The development of one-day surgery units has shown to be a better use of health resources without reducing quality. The objective of this study was to evaluate the effectiveness and quality criteria of ambulatory surgery program in the hallux valgus process.
Materials and methodsA retrospective study was conducted on a sample of 754 patients who underwent a hallux valgus process at our institution between 2002 and 2012.
PatientsThe cost-process was evaluated using the Weighted Care Unit (WCU) as a measuring unit. Secondary data were collected as regards discharge criteria and patient satisfaction.
ResultsA significant difference was found between WCU spending on in-patient surgery and out-patient surgery. Both samples were comparable and no differences were found between diagnosis and intervention. The admission rate after ambulatory surgery was 2.29%, and the substitution index increased to 56.04%. The ambulatory surgery program was given a satisfaction rating of 84.6 out of 100.
ConclusionsThe results of our study indicate that it is possible to maximise the substitution index of the hallux valgus process leading to a better use of resources and a high degree of patient satisfaction.
El desarrollo de las unidades de cirugía mayor ambulatoria ha puesto de manifiesto una mejor utilización de los recursos sanitarios sin mermar la calidad de los mismos. El objetivo del trabajo es valorar la eficacia del programa de cirugía mayor ambulatoria en el proceso Hallux valgus y sus criterios de calidad.
Material y métodosSe analizan retrospectivamente todos los pacientes intervenidos del proceso Hallux valgus en nuestro centro entre 2002 y 2012 obteniendo una muestra de 754 pacientes (263 en el grupo de CMA y 461 en el grupo de hospitalización). Se recogen datos relativos al paciente y datos relativos al coste proceso utilizando como unidad de medida la Unidad Ponderada Asistencial (UPA). Secundariamente se recogieron datos en cuanto a criterios de alta y satisfacción de los pacientes.
ResultadosSe encontró una diferencia muy significativa entre el gasto en UPAs de pacientes hospitalizados y los que se intervinieron en CMA. Ambas muestras eran comparables y no se encontraron diferencias demográficas ni de tipos de intervención. El índice de ingreso post CMA fue de 2,39% y el de sustitución creció hasta el 56,04%. Se obtuvo un índice de satisfacción de 84,6 puntos sobre 100 en el programa de cirugía ambulatoria.
ConclusionesLos resultados de nuestro estudio indican que es posible incrementar al máximo el índice de sustitución del proceso Hallux valgus consiguiendo una mejor utilización de los recursos y con un alto grado de satisfacción de los pacientes.
The development of major ambulatory surgery units (MAS) has allowed the reduction of spending and a better use of resources and also provided benefits for patients with conditions requiring little care in the immediate postoperative period. These units arose from a health management reform in the early 80s and are based on a rational use of available resources. They also increase annually, representing 50% of elective surgery in European countries and between 60% and 70% of all interventions in the U.S.A.1–19 One of their main objectives is to reduce hospital stay, which is considered unnecessary in 30% of cases,2 as well as to decrease surgical waiting lists,3 resulting in an effective decrease of their costs.
MAS is defined as healthcare for subsidiary processes of surgery performed under general, regional and local anaesthesia or sedation, requiring little and short intensive postoperative care, thus not requiring hospitalisation and leading to discharge within a few hours of the procedure.4 The main objective of these units is to use resources efficiently whilst combining safety and quality for patients. This task is favoured by significant advances in the fields of anaesthesia and postoperative analgesia, as well as an adequate selection of patients. Maintaining quality in these services is fundamental in MAS processes, with a special emphasis on accessibility, availability of information, efficiency, continuity of care, effectiveness and patient satisfaction.
Orthopaedic surgery without admission has been developed at our hospital from the start of the MAS unit in the early 90s. Processes relating to the foot and originating from deviations of the metatarsals, such as hallux valgus, are a clear example of this type of surgery and as such have experienced an exponential growth since their introduction in our service portfolio.
Following the example of other studies which have concluded that the cost of the hallux valgus process is clearly lower when treated through surgery without admission,20 we conducted a retrospective study comparing the expenditure in weighted care units (WCU) of a sample of patients treated on an outpatient basis against another sample of patients who underwent hospitalisation. We then analysed those variables which could change the attitude when considering the type of admission, regardless of health spending.
