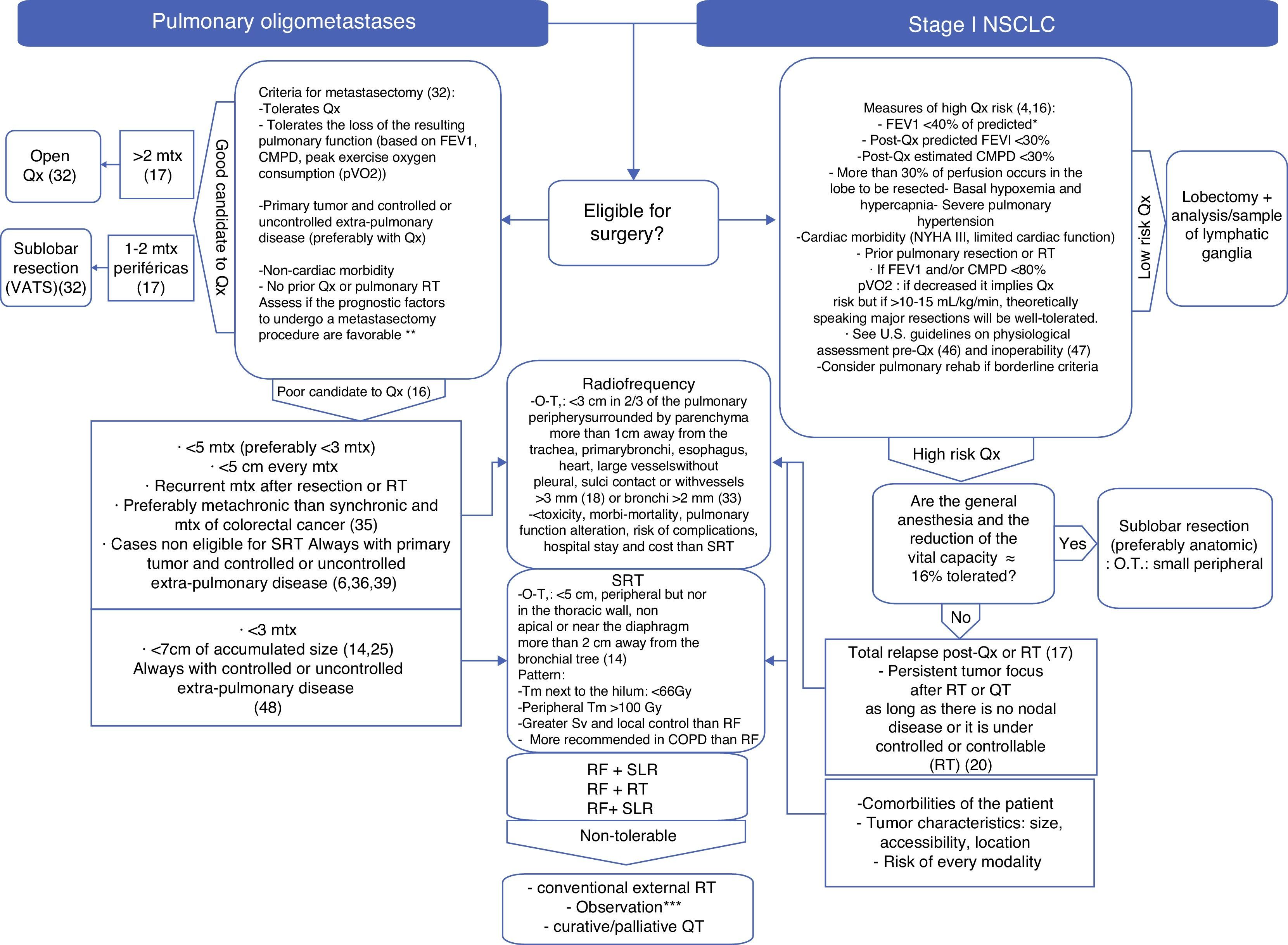
The risks involved in surgical treatment and conventional radiotherapy in patients with early lung cancer or lung metastases often make these treatments difficult to justify. However, on the other hand, it is also unacceptable to allow these lesions to evolve freely because, left untreated, these neoplasms will usually lead to the death of the patient. In recent years, alternative local therapies have been developed, such as pulmonary radiofrequency ablation, which has proven to increase survival with a minimal risk of complications. There are common recommendations for these treatments, and although the specific indications for using one technique or another have yet to be established, there are clearly defined situations that will determine the outcome of the treatment. It is important to know these situations, because appropriate patient selection is essential for therapeutic success. This article aims to describe the characteristics and constraints of pulmonary radiofrequency ablation and to outline its role in thoracic oncology in light of the current evidence.
Frecuentemente, los riesgos quirúrgicos y de la radioterapia convencional en los pacientes con cáncer de pulmón precoz o con metástasis pulmonares son inasumibles, pero dejarlos que evolucionen libremente es inaceptable porque la enfermedad neoplásica será la causa más frecuente de muerte del paciente. En los últimos años se han desarrollado terapias locales alternativas, como la radiofrecuencia pulmonar, que ha demostrado mejorar la supervivencia con un riesgo mínimo de complicaciones graves. Existen recomendaciones comunes para aplicar estas terapias y, aunque el papel concreto diferenciador de cada una está aún por establecer, hay situaciones claramente definidas que condicionarán el resultado del tratamiento. Conocerlas es importante, pues seleccionar adecuadamente al paciente será clave para el éxito terapéutico. El objetivo de este artículo es describir las características y condicionantes de la ablación pulmonar con radiofrecuencia y esbozar su papel en el ámbito de la oncología torácica de acuerdo a la evidencia actual.