Enhanced recovery after surgery (ERAS) programmes have been shown to reduce postoperative complications, use of critical care units, and length of hospital stay without increasing readmission rates, and are also cost-effective1. The number of declared ERAS centres in Spain has grown exponentially in recent years, but much work remains to be done. However, the spread of the Coronavirus disease (COVID-19) in the spring of 2020 created major challenges for healthcare systems. Non-urgent and non-cancer-related procedures, and even cancer-related procedures in some heavily affected hospitals, were cancelled worldwide to make way for COVID-19 patients, many of which were admitted to intensive care units, generating the so-called Post COVID-19 Surgical Backlog2. Some ERAS preoperative interventions, such as anaemia correction or prehabilitation, might also have been curtailed due to lockdown travel rules and the restrictions imposed on hospital admissions for therapy.
Hospitals where ERAS is routine practice have had difficulties maintaining these programmes due to the high number of COVID-19 patients, and those that did not routinely apply ERAS before the pandemic have found it difficult to start introducing the protocols.
The objective of this study was to evaluate current ERAS practice in major surgery by means of a questionnaire sent to anaesthesiologists and surgeons after the first wave of the COVID19 pandemic in Spain.
The Spanish Perioperative Audit and Research Network (REDGERM), the Spanish Society of Anaesthesiology and Critical Care (SEDAR) and the Spanish Association of Surgeons (AEC) endorsed the survey after it had been approved by their respective scientific and research committees.
The target population of this study were members of REDGERM. The estimated size of the target population for our survey was about 1000 researchers. Using a study sample size calculator (total population 1000, 95% confidence interval), we calculated that a total sample size of 278 participants would be needed to obtain useful information.
We contacted REDGERM researchers from more than 125 Spanish centres inviting them to voluntarily complete an open questionnaire on the Internet. The invitation included a link to the survey. The survey was not made public, so access to the questionnaire by uninvited people was unlikely. Participant responses were collected using Google forms. The survey was active for 1 month. Respondents implicitly gave their informed consent by opening, completing, and returning the online questionnaire. The questionnaire was a structured, web-based form with single and multiple response questions. All questions were mandatory. To prevent investigators completing multiple questionnaires, they were asked to provide their name and email, and duplicate entries in the database were eliminated before performing the analysis.
A 44-item questionnaire was developed to determine the changes in the perioperative management of patients caused by the COVID pandemic. Participants were asked to answer the questions based on their personal clinical practice at the time the survey was launched — 15 June 2020 — and not on the changes introduced mid-way during the first wave of the pandemic. The questions were structured in blocks: in the first, the respondent's demographic characteristics were obtained; in the second, the change in each of the perioperative items was characterized based on the recommendations of the ERAS Society; and in the third, participants were asked to rate their adherence (from 0 [minimum] to 10 [maximum]) to a series of ERAS items. The face validity and content of the questionnaire were established and tested during the development phase by a panel of experts from REDGERM (JVL, JRM, AAM), SEDAR (CA) and AEC. Data were expressed as frequency (proportion) and median (IQR) and analysed according to the number of responses obtained for each item. Median adherence to each perioperative item was compared using Friedman’s test. To avoid incongruent answers, we eliminated comparisons made by respondents who had previously stated that a particular ERAS item was not implemented. We also eliminated answers where respondents had already stated that the pandemic did not change a particular item, but in the next question (which assessed the extent of adherence to that item), the respondent answered that the change in adherence before and after the pandemic was greater than half.
The questionnaire was completed by 30.3% of physicians contacted. We received a total of 320 completed questionnaires. Two hundred and fifteen questionnaire were completed by anaesthesiologists (67.2%), 99 by surgeons (30.9%) and 6 by other specialists (1.87%); 212 physicians (66.3%) worked in hospitals with up to 600 beds. More than half of the participants (58.8%) had been routinely tested for Coronavirus. Almost all respondents reported that in their centres, patients were screened for SARS-CoV-2 infection preoperatively (98.4%), with RT-PCR of nasopharyngeal swabs being the most common test (94.4%).
