Perinatal stress and the impact generated by adverse conditions could affect fetal development negatively with long term and short term manifestations and could increase the risk of maternal depression.
ObjectiveTo determine the psychosocial risk factors present in women with high-obstetric risk and hospitalized in a high complexity institution.
MethodsA cross-sectional study that included 112 pregnant or immediate postpartum women, who were evaluated using a scale designed by the researchers and the Edinburgh Postnatal Depression Scale.
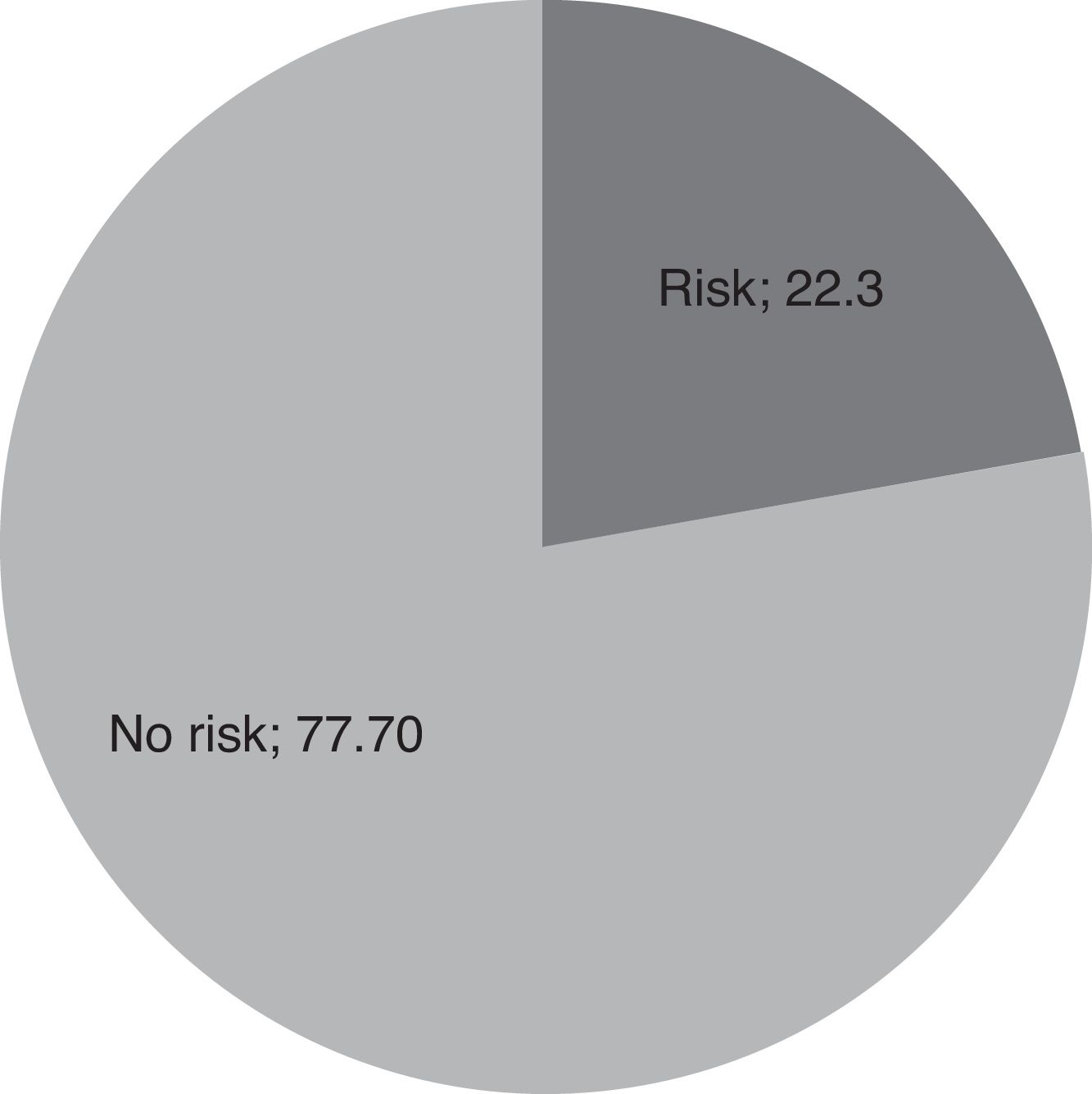
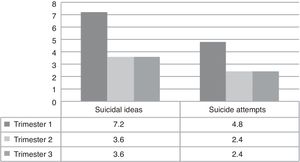
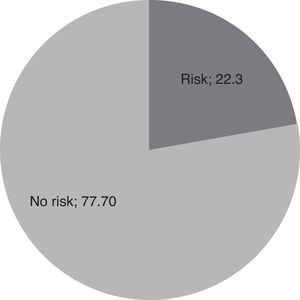
ResultsMedian age was 24 (RIC 9) years; 39.3% of the women were pregnant, and 65.9% had a gestational age of more than 28 weeks. The main reason for hospitalization was threat of preterm delivery in 39.2%. 52.4% planned the pregnancy and 22.3% had depressive symptoms compatible with depression. Suicidal ideas and suicide attempts were more prevalent in the first trimester (7.2% and 3.6%).
DiscussionThe high prevalence of depressive symptoms in the population studied coincides with what was reported in similar studies in Latin America. The fact that pregnancy does not protect against suicide was confirmed.
ConclusionsPsychosocial screening is recommended in every pregnant woman and women in immediate postpartum to detect symptoms and risk factors for depression.
El estrés perinatal y el impacto generado por condiciones adversas, podrían afectar negativamente el desarrollo fetal con manifestaciones a corto y largo plazo, y aumentaría el riesgo de desarrollar depresión materna.
ObjetivoDeterminar los factores de riesgo psicosocial presentes en mujeres con alto riesgo obstétrico, hospitalizadas en una institución de alta complejidad.
