We performed a meta-analysis to assess the effectiveness and safety of tranexamic acid in patients with traumatic brain injury (TBI).
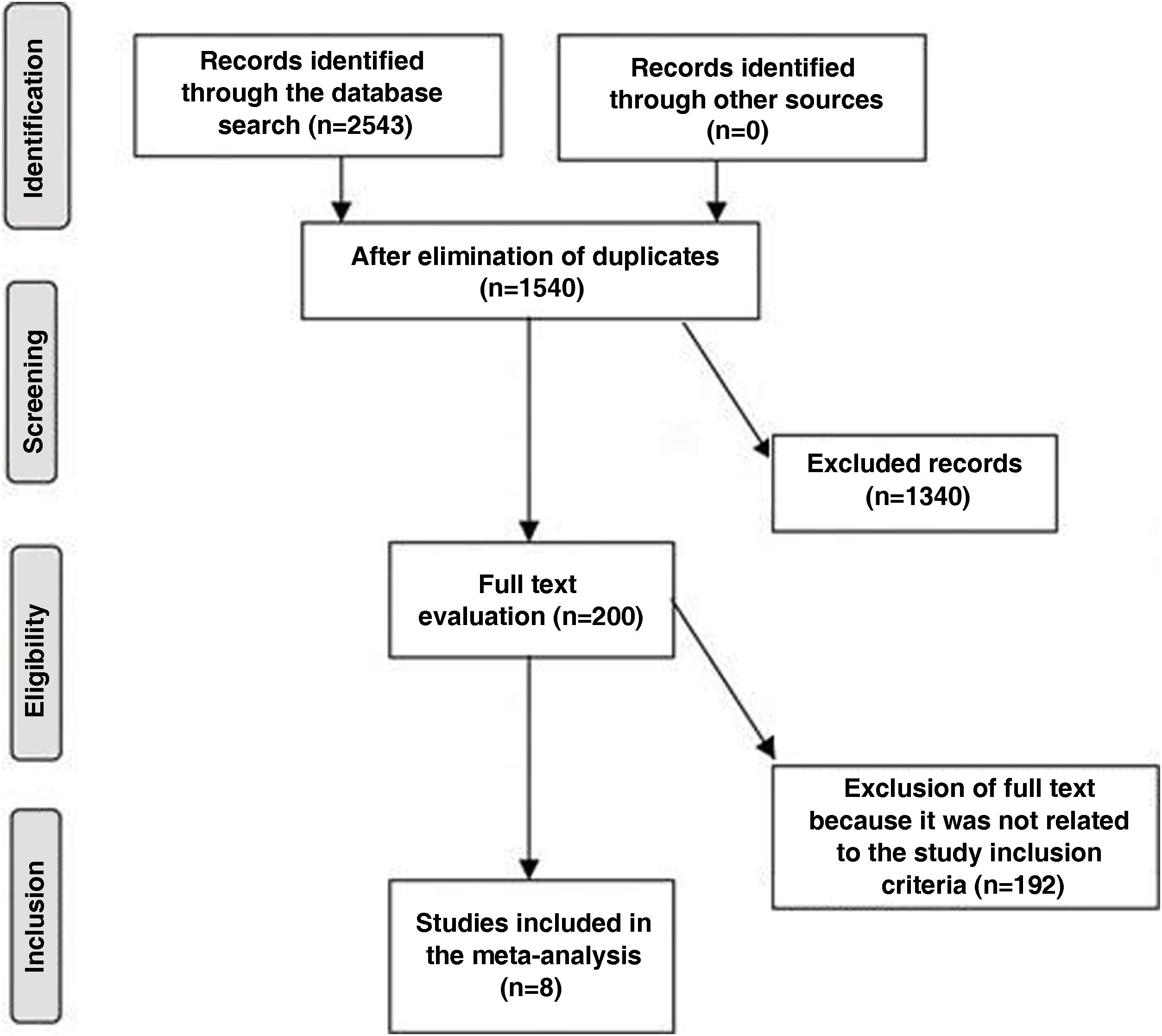
MethodsWe searched the literature for articles evaluating the effectiveness and safety of tranexamic acid (TXA) in TBI published between January 2012 and January 2021, and identified 8 studies with a total of 10860 patients: 5660 received TXA and 5200 served as controls. We used a dichotomous or continuous approach with a random or fixed-effect model to assess the efficacy and safety of TXA in TBI, and calculated the mean difference (MD) and odds ratio (OR) with the corresponding 95% confidence interval.