Of the total number of respondents, 37% stated that surgery for non-malignant diseases had been postponed in their centres, 18% stated that only oncologic surgeries were performed, and 2.82% that only emergency surgeries were performed in their hospital. Multidisciplinary meetings to decide on the surgical oncology programme were held frequently (38.4%) or had been reduced (23.8%). Respondents believed that in many cases the decisions have been influenced by the pandemic, prioritising neoadjuvant therapy over surgery (36.9%). Our survey has shown that post-operative care has been adapted to the pandemic, with shorter than usual stays in the Critical Care Unit (44.8%). In many cases, critical care beds were not available in the post-operative period, and patients were transferred directly to the ward (7.19%).
Respondents also stated that standard clinical pathways have been altered, with some patients being discharged home earlier than usual due to the workload and to avoid Coronavirus infection (31.6%)
Nearly all (83.4%) respondents stated that ERAS pathways were implemented in their centres. Despite this, before the pandemic, only 60% of respondents stated that ERAS patients attended a specific pre-operative visit in their hospitals, and in 44.1% of cases no regular specific multidisciplinary meetings were held to audit improvements and monitoring. A large number of respondents indicated that prehabilitation programmes had never been implemented in their centres (35.9%). In centres where prehabilitation was implemented (64.1%), there was a statistically significant decrease in the subjective perception of patients who underwent prehabilitation before versus after COVID (Friedman X2 = 96.593, p < 0.05). Two-hundred and fifty-seven respondents (80.3%) performed preoperative nutritional assessment before the pandemic. There were significant differences among participants who believed that patient screening had changed before and after the COVID pandemic (Friedman X2 = 61.357, p < 0.05).
Treatment of anaemia had not changed in the hospitals of 65.3% of respondents, but respondents observed differences in the number of patients who underwent preoperative assessment and treatment of anaemia. The administration of carbohydrate drinks 2 h before surgery had been slightly reduced due to the pandemic. Adherence to this measure remains very low (55.6%). Most surgical approaches were laparoscopic (88.4%), and epidural analgesia was usually used in open surgery (88.1%). Respondents observed that the use of multimodal analgesia (95.6%), thromboprophylaxis according to guidelines (97.2%), management of postoperative fluids, early oral intake (92.2%), treatment of postoperative malnutrition (85.3%), and early mobilization (89.7%) have varied less than 5% following the outbreak of SARS CoV-2.