MetodologíaEstudio transversal que incluyó 112 mujeres embarazadas o en posparto inmediato, evaluadas a través de una escala diseñada por las investigadoras y la Escala de Depresión Posparto de Edimburgo.
ResultadosLa mediana para la edad fue 24 años (RIC 9). El 39,3% de las mujeres estaban embarazadas. El 65,9% tenía una edad gestacional mayor de 28 semanas. El principal motivo de hospitalización fue la amenaza de aborto en el 39,2%. El 52,4% planeó el embarazo y 22,3% tenía síntomas depresivos compatibles con depresión. Las ideas e intentos suicidas, fueron más prevalentes en el primer trimestre (7,2% y 3,6%).
DiscusiónLas características sociodemográficas y clínicas de la población estudiada coinciden con lo reportado previamente. La alta prevalencia de síntomas depresivos en la población estudiada coincide con lo reportado en estudios similares en Latinoamérica. Se confirma que el embarazo no protege contra el suicidio.
ConclusionesSe recomienda incluir tamización psicosocial a toda mujer en embarazo y post parto inmediato para detectar síntomas y factores de riesgo susceptibles de ser intervenidos precozmente y evitar desenlaces negativos tanto para la madre como para el neonato.
The need to make an approach taking gender into account in the health care field has become extremely important because women and men exhibit differences in the presentation of mental health disorders. Gender may affect every aspect of psychopathology including prevalence, symptom's expression, course of the disease, help seeking and response to treatment.1
Perinatal mental health study (a term that covers pregnancy and postpartum) has reached great relevance in the last few decades.2 According to the American College of Obstetrics and Gynecology (ACOG), psychosocial factors must be evaluated in the prenatal period, during pregnancy and postpartum to identify psychosocial problems that would increase the risk of a negative outcome.3
Stress is a multidimensional concept, which results from an unbalanced perception between environmental challenges (acute and chronic stressors) and individual resources (socio-economic conditions, life style, personality and social support) and it leads to a greater risk of maladaptive behavioral and emotional responses. One can speak of perinatal stress when it occurs during this period.4
There are studies that show how maternal stress has a direct effect on fetal wellbeing. This contradicts old ideas that considered pregnancy as a period which protects both the woman and the fetus from any noxa5
The World Health Organization (WHO) defines risk factor as any trait, characteristic or exposure an individual undergoes, which increases the individual's probability of suffering a disease or a lesion.6 Psychosocial risk factors are stressing events such as: the death of a family member, a marital breakup, unemployment, little support coming from the partner, scarce social support, low family income, an undesired pregnancy, physical and emotional violence, tobacco use, drug or alcohol abuse, poor schooling, and a personal history of psychiatric disorders. They are associated with the development of anxiety and depression during pregnancy and postpartum.2,7–11
Different studies have found that prenatal stress and depression are associated to placental abnormalities, villous and decidual necrosis, sharp inflammation and hemorrhage which correlates with an increase in pro-inflammatory factors, immune deficit and infections.12,13 Furthermore, there is a generation of neuroendocrine responses to stress that may contribute to negative perinatal results by different mechanisms. These include hypothalamic-pituitary-adrenal axis alterations, i.e. high levels of corticotropin-releasing hormone (CRH) which leads to a greater risk of premature birth. Likewise, catecholamine release affects the tone of peripheral blood vessels and contributes to developing preeclampsia, delay in intrauterine growth and preterm delivery.4,5,13–16
The impact generated by adverse conditions in the prenatal and postnatal periods could affect negatively a child's short and long-term neurological development.13,17,18 The above could increase vulnerability to developing future mental disorders.19–21 Likewise, it has been established that adults that suffered intrauterine growth restriction or who were born preterm have a greater risk of morbidity and premature mortality resulting from cardiovascular and metabolic diseases.22,23
Several studies show the existing relation between depression during pregnancy and postpartum and psychosocial risk factors.24 A recent study conducted with a sample of 2411 pregnant women, to whom the Edinburgh Postnatal Depression Scale was applied on the 16th week of pregnancy, showed that 233 (9.7%) of the patients had a positive screening for depression, and 153 of them met the criteria for another psychiatric disorder. Women with positive screening had greater probability of presenting psychosocial risk factors, including being unemployed (P≤.001), poor schooling level (P≤.001), and a history of partner violence (P≤.001) in comparison with the patients with negative screening.17
A lack of consensus regarding methodology and the populations analyzed in various studies hinder the determination of the real prevalence of depression during pregnancy and postpartum. More than 70% of pregnant women reported depressive symptoms, 10 to 16% of them met the criteria for major depressive disorder. In fact, more than 10% of the women evaluated for postpartum depression consulted for symptoms that had been presenting since pregnancy.25
Nonetheless, one can accept that global prevalence of this disorder in the prenatal stage fluctuates between 7.4% in the first trimester of pregnancy and 12% in the third trimester.5 Approximately, between 10 and 15% of new mothers presented postpartum depression according to recent literature,12,26–28 and up to 80% experimented some sort of ‘baby blues’.20 Studies conducted in some developing countries showed a prevalence of postpartum depression that fluctuated from 8% to 50%, and it was three times higher than in developed nations.26,29
In Chile, Alvarado et al. demonstrated that having vital events during pregnancy, low socio-economic level and maternal malnutrition were risk factors for developing depression (P<.05) while having adequate social support was deemed as a protective factor (P=.221).30
In Colombia, a study conducted in the year 2000 found that the prevalence of depression in the perinatal period was 66%, with 57% in the postpartum. They determined the prevalence with the Center for Epidemiologic Studies Depression (CES-D). In addition, they found that the unmet needs for support and satisfaction along with social support and level of conflict could be predictors of depressive symptomatology.31 Another study carried out by Ortiz Martinez et al. in 2016 showed a prevalence of 40.20% (95%CI, 33%-47%) of positive screening for postpartum depression using the Edinburgh Depression Scale. The possible factors associated with this were: high risk of obstetric pathology, hospitalized newborn, poor social support, inability to breastfeed, African/Indian race, schooling less than five years, and a subsidized healthcare scheme.32
The objective of the present study was to determine the psychosocial risk factors of high-obstetric risk women hospitalized in a third level institution.