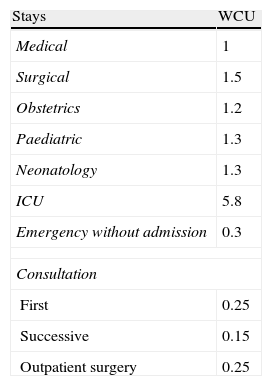
WCU are a measure of health spending which emerged in the late 80s, based on the weighting of different activities taking place at a hospital.21 The objective of this measurement is, once having set a specific value for a given unit, in this case a medical admission, to weigh the value of other activities with respect to it (Table 1). Whilst it is true that the current management model uses other, more precise measures, such as process cost based on Diagnosis Related Groups (DRG), the WCU model is far simpler and we believe it to have sufficient value for the purpose of our study.
Value of stays according to weighted care units.
| Stays | WCU |
| Medical | 1 |
| Surgical | 1.5 |
| Obstetrics | 1.2 |
| Paediatric | 1.3 |
| Neonatology | 1.3 |
| ICU | 5.8 |
| Emergency without admission | 0.3 |
| Consultation | |
| First | 0.25 |
| Successive | 0.15 |
| Outpatient surgery | 0.25 |
ICU: intensive care unit; WCU: weighted care units.
Source: Bestard Perelló et al.21
The main hypothesis of this work is that when the selection criteria for the ambulatory surgery unit are met, it is not efficient to conduct other types of admission. In order to accept or reject this hypothesis we looked for differences regarding complications and readmission rates between the 2 groups mentioned. As secondary objectives, we reviewed the overall rate of outpatient treatment of the centre, our replacement rate for hallux valgus process and the causes for delay of discharge in hospitalised patients.
Materials and methodsWe retrospectively reviewed all patients undergoing hallux valgus process at our hospital, considering a transversal, retrospective, observational study to compare 2 different cohorts of patients. A total of 753 patients were intervened between January 2002 and January 2012, regardless of the type of admission through which they had been included in the surgical waiting list. We excluded 64 patients from the initial sample because the hallux valgus coding diagnosis was not confirmed, so these cases were diagnosed with hallux rigidus. This resulted in a sample of 689 patients. Of these, 251 patients were operated on an ambulatory basis and 438 were admitted to the hospital.
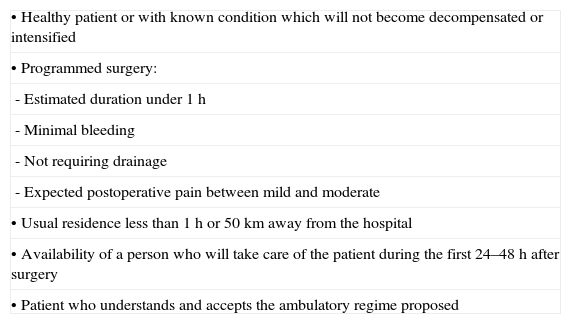
All patients intervened via MAS met the inclusion criteria7,24,25 and accepted the outpatient admission protocol. We applied the criteria of the MAS selection protocol (Table 2) to hospitalised patients in order to homogenise the sample and avoid a selection bias. Thus, we excluded 32 patients from the hospitalised group and obtained a final sample of 657 patients (406 with admission and 251 as outpatients) who did meet the social, personal and morbidity requirements (according to the ASA risk classification) listed in Table 2.
Selection criteria of MAS patients.
| • Healthy patient or with known condition which will not become decompensated or intensified |
| • Programmed surgery: |
| - Estimated duration under 1h |
| - Minimal bleeding |
| - Not requiring drainage |
| - Expected postoperative pain between mild and moderate |
| • Usual residence less than 1h or 50km away from the hospital |
| • Availability of a person who will take care of the patient during the first 24–48h after surgery |
| • Patient who understands and accepts the ambulatory regime proposed |
The following data were collected for each patient: age, gender, diagnosis, anaesthetic risk,26,27 type of intervention and associated healthcare costs measured in WCU.21 For admitted patients we recorded the days of hospital admission and in those cases where this exceeded 1 day we reviewed postoperative medical records to determine the cause of the delay. In the MAS group we identified patients who required admission and the reason for it. We also identified hospital readmissions in both groups.
