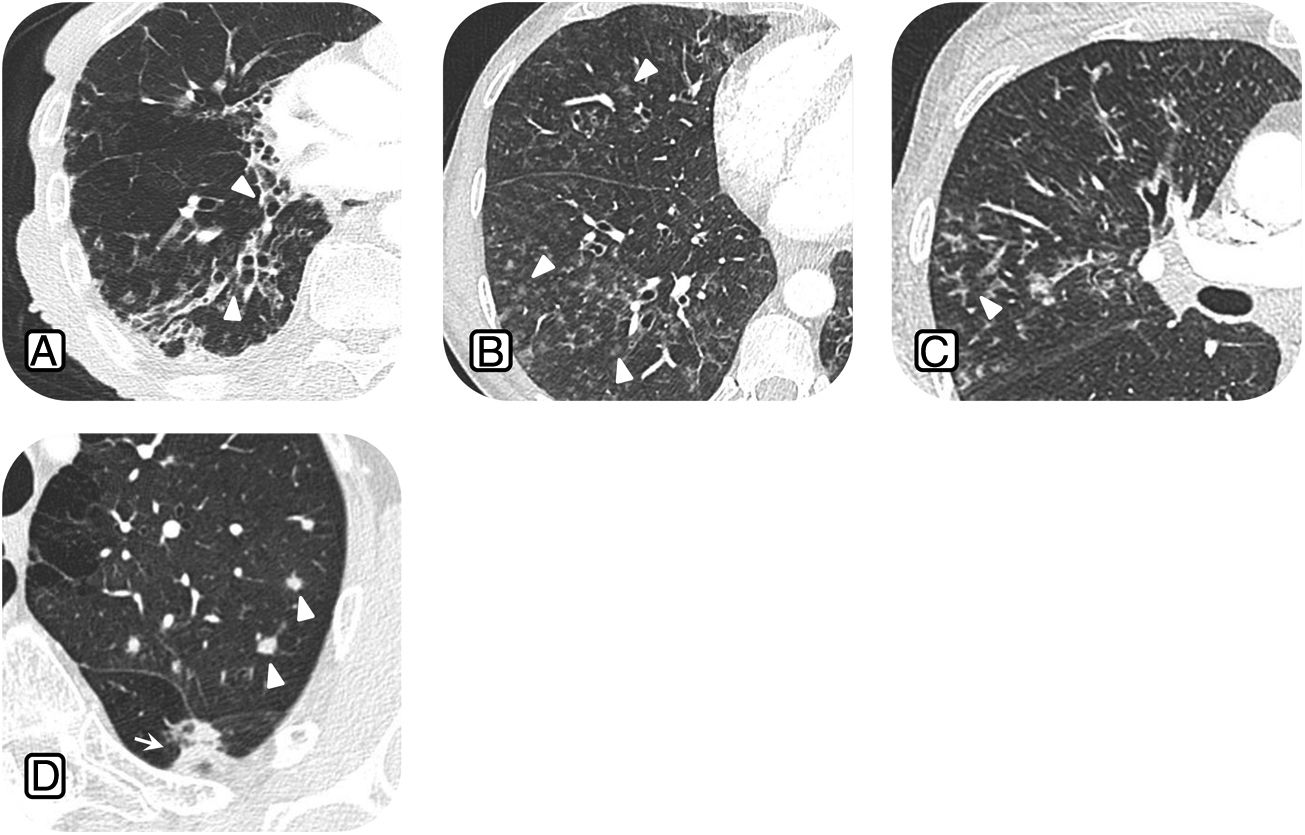
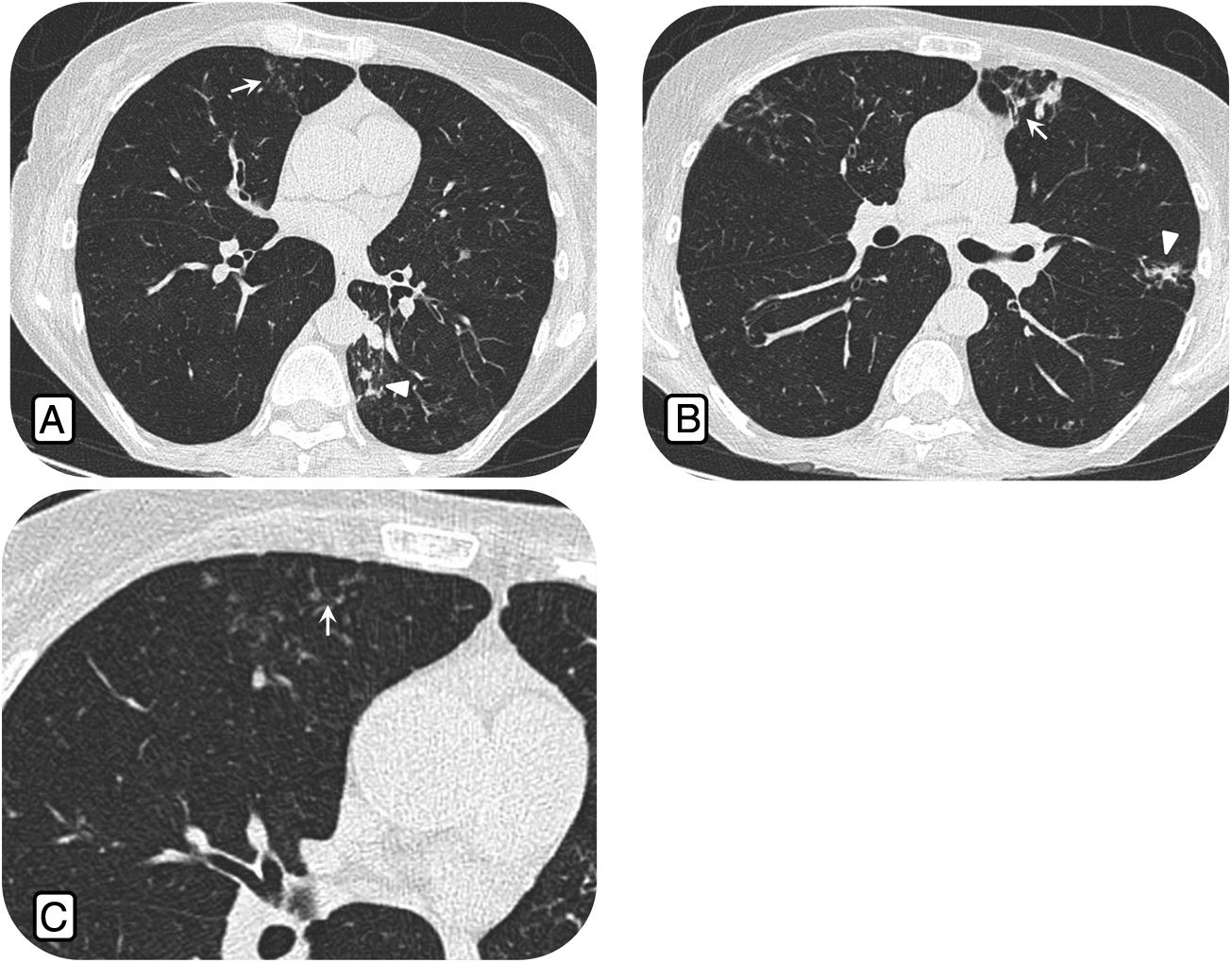
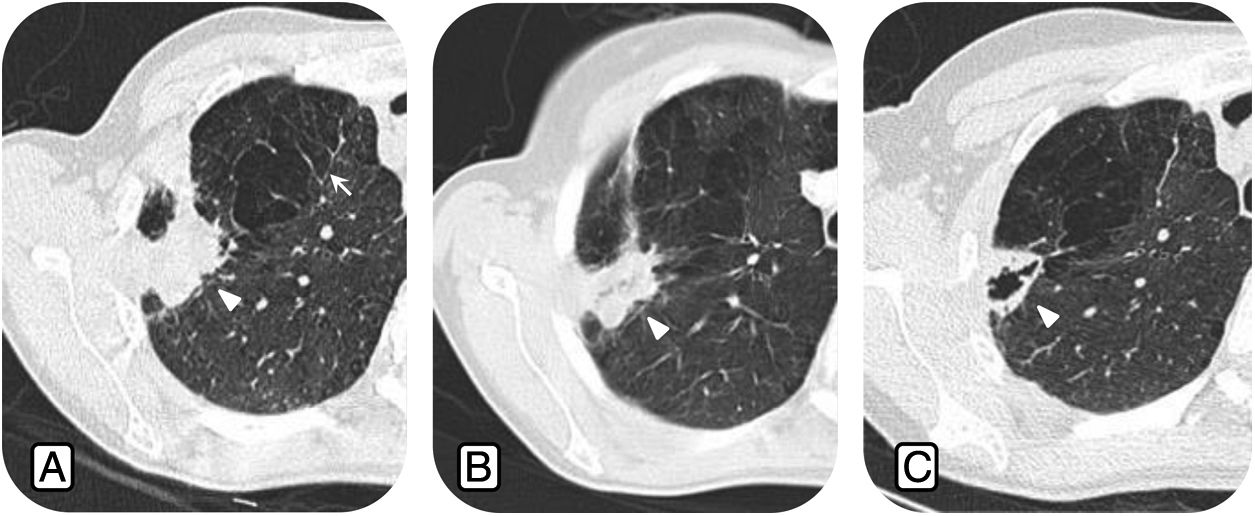
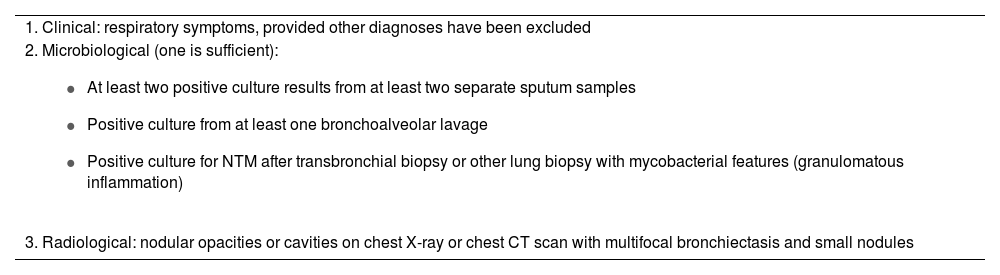
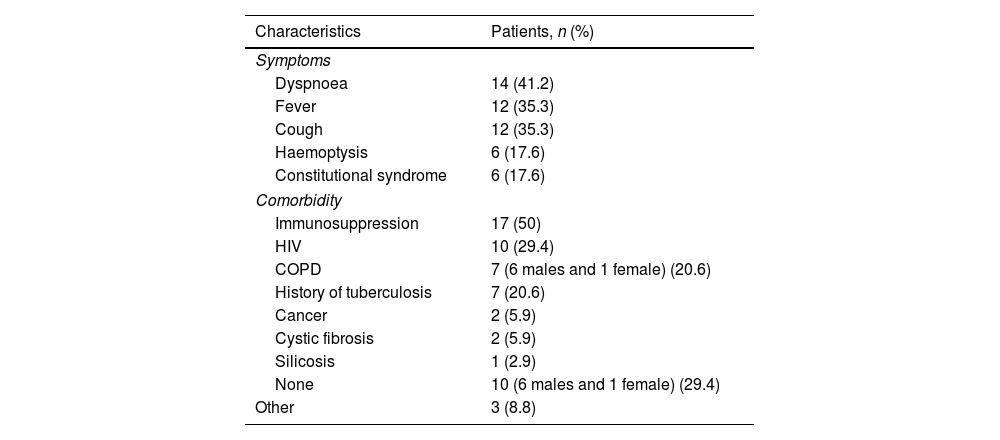
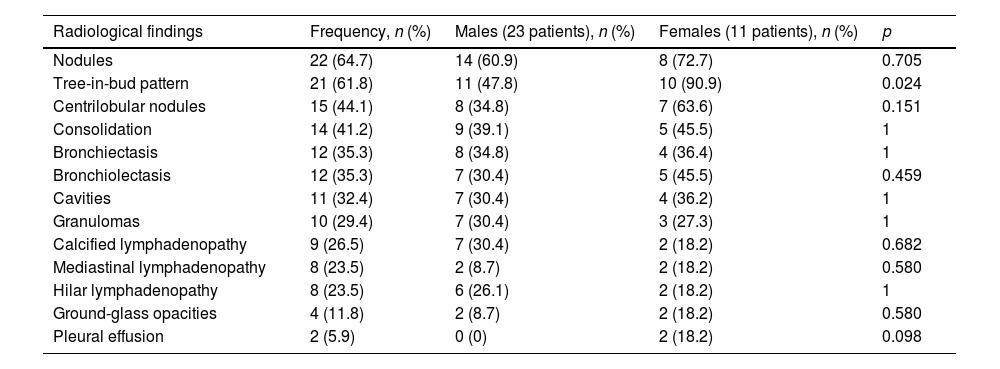
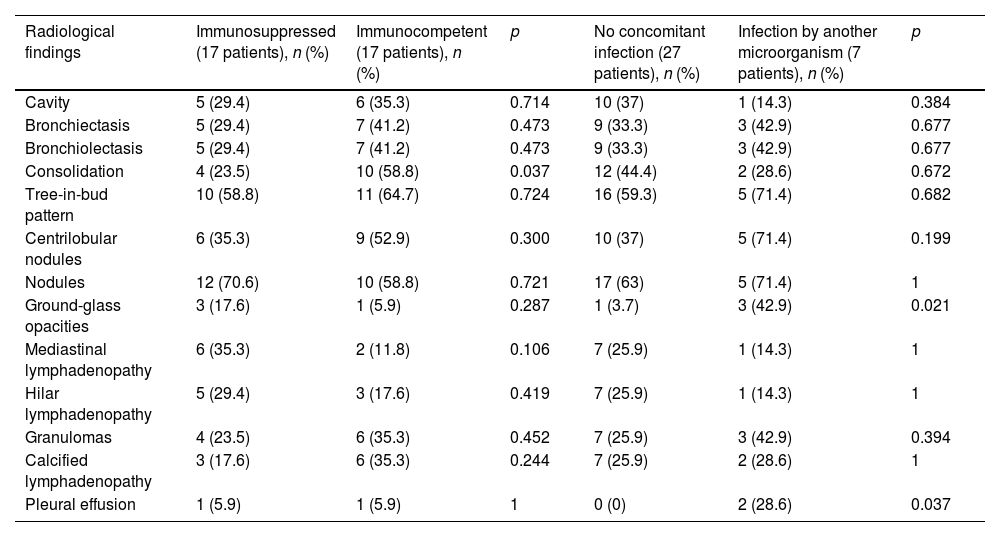
ResultsWe included 34 patients (mean age, 55 y; 67.6% men); 50% were immunodepressed (58.8% of these were HIV+), 20.6% had COPD, 5.9% had known tumors, 5.9% had cystic fibrosis, and 29.4% had no comorbidities. We found that 20.6% had a history of tuberculosis and 20.6% were also infected with other microorganisms. Mycobacterium avium complex was the most frequently isolated germ (52.9%); 7 (20.6%) were also infected with other organisms. The most common CT findings were nodules (64.7%), tree-in-bud