MethodsDesign of the Study and Population IncludedThis was an observational descriptive cross-sectional study. All the women admitted to the hospitalization service at Medellin General Hospital and who met the inclusion criteria were included in the study from November 1st to December 19th, 2014. The inclusion criteria included: a) being literate; b) being pregnant or in the immediate postpartum, and c) having signed the informed consent, which was given to all women older than 14 years of age, while those under that age had the consent form signed by the parent or guardian.
Variables AnalyzedThe variables included were sociodemographic (age, sex, schooling, marital status, place of birth and place of residence), obstetrical (gestational age, reason for hospitalization, abortions, prior deliveries and cesareans, prenatal control); psychiatric (Edinburgh scale), psychosocial (negative vital events in the last 12 months, perception of family life, social and economic status and relationship with the partner).
Collection of InformationThe information required for all the variables of the study was obtained. The unit of analysis was pregnant women admitted at HGM either for obstetrical complications or labor. The language of the questions was simple, and participating women took approximately 30 minutes to fill it out. One of the researchers (JV) was in charge of motivating patients to participate in the research, and she was present to clarify any doubts and guarantee that the survey was filled out correctly.
The Edinburgh Scale33 was used for depression screening. At first, it was proposed as a screening tool for postpartum depressive diagnoses, yet it has been widely tested, translated and used in more than 23 countries to identify women who could be undergoing postpartum depression. This scale has also been used as a tool to detect depression in the 3 trimesters of pregnancy.34,35
The researchers obtained permission to use the scale validated in Spanish by Jadresic et al. In 2007, Campo-Arias et al. conducted a study and showed that the Edinburgh Postnatal Depression Scale had high internal consistency and was composed of a three-dimensional structure exploring the concept of depression in low-income pregnant women in Cartagena, Colombia.36 The 10-item scale was self-administered and took 5 minutes approximately to fill it out completely. The questions are Likert-type with a 0 to 3 score, where 0 corresponds to “No, never” and 3 corresponds to “Yes, most of the time”. The maximum score was 30. When the cutoff point is taken between 12 and 13, greater global efficiency is obtained (correct case classification and no cases in 87.4%), with a good combination of positive predictive values (PPV) (85.3%) and negative predictive values (NPV) (88.3%) in addition to 76.3% sensitivity and 93.2% specificity.
Statistical AnalysisThe description of qualitative variables was conducted using absolute and relative frequencies, the median [interquartile range] were used for age because the variable did not have a normal distribution. To analyze information, the SPSS® 2012 version 21.0 (SPSS Inc.; Chicago, Illinois, USA) software was used under a license from Universidad CES.
Ethical AspectsThis research was approved by the Ethics Committee at Universidad CES and the Research Committee at Hospital General de Medellin. Women participants over 14 were asked to sign an informed consent and women under 14 were asked to have their family or legal guardian signed it. Confidentiality of the information analyzed was guaranteed at all times.
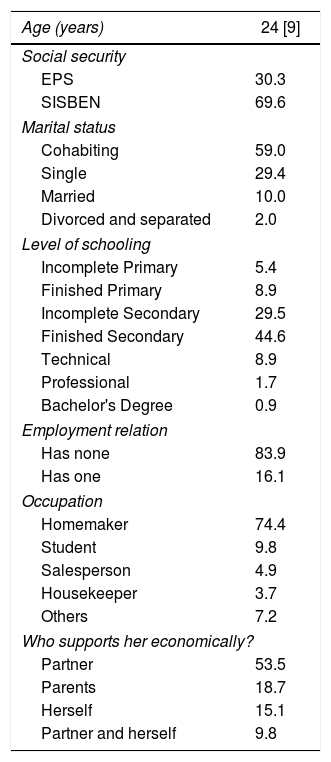
ResultsDescriptive AnalysisThe final analysis included 112 women. The median age was 24 [9] years (range, 13-45). 30.3% of the patients had health insurance using an HMO (in Spanish, Entidad Prestadora de Salud [EPS]) and 69.6%, Potential Social Program Beneficiary Identification System (In Spanish, Sistema de Identificación de Potenciales Beneficiarios de Programas Sociales [SISBEN]). 58.9% of the women lived with their partners and 29.4% were single. Regarding their level of schooling, 44.6% finished basic secondary school. Regarding religion, 92% reported belonging to a religion, and 73.3% were catholic. 83.9% of the patients had no job and 53.3% depended economically on their partners (Table 1).
Socio-demographic characteristics of the population in the study.
| Age (years) | 24 [9] |
|---|---|
| Social security | |
| EPS | 30.3 |
| SISBEN | 69.6 |
| Marital status | |
| Cohabiting | 59.0 |
| Single | 29.4 |
| Married | 10.0 |
| Divorced and separated | 2.0 |
| Level of schooling | |
| Incomplete Primary | 5.4 |
| Finished Primary | 8.9 |
| Incomplete Secondary | 29.5 |
| Finished Secondary | 44.6 |
| Technical | 8.9 |
| Professional | 1.7 |
| Bachelor's Degree | 0.9 |
| Employment relation | |
| Has none | 83.9 |
| Has one | 16.1 |
| Occupation | |
| Homemaker | 74.4 |
| Student | 9.8 |
| Salesperson | 4.9 |
| Housekeeper | 3.7 |
| Others | 7.2 |
| Who supports her economically? | |
| Partner | 53.5 |
| Parents | 18.7 |
| Herself | 15.1 |
| Partner and herself | 9.8 |
Data are presented as median [interquartile range] or percentage.