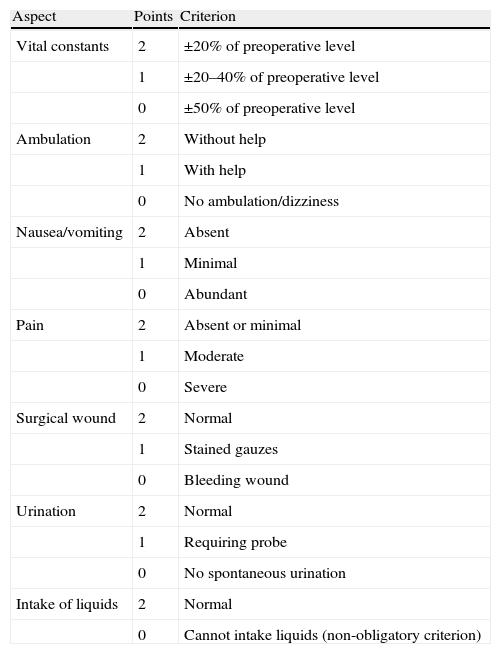
In addition, we collected the scores obtained by MAS patients regarding discharge criteria23 (adaptation of the Chung criteria22 to our environment) (Table 3) and the results of an anonymous satisfaction survey on the quality of the MAS service conducted by the nurses of the unit.24 The anonymous survey consisted of 25 questions with a single, staggered answer covering various aspects of the assistance provided, grouped into 5 key areas: information and connection with the unit, personal comfort, health care, hospitality and overall satisfaction. These responses were automatically transformed into a score, and provided information about the degree of acceptance of each area (minimum score: 0; maximum score: 20) and the overall acceptance through the sum of the 5 areas (minimum score: 0; maximum score: 100).
Criteria for discharge according to Chung.
| Aspect | Points | Criterion |
| Vital constants | 2 | ±20% of preoperative level |
| 1 | ±20–40% of preoperative level | |
| 0 | ±50% of preoperative level | |
| Ambulation | 2 | Without help |
| 1 | With help | |
| 0 | No ambulation/dizziness | |
| Nausea/vomiting | 2 | Absent |
| 1 | Minimal | |
| 0 | Abundant | |
| Pain | 2 | Absent or minimal |
| 1 | Moderate | |
| 0 | Severe | |
| Surgical wound | 2 | Normal |
| 1 | Stained gauzes | |
| 0 | Bleeding wound | |
| Urination | 2 | Normal |
| 1 | Requiring probe | |
| 0 | No spontaneous urination | |
| Intake of liquids | 2 | Normal |
| 0 | Cannot intake liquids (non-obligatory criterion) |
Total score: ≥12 points→discharge; total score: <12 points or some compulsory criterion; 0→admission.
Source: adapted by Jiménez et al.15 Hospital Clínico Universitario Lozano Blesa, Zaragoza. Criteria used upon discharge in the area of readaptation to the environment, to enable house discharge.
We calculated the substitution rate of the hallux valgus process (% [(∑ surgeries performed on an outpatient basis/∑ surgeries conducted through both conventional and ambulatory hospitalisation)]×100) and its evolution during the 10 years covered by the study, as quality criteria. Moreover, as a reference we collected data related to the overall ambulatory index of the centre, calculated as an index in percentage of outpatient sessions/total stay at the centre.
Data analysis was performed using the software package SPSS® v.15.0. We used the Student t test for quantitative variables and the Chi-square test for qualitative variables. We considered a value of P<.05 as significant.
ResultsThe mean age of patients was 60.66 years (range: 19–85; mode: 61) in the ambulatory surgery group compared to 59.81 years (range: 12–86; mode: 61) in the hospital admission group. Regarding gender, we found 16 males and 235 females in the MAS group compared to 27 males and 379 females in the surgery with hospitalisation group. We observed no significant differences in terms of age (P=.353) or gender (P=.656) among the samples.
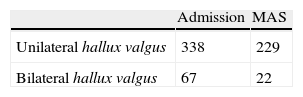
The diagnosis was divided into 2 main groups based on whether the process was unilateral or bilateral. The most common was unilateral hallux valgus (85.2%). We found significant differences between the MAS group and the hospitalised group regarding the distribution between bilateral and unilateral hallux valgus (P=.014), since more bilateral interventions were performed in the group of hospitalised patients (Table 4).