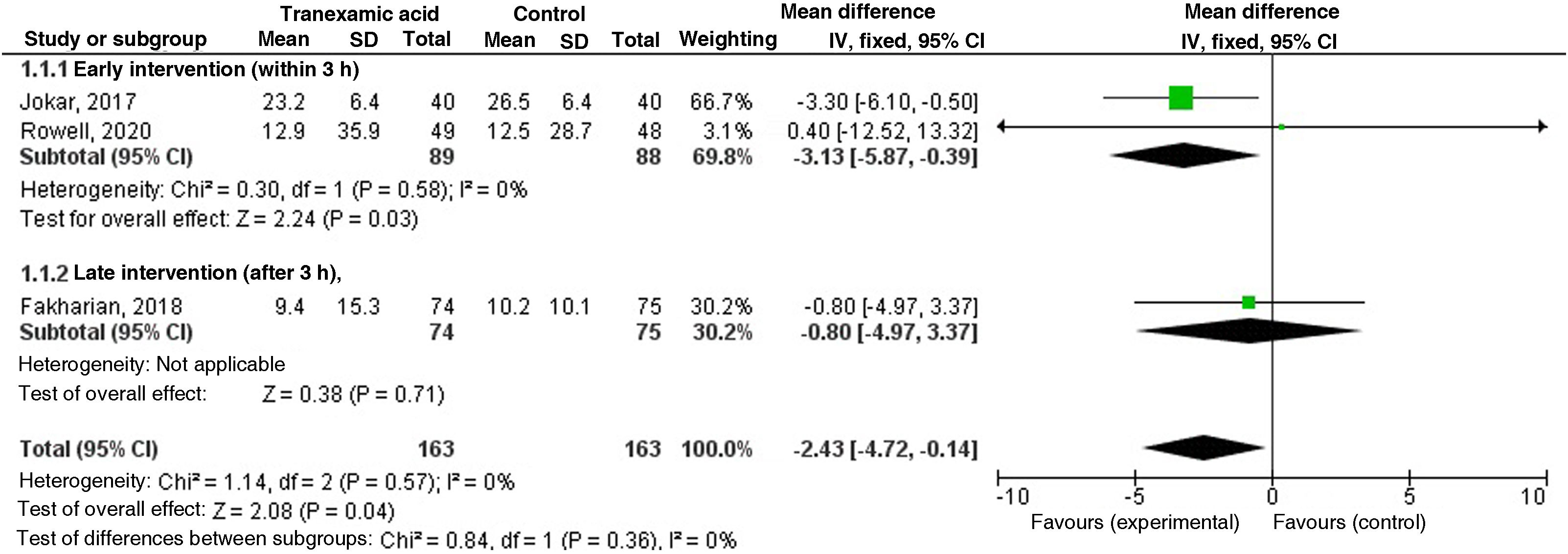
ResultsIn patients with TBI, early administration of TXA was associated with a greater relative benefit (MD −2.45; 95% CI = −4.78 to −0.12; p=0.04) and less total haematoma expansion (MD - 2.52; 95% CI = −4.85 to −0.19; p=0.03) compared to controls.