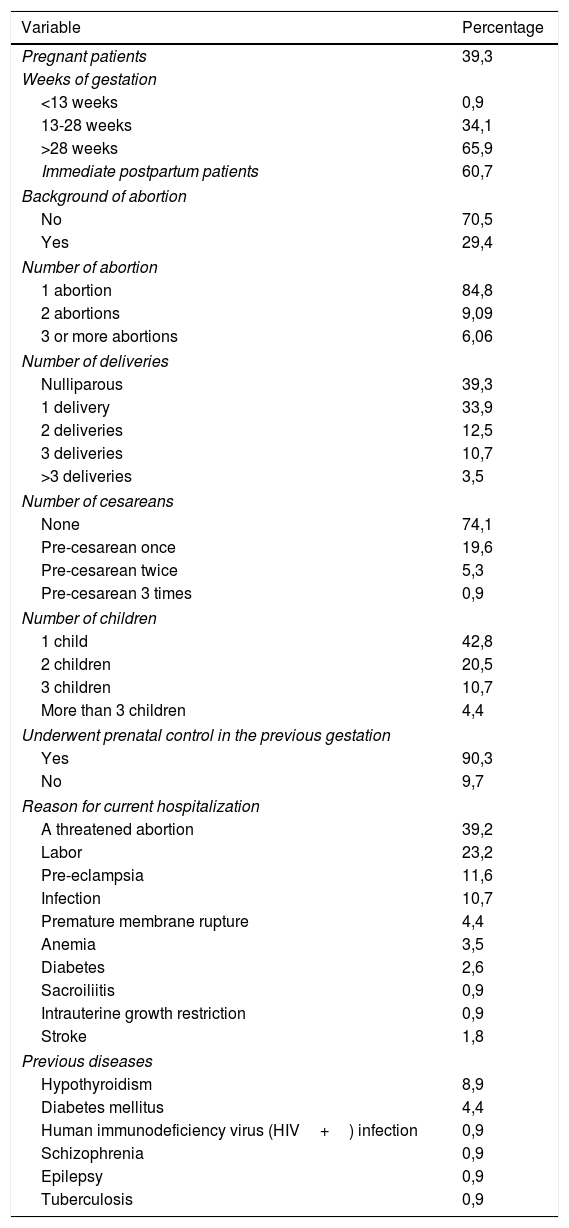
39.3% of the women studied were pregnant and 60.7% were in immediate postpartum (up to 3 days postpartum). 65.9% of the pregnant women had a gestational age of more than 28 weeks. 34.1% had 13 to 28 weeks of gestation and just 1 woman had a gestational age less than 13 weeks. The main reasons for hospitalization for these women were: threat of preterm delivery (39.28%), labor (23.2%), and pre-eclampsia (11.6%). Regarding OB/GYN history, 29.4% had a history of abortion and 84.8% of them had had 1 abortion. 39.3% of the women were nulliparous; 42.8% had 1 child and 20.5% had 2.
On the other hand, 90.3% of the women with prior gestations had undergone prenatal control, and 25.9% were pre-cesarean. 8.9% of the women had a history of hypothyroidism and 4,4% had a history of diabetes (Table 2).
OB/GYN characteristics of the population in the study.
| Variable | Percentage |
|---|---|
| Pregnant patients | 39,3 |
| Weeks of gestation | |
| <13 weeks | 0,9 |
| 13-28 weeks | 34,1 |
| >28 weeks | 65,9 |
| Immediate postpartum patients | 60,7 |
| Background of abortion | |
| No | 70,5 |
| Yes | 29,4 |
| Number of abortion | |
| 1 abortion | 84,8 |
| 2 abortions | 9,09 |
| 3 or more abortions | 6,06 |
| Number of deliveries | |
| Nulliparous | 39,3 |
| 1 delivery | 33,9 |
| 2 deliveries | 12,5 |
| 3 deliveries | 10,7 |
| >3 deliveries | 3,5 |
| Number of cesareans | |
| None | 74,1 |
| Pre-cesarean once | 19,6 |
| Pre-cesarean twice | 5,3 |
| Pre-cesarean 3 times | 0,9 |
| Number of children | |
| 1 child | 42,8 |
| 2 children | 20,5 |
| 3 children | 10,7 |
| More than 3 children | 4,4 |
| Underwent prenatal control in the previous gestation | |
| Yes | 90,3 |
| No | 9,7 |
| Reason for current hospitalization | |
| A threatened abortion | 39,2 |
| Labor | 23,2 |
| Pre-eclampsia | 11,6 |
| Infection | 10,7 |
| Premature membrane rupture | 4,4 |
| Anemia | 3,5 |
| Diabetes | 2,6 |
| Sacroiliitis | 0,9 |
| Intrauterine growth restriction | 0,9 |
| Stroke | 1,8 |
| Previous diseases | |
| Hypothyroidism | 8,9 |
| Diabetes mellitus | 4,4 |
| Human immunodeficiency virus (HIV+) infection | 0,9 |
| Schizophrenia | 0,9 |
| Epilepsy | 0,9 |
| Tuberculosis | 0,9 |
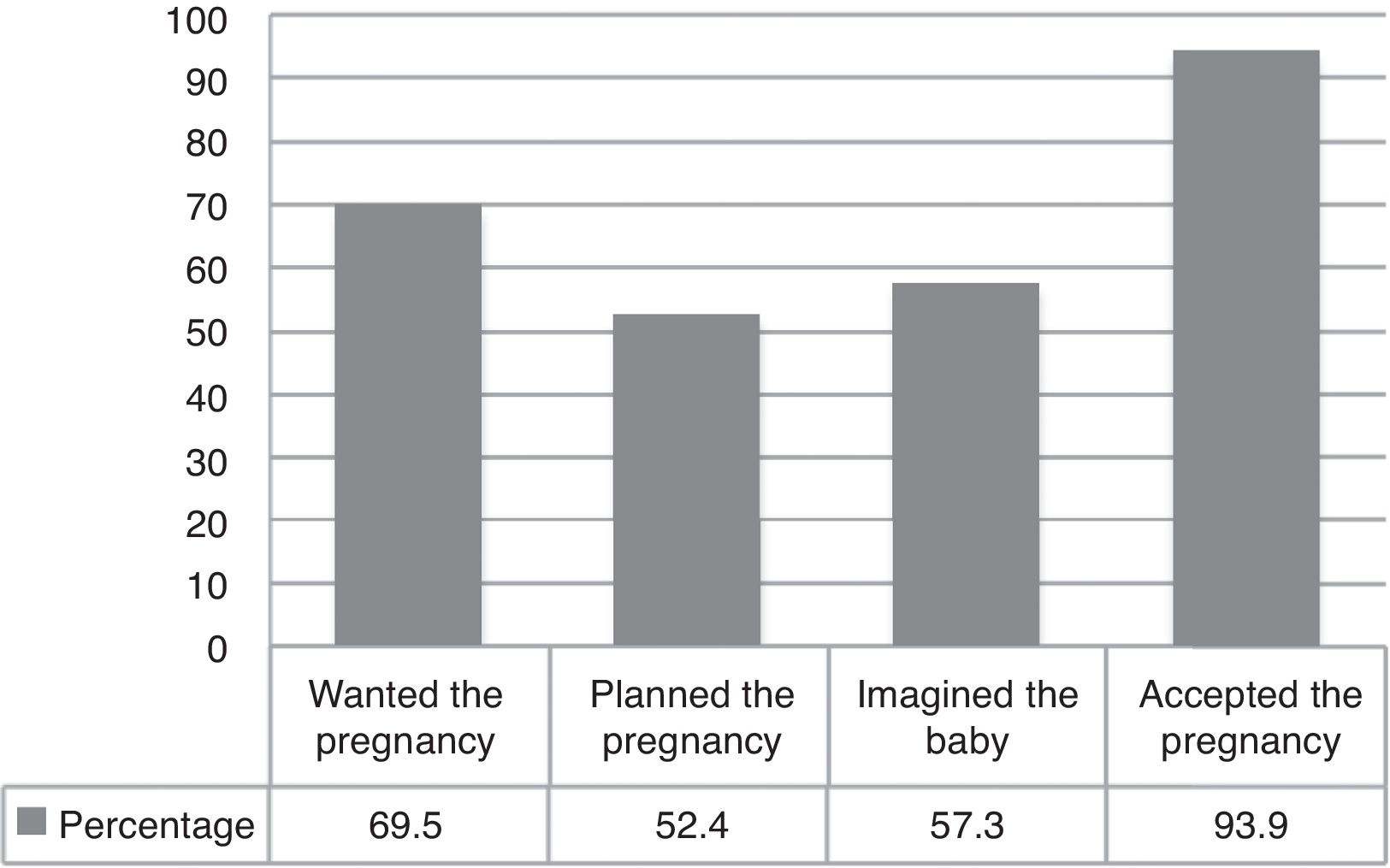
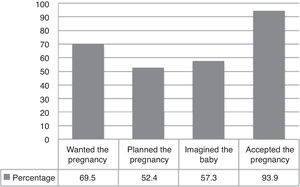