Regarding the anaesthetic risk of patients assessed by the ASA index, the distribution in both groups was homogeneous, with a predominance of ASA ii (76% in the MAS group and 82.2% in the hospitalised group). No statistically significant differences were found between the 2 groups (P=.071).
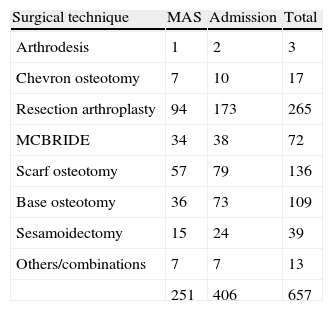
There were various types of interventions based on the severity, age and previous foot function. Scarf osteotomy and Keller–Brandes type resection arthroplasty were the most frequent, but first metatarsal osteotomies (Chevron type, base of the first metatarsal, L-type, Ludloff) were also noted, as were other techniques such as the Regnauld procedure (Table 5). No percutaneous surgery procedures were performed.
Types of intervention.
| Surgical technique | MAS | Admission | Total |
| Arthrodesis | 1 | 2 | 3 |
| Chevron osteotomy | 7 | 10 | 17 |
| Resection arthroplasty | 94 | 173 | 265 |
| MCBRIDE | 34 | 38 | 72 |
| Scarf osteotomy | 57 | 79 | 136 |
| Base osteotomy | 36 | 73 | 109 |
| Sesamoidectomy | 15 | 24 | 39 |
| Others/combinations | 7 | 7 | 13 |
| 251 | 406 | 657 |
MAS: major ambulatory surgery.
Pearson Chi-square; P=.149.
We applied the Chi-square test to assess whether there was a statistically significant difference between surgical techniques depending on the type of admission, and this was not found (P=.149).
Since the results could be influenced by whether surgery was unilateral or bilateral, we statistically compared overall admissions and the presence of unwanted admissions in the MAS group and the initial diagnosis. We found no statistically significant differences in the mean stay of patients who underwent surgery on both feet during the same procedure (P=.837). Moreover, we found no significant differences between the number of admissions after ambulatory surgery depending on whether the intervention had taken place on 1 or 2 feet (P=.765).
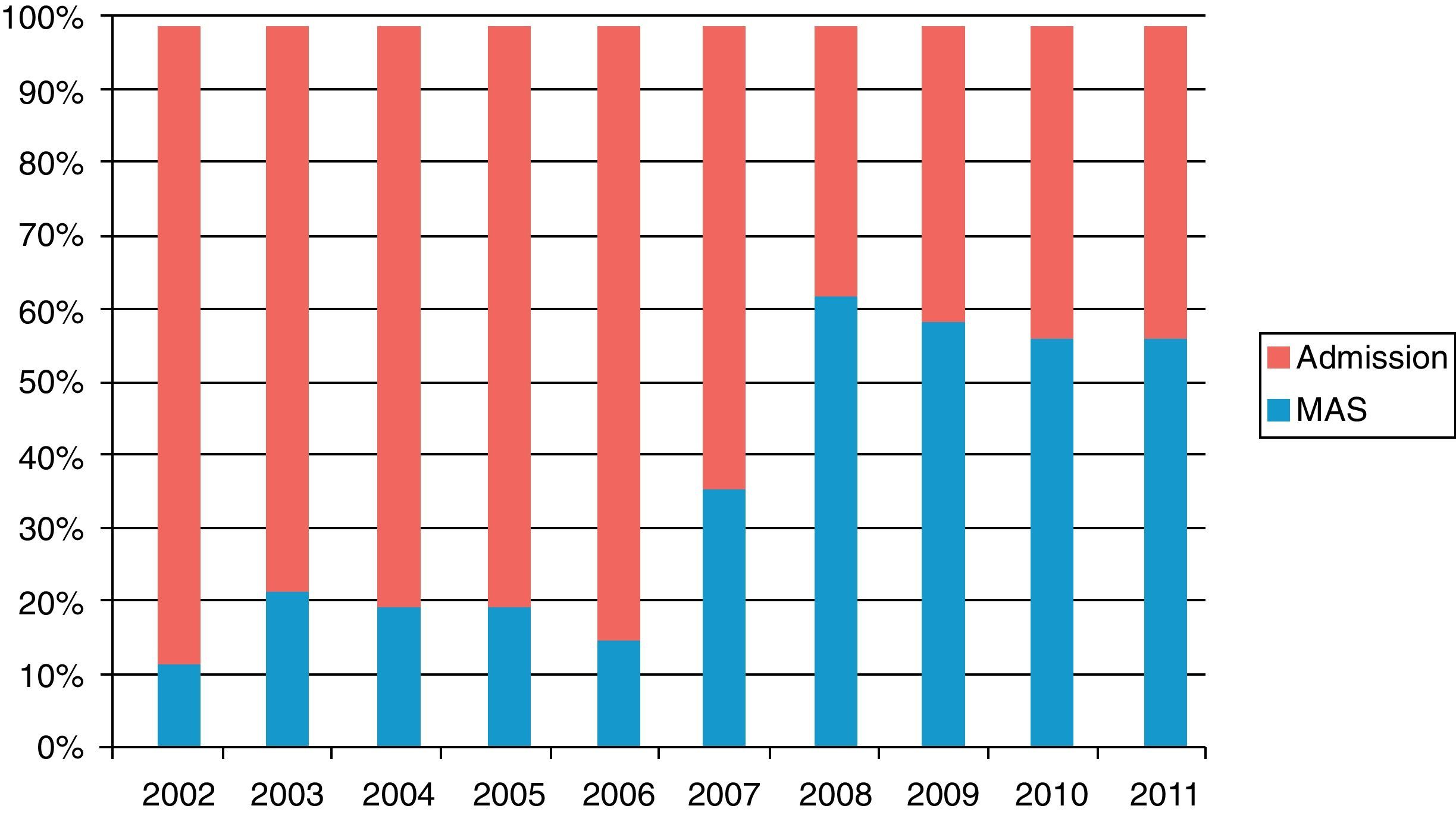
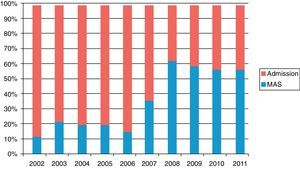