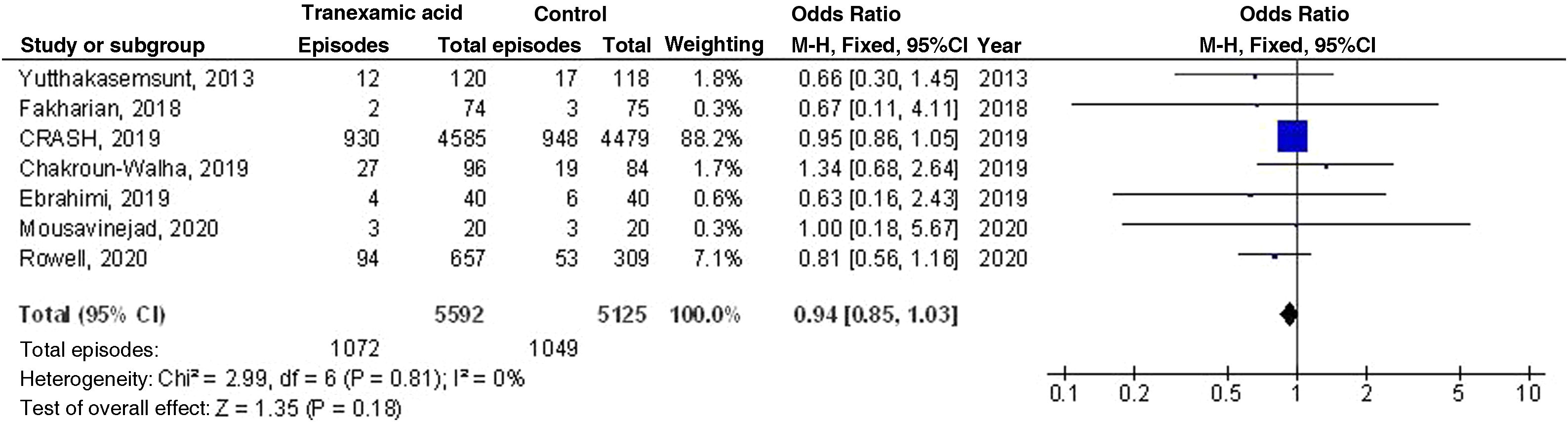
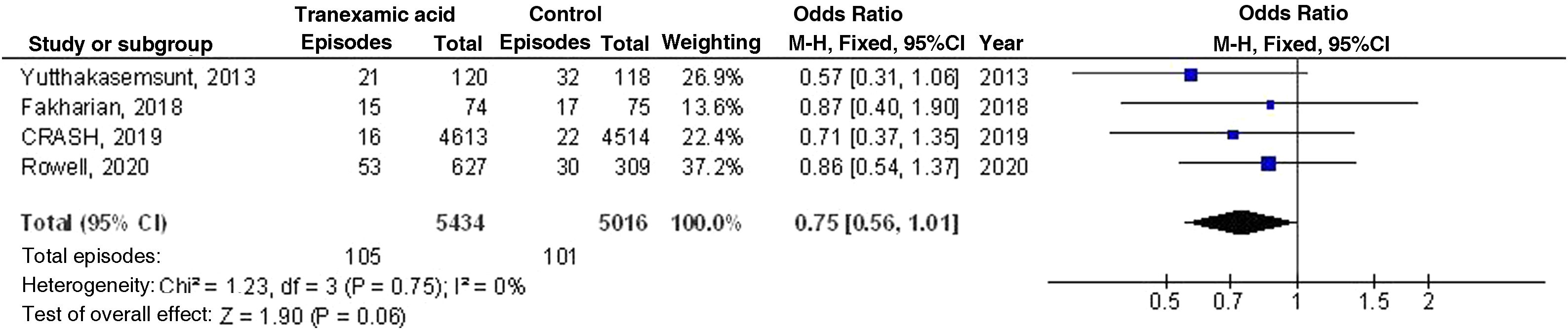
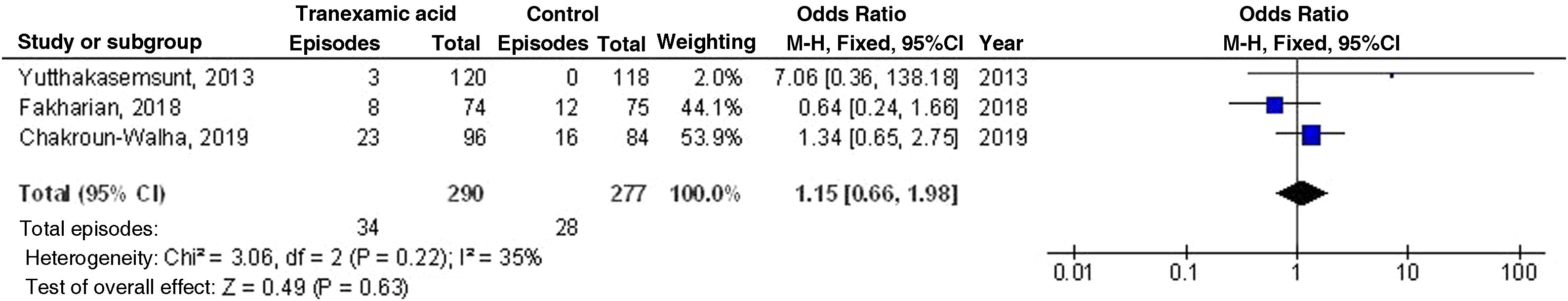
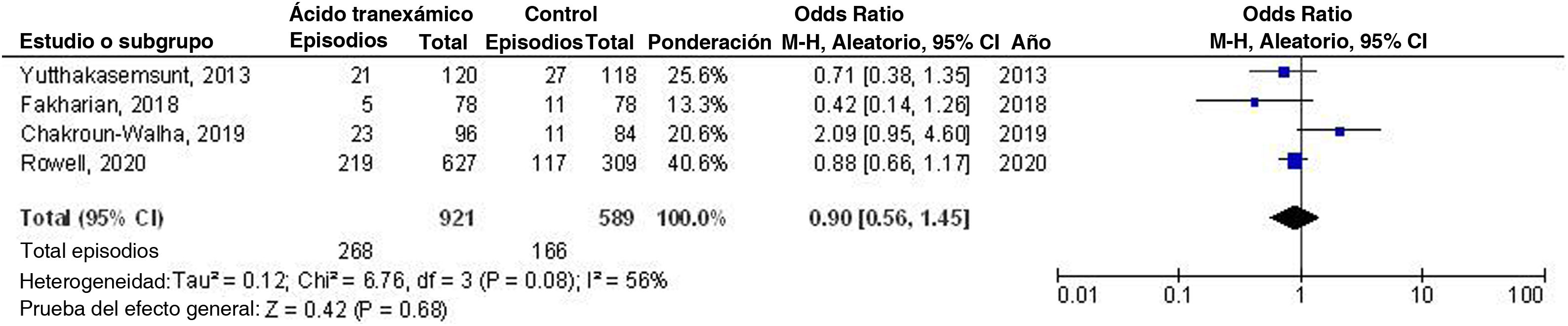
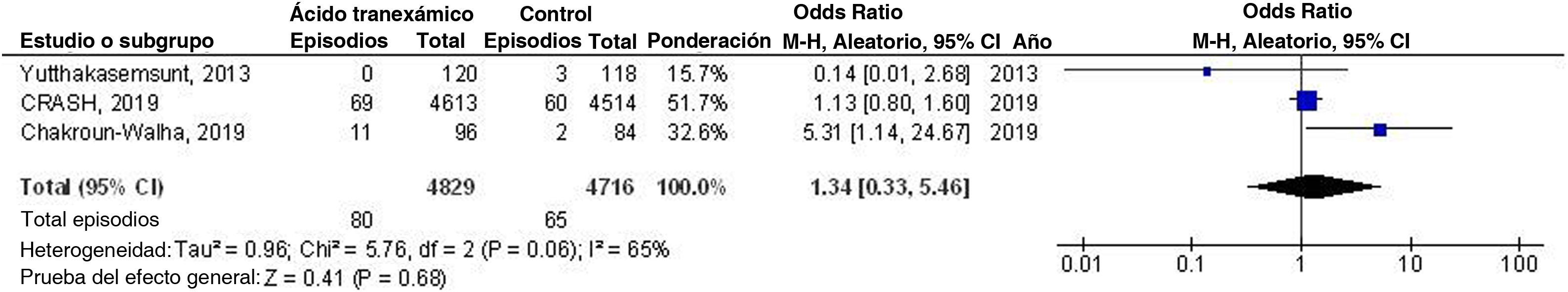
There were no statistically significant differences in mortality (OR 0.94; 95% CI=0.85–1.03; p=0.18), presence of progressive haemorrhage (OR 0.75; 95% CI=0.56–1.01; p=0.06), need for neurosurgery (OR 1.15; 95% CI=0.66–1.98; p=0.63), high Disability Rating Scale score (OR 0.90; 95% CI=0.56–1.45; p=0.68), and incidence of ischaemic or thromboembolic complications (OR 1.34; 95% CI=0.33–5.46; p=0.68) between TBI patients treated with TXA and controls.
ConclusionsEarly administration of TXA in TBI patients may have a greater relative benefit and may inhibit haematoma expansion. There were no significant differences in mortality, presence of progressive haemorrhage, need for neurosurgery, high Disability Rating Scale score, and incidence of ischaemic or thromboembolic complications between TBI patients treated with TXA and controls. Further studies are needed to validate these results.