The possibility that each pregnant woman had to imagine, plan, accept and want gestation was explored, and it was found that 57.3% of the pregnant women imagined their baby, only 52.4% had planned their pregnancy, 69.5% had desired a pregnancy and 93.9% eventually accepted it (fig. 1).
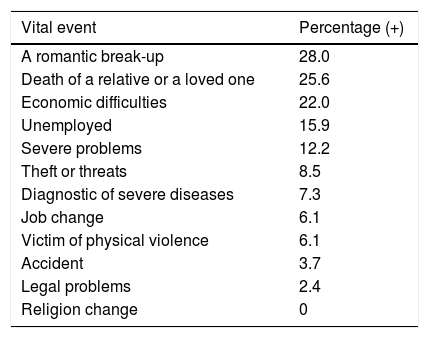
Negative Vital Events Which Occurred in the Last 12 MonthsThe following 12 vital events, occurring in the past 12 months of life, were explored: death of a relative or a loved one; a significant break-up; severe problems; economic difficulties; theft or loss of valuable objects; the diagnosis of a severe disease; unemployment; job change; legal problems; an accident; victim of physical violence, and change in religion. The most prevalent vital event was a break-up (28.0%), followed by the death of a relative or a loved one (25.6%), and economic difficulties (22.0%). It is worth noting that 6.1% of the women stated that in the last year they had been victims of some sort of physical violence (Table 3).
Distribution of negative vital effects on the population in study in the last 12 months.
| Vital event | Percentage (+) |
|---|---|
| A romantic break-up | 28.0 |
| Death of a relative or a loved one | 25.6 |
| Economic difficulties | 22.0 |
| Unemployed | 15.9 |
| Severe problems | 12.2 |
| Theft or threats | 8.5 |
| Diagnostic of severe diseases | 7.3 |
| Job change | 6.1 |
| Victim of physical violence | 6.1 |
| Accident | 3.7 |
| Legal problems | 2.4 |
| Religion change | 0 |
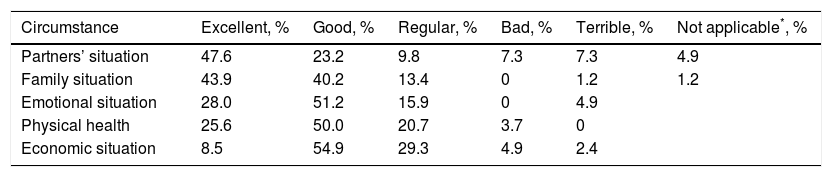
Women were asked about their perception of the circumstances surrounding the start of the gestation from the point of view of partner's relationship, family relations, economic situation, physical health and emotional status. The questions which evaluated these aspects were Likert-type and had 5 possible answers: excellent, good, regular, bad and terrible. The partners’ situation at the time of the pregnancy was excellent or good for 70.8% and regular, bad or terrible for 24.4%. 84.1% of the women surveyed ranked their family situation between excellent and good, and 15.8% between regular and terrible. Regarding the economic situation, 54.9% ranked it as good and it was regular, bad or terrible for 36.6%. 75.6% ranked physical health as excellent or good at the time of the pregnancy, while their emotional situation was excellent or good for 79.2% and regular, or terrible for 19.6% (Table 4).