The replacement rate (% [(∑ surgeries performed on an outpatient basis/∑ surgeries conducted through both conventional and ambulatory hospitalisation)]×100), that is, the percentage of hallux valgus intervened at MAS with respect to total hallux valgus cases, increased from 10.52% in 2002 to 56.04% in 2011 (Fig. 1).
The rate of unwanted admissions after MAS (one of the most important quality controls in the outpatient surgery program and one representing a failure of the program) was 6/251 (2.39%). In 4 cases it was due to uncontrollable pain and in 2 cases to dizziness and nausea in the postoperative period. We recorded 9 complications, 2 patients suffered a hypertensive crisis (at 3 and 5 days after the intervention) and 1 suffered paroxysmal tachycardia requiring treatment. One patient suffered a fracture of the second metatarsal of the operated foot. There were 5 complications deriving from the surgical wound, with 2 of these cases requiring deferred hospitalisation for antibiotic treatment of an acute infection. Regarding the number of reoperations, there were 5 in this group (2 cases due to recurrence, 1 case due to infection, 1 case due to removal of material and 1 due to surgical wound granuloma). The median time to reoperation was 10.86 months (range: 1–24 months).
In the inpatient surgery group we noted a mean stay of 3.71 days (range: 1–21; mode: 4). The causes for an extended delay (14 patients) included 1 hypertensive crisis, 1 bradycardia studied by cardiac Holter, 1 cardiac angina and 1 pneumonia in the immediate postoperative period. A total of 9 cases suffered complications due to the surgery, 8 of them caused by wound complications (seroma, necrosis and acute infection) and 1 by acute osteosynthesis failure. In this group we identified 9 reoperations, 2.22% of the sample (1 acute due to osteosynthesis failure, 2 due to wound complications, 2 due to removal of osteosynthesis and 4 due to recurrence of the deformity).
We found no statistically significant difference between the number of complications in both groups, with a level of P=.480.