Realizamos un metaanálisis para evaluar la efectividad y seguridad del ácido tranexámico (ATX) en sujetos con lesión cerebral traumática (TBI).
MétodosEfectuamos una búsqueda minuciosa en la literatura, de enero de 2012 a enero de 2021, e identificamos ocho estudios con un total de 10.860 pacientes al inicio del ensayo: 5.660 recibieron ATX y 5.200 actuaron de controles. Los artículos trataban de la eficacia y seguridad del ATX en los sujetos con TBI. A fin de calcular la diferencia media (DM) y odds ratio (OR) con el correspondiente 95% de intervalo de confianza (IC), utilizamos un enfoque dicotómico o continuo con un modelo de efecto aleatorio o fijo.
ResultadosEl ATX estuvo ligado a una mayor ventaja relativa de la inclusión temprana en las personas con TBI (DM −2,45; IC 95% = −4,78 a −0,12; p=0,04) y a un menor crecimiento total de la lesión hemorrágica (MD, −2,52; IC 95% = −4,85 a −0,19, p=0,03), en comparación con los controles.
Por otro lado, no existió varianza significativa en términos de mortalidad entre los grupos de ATX y control en los sujetos con TBI (OR 0,94; IC 95%=0,85-1,03; p=0,18), hemorragia progresiva (OR 0,75; IC 95%=0,56−1,01; p=0,06), necesidad de neurocirugía (OR 1,15; IC 95%=0,66−1,98; p=0,63), puntuación desfavorable de Disability Rating Scale (DRS) (OR 0,90; IC 95%=0,56−1,45; p=0,68), e incidencia de complicaciones isquémicas o tromboembólicas (OR 1,34; IC 95%=0,33−5,46; p=0,68).
ConclusionesEl ATX en los sujetos con TBI puede tener un mayor beneficio relativo en cuanto a inicio temprano y menor crecimiento de la lesión hemorrágica en comparación con el grupo control. Por el contrario, no existieron diferencias significativas en los grupos de ATX y control en los pacientes con TBI con respecto a la mortalidad, hemorragia progresiva, necesidad de neurocirugía, puntuación desfavorable de DRS e incidencia de complicaciones isquémicas o tromboembólicas Son necesarios estudios adicionales para validar estos resultados.