pattern (61.8%), centrilobular nodules (44.1 %), consolidations (41.2%), bronchiectasis (35.3%), and cavities (32.4%). We compared findings between men and women and between immunodepressed and immunocompetent patients. Treatment was antituberculosis drugs in 67.6% of patients (72% of whom showed improvement) and conventional antibiotics in 20.6% (all of whom showed radiologic improvement).
ConclusionThe diagnosis of nontuberculous mycobacterial lung infections is complex. The clinical and radiologic findings are nonspecific and a significant percentage of pateints can have other, concomitant infections.
Describir la epidemiología y hallazgos en tomografía computarizada (TC) de las infecciones pulmonares por micobacterias no tuberculosas (IPMNT) y su evolución según el tratamiento.
Material y métodosEstudio retrospectivo de 131 pacientes consecutivos con cultivos positivos para micobacterias no tuberculosas (MNT) entre 2005 y 2016. Se seleccionaron los que cumplían con los criterios diagnósticos de IPMNT. Se analizaron los datos epidemiológicos, clínicos, microbiológicos, radiológicos, el tratamiento recibido y la evolución en función de este.
ResultadosSe incluyeron 34 pacientes con una edad media de 55 años, el 67,6% hombres. El 50% estaba inmunodeprimido (VIH positivos, el 58,8%); el 20,6% tenía EPOC; el 5,9%, neoplasias conocidas; el 5,9%, fibrosis quística; y el 29,4% no presentaba comorbilidades. El 20,6% presentaba antecedentes de tuberculosis y el 20,6% estaba infectado por otros microorganismos. Mycobacterium avium complex fue el germen más frecuentemente aislado (52,9%). Siete pacientes (20,6%) presentaron además infecciones por otros microorganismos. En la TC, los hallazgos más frecuentes fueron: nódulos (64,7%), patrón en árbol en brote (61,8%), nódulos centrolobulillares (44,1%), consolidaciones (41,2%), bronquiectasias (35,3%) y cavidades (32,4%). Se realizó un estudio comparativo de los hallazgos entre hombres y mujeres y entre pacientes inmunodeprimidos e inmunocompetentes. El 67,6% recibió antituberculostáticos (el 72% mostró mejoría) y el 20,6%, antibióticos convencionales (todos con mejoría radiológica).
ConclusiónEl diagnóstico de la IPMNT es complejo. Los hallazgos clínicos y radiológicos son inespecíficos y un porcentaje importante de pacientes puede presentar otras infecciones concomitantes.