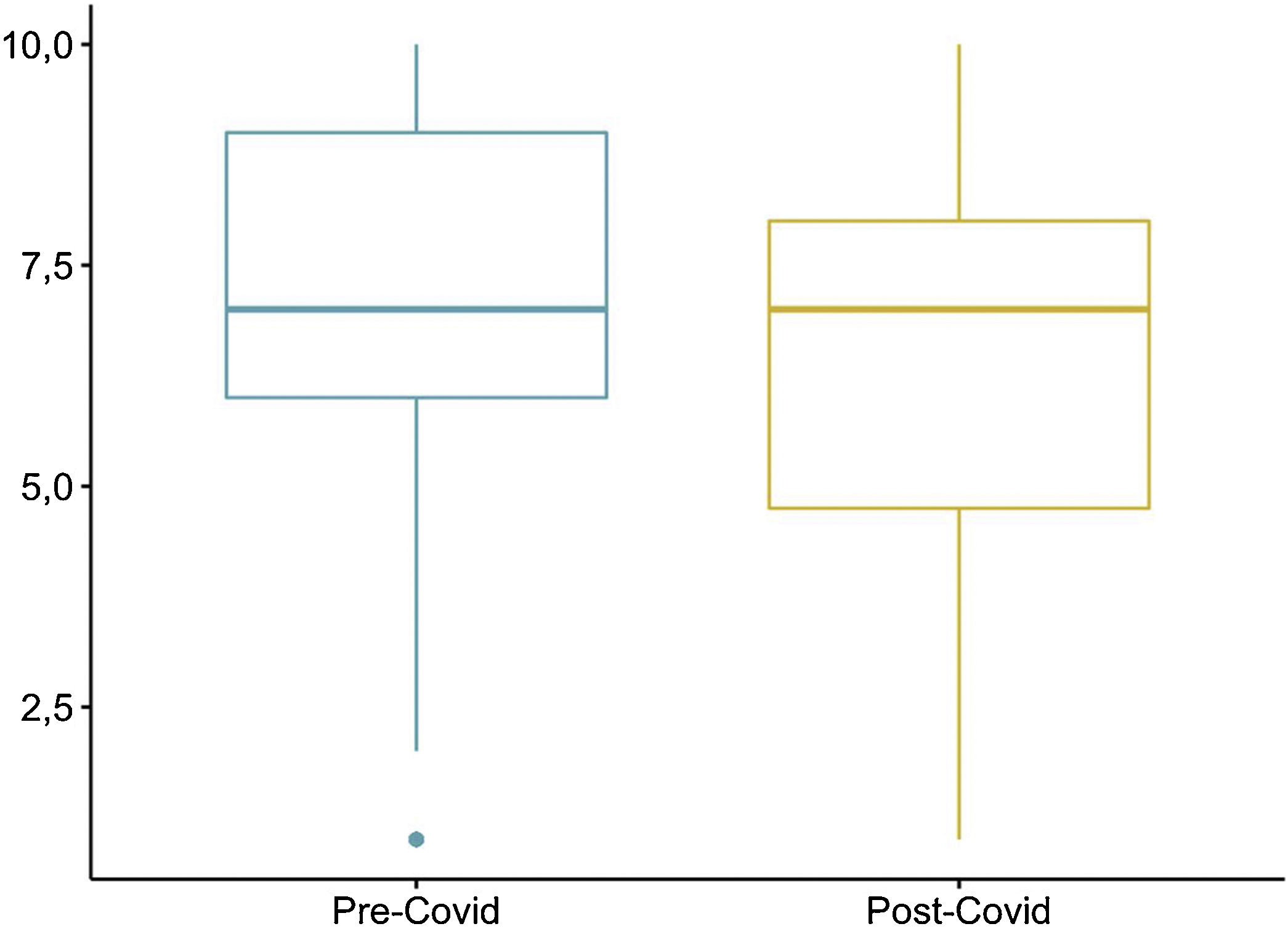
Hospital adherence to ERAS protocols, according to respondents, was lower than before the pandemic (Friedman X2 = 56,828, p < 0.05) Fig. 1.
These results, which reflect the personal opinion of respondents, show a decline in adherence to ERAS items, particularly those involving preoperative optimization, including preoperative management of anaemia.
The latest estimates suggest that more than 28 million surgeries were cancelled or postponed during the first wave of the pandemic2. In addition, many specialists involved in ERAS pathways have had to be relocated within their hospital to care for COVID-19 patients. Changes in these multidisciplinary teams may result in decreased adherence to ERAS items, and this has been associated with changes in postoperative outcomes3. Moreover, as our survey shows, adherence to ERAS protocols was already poor before the pandemic.
Our study has limitations: first, the questionnaire collected the respondent’s opinion, not objective data; second, being members of the REDGERM group, the respondents were already interested in ERAS programmes; third, we do not know whether some responders worked in the same centre as others. Furthermore, the dynamic of the questionnaire itself may result in responses that are not sufficiently rigorous, especially the ordinal assessment questions.
This survey shows that the quality of perioperative management in patients who underwent surgery just after the first wave of the COVID pandemic declined significantly, particularly in terms of adherence to ERAS items.
Given the high number of cancelled and postponed surgeries, hospital staff should give priority to optimising healthcare resources. The application of ERAS protocols can be an important tool in the management of the Post COVID-19 Surgical Backlog4.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Declaration of interestThe authors have no conflict of interest to declare
Please cite this article as: Lorente JV, Ripollés-Melchor J, Aldecoa C, Abad-Motos A. Efecto de la primera ola de la pandemia COVID-19 en la aplicación de los protocolos de recuperación intensificada perioperatoria según la percepción de los profesionales sanitarios. Rev Esp Anestesiol Reanim. 2022;69:374–376.