Personal family and social circumstances that framed the start of the gestation of the population in the study.
| Circumstance | Excellent, % | Good, % | Regular, % | Bad, % | Terrible, % | Not applicable*, % |
|---|---|---|---|---|---|---|
| Partners’ situation | 47.6 | 23.2 | 9.8 | 7.3 | 7.3 | 4.9 |
| Family situation | 43.9 | 40.2 | 13.4 | 0 | 1.2 | 1.2 |
| Emotional situation | 28.0 | 51.2 | 15.9 | 0 | 4.9 | |
| Physical health | 25.6 | 50.0 | 20.7 | 3.7 | 0 | |
| Economic situation | 8.5 | 54.9 | 29.3 | 4.9 | 2.4 |
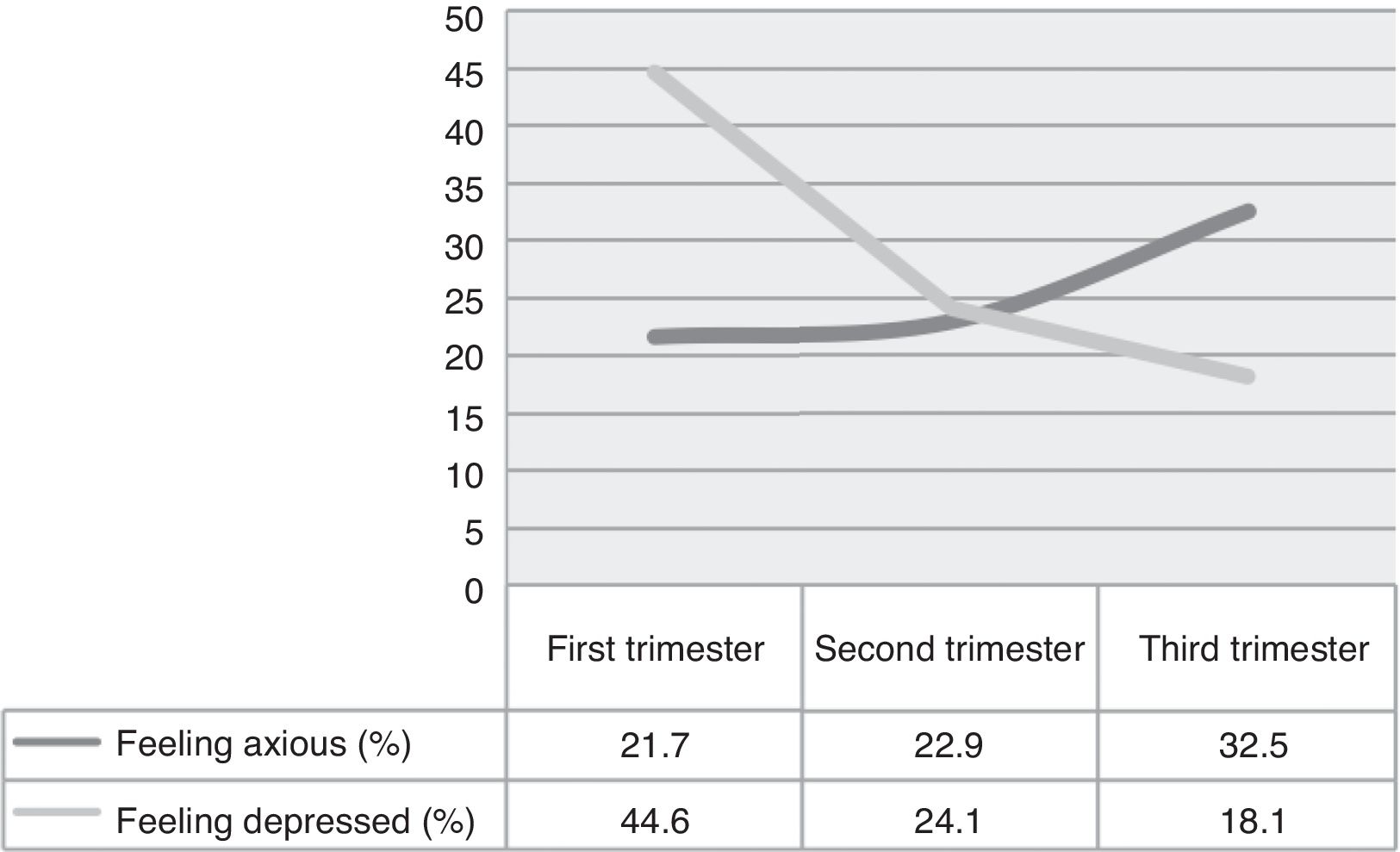
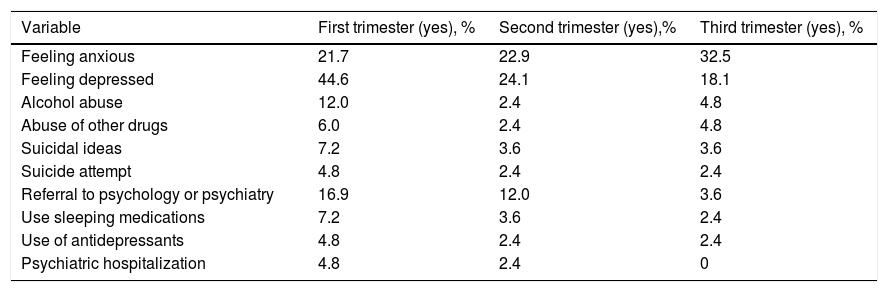
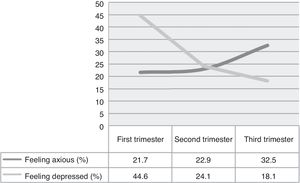
The women surveyed were asked to answer some questions and discriminate responses depending on the trimester of gestation. The ratio of women who said they felt increased anxiety during their pregnancy reached 32.5% in the third trimester. On the other hand, feeling depressed showed the largest ratio in the first trimester with 44.6% and just 18.1% in the third trimester (fig. 2).
The use of hypnotics and antidepressants showed the same pattern with a larger ratio in the first trimester (7.2% and 4.8%) and a gradual decrease until the third trimester (2.4% and 2.4%). Regarding psychiatric hospitalization in the first trimester, 4.8% of the women required it, 2.4% in the second trimester and none in the third trimester. Referral of patients to psychology or psychiatry was 16.9% in the first trimester, 12.0% in the second trimester, and 3.6% in the third trimester. The use of liquor was greater than any other drug in the first trimester (12.0% vs. 6.0%), while in the second and third trimester, the ratio of women that used alcohol and other drugs was the same (Table 5).
Mental health and substance abuse depending on the trimester of gestation.
| Variable | First trimester (yes), % | Second trimester (yes),% | Third trimester (yes), % |
|---|---|---|---|
| Feeling anxious | 21.7 | 22.9 | 32.5 |
| Feeling depressed | 44.6 | 24.1 | 18.1 |
| Alcohol abuse | 12.0 | 2.4 | 4.8 |
| Abuse of other drugs | 6.0 | 2.4 | 4.8 |
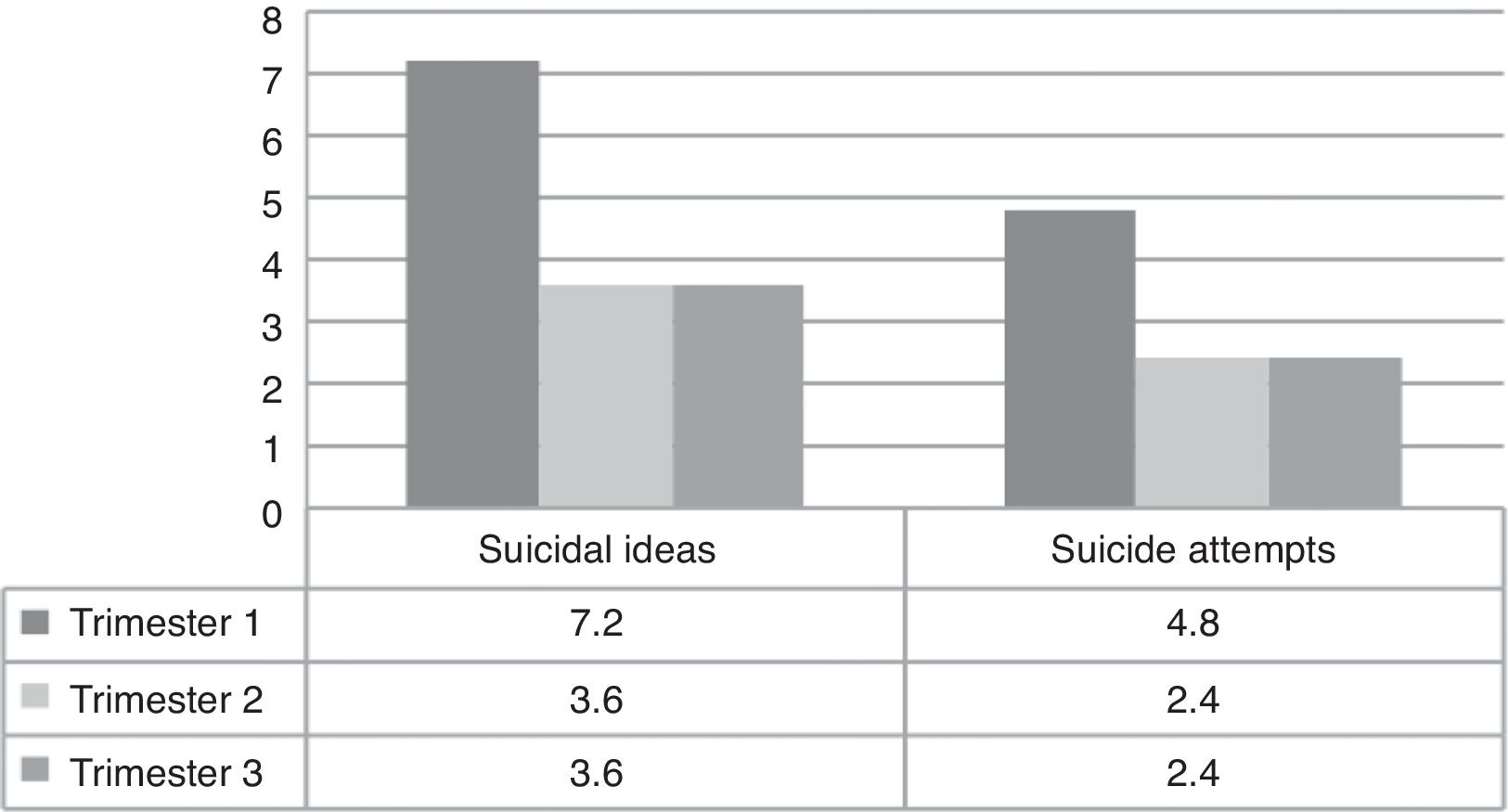
| Suicidal ideas | 7.2 | 3.6 | 3.6 |
| Suicide attempt | 4.8 | 2.4 | 2.4 |
| Referral to psychology or psychiatry | 16.9 | 12.0 | 3.6 |
| Use sleeping medications | 7.2 | 3.6 | 2.4 |
| Use of antidepressants | 4.8 | 2.4 | 2.4 |
| Psychiatric hospitalization | 4.8 | 2.4 | 0 |
Suicidal behavior (ideas or attempts) showed a similar trend to the one for depression with a larger ratio in the first trimester (7.2% and 4.8%) than the third one (3.6% and 2.4%) (fig. 3).
Edinburgh Scale22.36% of the women evaluated had a >12 score on the Edinburgh scale, which represents a risk of presenting perinatal depression (fig. 4).
Discussion112 women were characterized socio-demographically, clinically and psychosocially during their perinatal period in a high-obstetric-risk institution. Despite the importance of this topic, there are few Colombian studies that address this issue. In a meta-analysis conducted by Littleton et al., in which they included 35 studies published between 1991 and 2009 including a total of 31.323 women, they found an association between psychosocial stress and negative perinatal outcomes.7
In the world, of 210 million pregnancies a year, 80 million are not planned; that is to say 2 of each 5 pregnancies (OMS, 2010). In Colombia, there is an estimate of 89 unplanned pregnancies for each 1000 women in reproductive age every year. Rates vary widely in the five main regions of the country, from 67 per 1000 in the Central and Eastern regions and up to 113 per 1000 in Bogota.7 The ratio of unplanned births has increased from 36% in 1990 to 51% in 2010. Currently, in Colombia, 2 of every 3 pregnancies are not planned. This coincides with the report in this study where 1 of every 2 pregnancies was not planned.37,38
While it is striking that 1 in 4 women in our study have had both induced and spontaneous abortions, it is not possible to compare this finding with other studies, since proper measurement of abortion levels is difficult in many areas of the world. It has been found that the proportion of abortions (abortions per 100 pregnancies) ending in a birth or abortion is higher in the developed than in the underdeveloped regions (42% vs. 23%). Even in Eastern Europe, the highest percentage of pregnancies ending in abortions is 65%.39
A recent study,40 conducted in a public hospital in México City, found that the average age was 25±6.4 years, and 91.7% had schooling higher than primary. This is similar to what was found in this study. Regarding marital status, a Colombian study on pregnant women reported that 54% of the patients cohabited, and this coincides with was reported here.31
The relation between social support and obstetric outcomes has been studied previously.41 Nuckolls et al.’s pioneer study in the sixties demonstrated the protective effect of social support in the presence of high stress levels.42 We found that 80% of women depended financially on their families and/or partners. Only 1/5 was financially independent. Furthermore, 1 out every 3 women reported unfavorable (very bad, bad, fair) economic circumstances during pregnancy.
In a Mexican study, the prevalence of domestic violence towards women varies widely from 5.2%41 up to 19.8%.40 In this study, 6.1% reported violence in the past year.
The proportion of women that felt increased anxiety during their pregnancy coincides with Rubertsson et al.,43 who found a 15.6% prevalence for anxious symptoms during the beginning of gestation, and Lee et al.44 found a prevalence of 54% of anxious symptoms before delivery.
We considered that the depressive symptoms detected in the evaluation of women in the inmediate postpartum (first 72 h) had been present during gestation. In other words, the depressive symptoms found in our patients do not correspond to “baby blues” since we consider that the symptoms of this entity appear after the third day postpartum.45
A Colombian study found that 66% had depressive symptomatology in the prenatal stage and 57% had it in the postpartum.31 In our study, the Edinburgh scale found that 22.3% of the women evaluated had a risk of perinatal depression with a score of 12 or more; this widely surpasses that 13% reported in world literature.
These differences are noteworthy; we consider that this could be explained by the numerous unfavorable psychosocial factors of the women included in our sample. Nevertheless, more research is required regarding this matter to determine possible associations.
Beyond the biological risks generated by maternal depression, suicide must be considered as a possible outcome in the pregnancies of high-psychosocial-risk women.46 This challenges the previously held idea that pregnancy is protective against mental disorders. Our finding regarding suicidal behavior deserves special attention. In a large cohort study, 22 118 women were evaluated in the first trimester of gestation and 6 weeks postpartum, they found that suicidal ideas were present in 3.8% (95%IC, 3.5-4.1%) of the women evaluated, and 1.1% (95%CI, 0.2-1.9%) had high suicide risk. This study found that suicidal ideas and plans behaved similar to depressive symptoms with a higher ratio in the first trimester. Nevertheless, it is worth noting that the prevalence of suicidal ideas we reported is almost twice than Kim et al.47 reported. In a recent British study in women in contact with psychiatric services, suicides in the perinatal period were more likely to occur in those with a diagnosis of depression and no active treatment.48
Regarding the limitations of this study, one must bear in mind that the women were surveyed in a public hospital in the city of Medellin. Hence, results cannot be generalized for all the population of Colombia. Participation was voluntary, so the women who participated could be different from women who did not participate. Nonetheless, just few women refused to participate. Since the information obtained was self-report, memory bias is possible. In addition, women may have been afraid or embarrassed when they answered certain questions, so this could have reduced information validity. Nevertheless, accompaniment was given to women who decided to participate, and one of the researchers cleared up doubts. Finally, the survey used to gather this information was designed by the researchers, and it has not been validated.
ConclusionsThe high prevalence of adverse psychosocial factors and mental symptoms of anxiety and depression reported support the need to include psychosocial screening for all pregnant and immediate postpartum women, in order to detect symptoms and risk factors susceptible of being intervened to prevent negative outcomes for the mother and the newborn.
The importance of evaluating psychosocial risk factors is clearly associated with diseases as depression, which presents bidirectionally as a psychosocial risk factor and/or a consequence. In addition, it has been demonstrated that depression does not just affect the mother's emotional status, but also it generates diverse neuroendocrine and immunological alterations that affect fetal wellbeing, and these increase the risk of complications as preterm birth, restriction of intrauterine growth and preeclampsia.
Detection of psychosocial risk factors and screening for depression and anxiety would allow practitioners to tailor their interventions in order to reduce the impact of distress and unfavorable life circumstances on the outcomes for the mother and the newborn. Therefore, it is imperative that sexual and reproductive health providers acquire the competencies to comprehensively evaluate these aspects in pregnant women.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsNone.
We specially thank the women who helped us on this research.