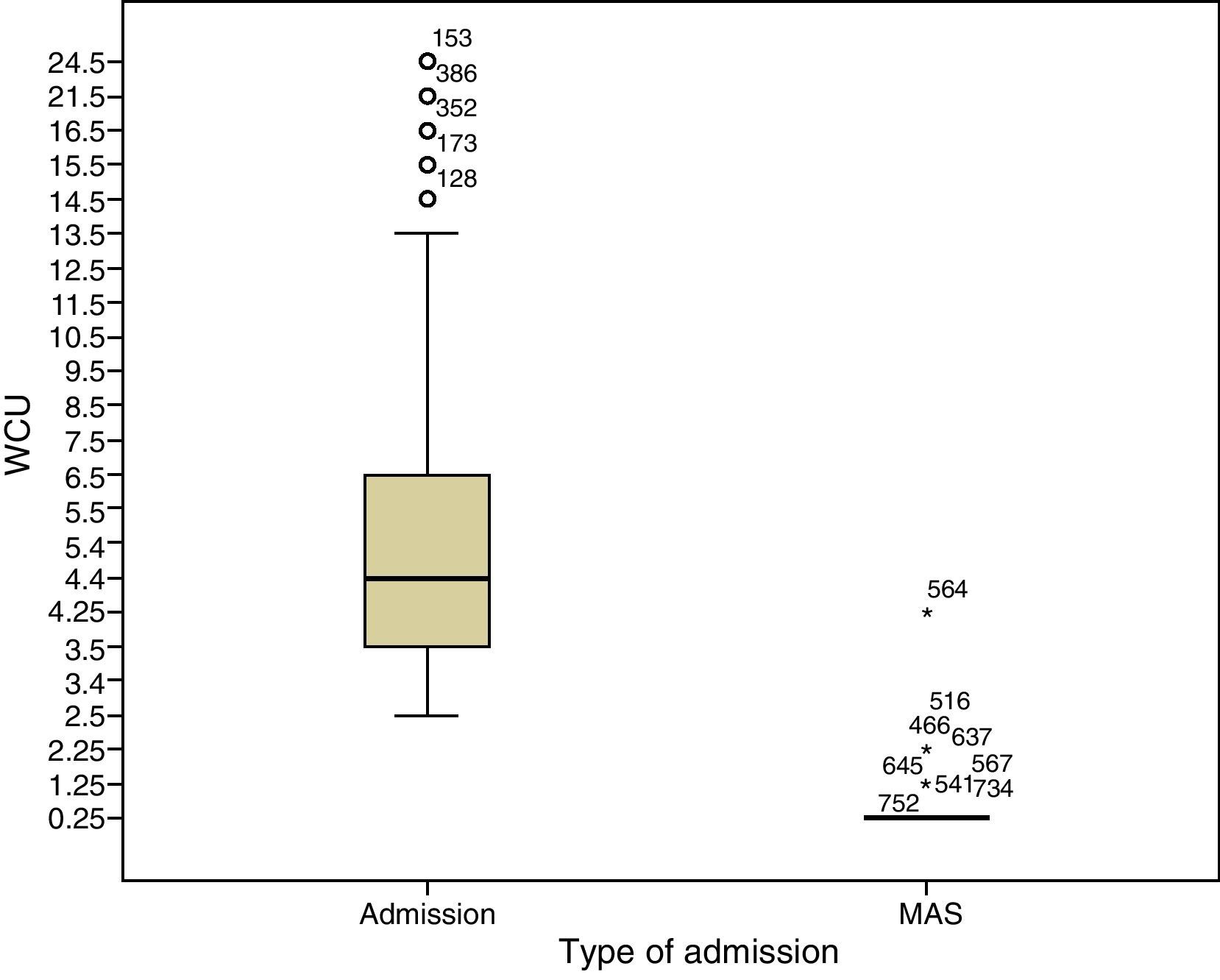
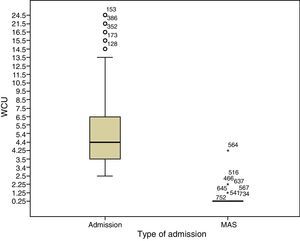
When applying the measurement of weighted care units we observed that the mean value was 0.305 (range: 0.25–4.25; mode: 0.25) in the ambulatory surgery group (6 admissions, 2.39%), compared to 5.19 (range: 2.5–21.5; mode: 3.5) in the hospitalised group. The difference between both means was statistically significant (P=.00001) (Fig. 2). It is important to note that, under normal conditions, inpatient spending would be 2.5 WCU4,5 (1.5 medical units for the operation and 1 medical unit for 1 day of admission) compared to only 0.25 WCU in an ambulatory unit, thus resulting in minimum savings of 2.25 WCU for each process.
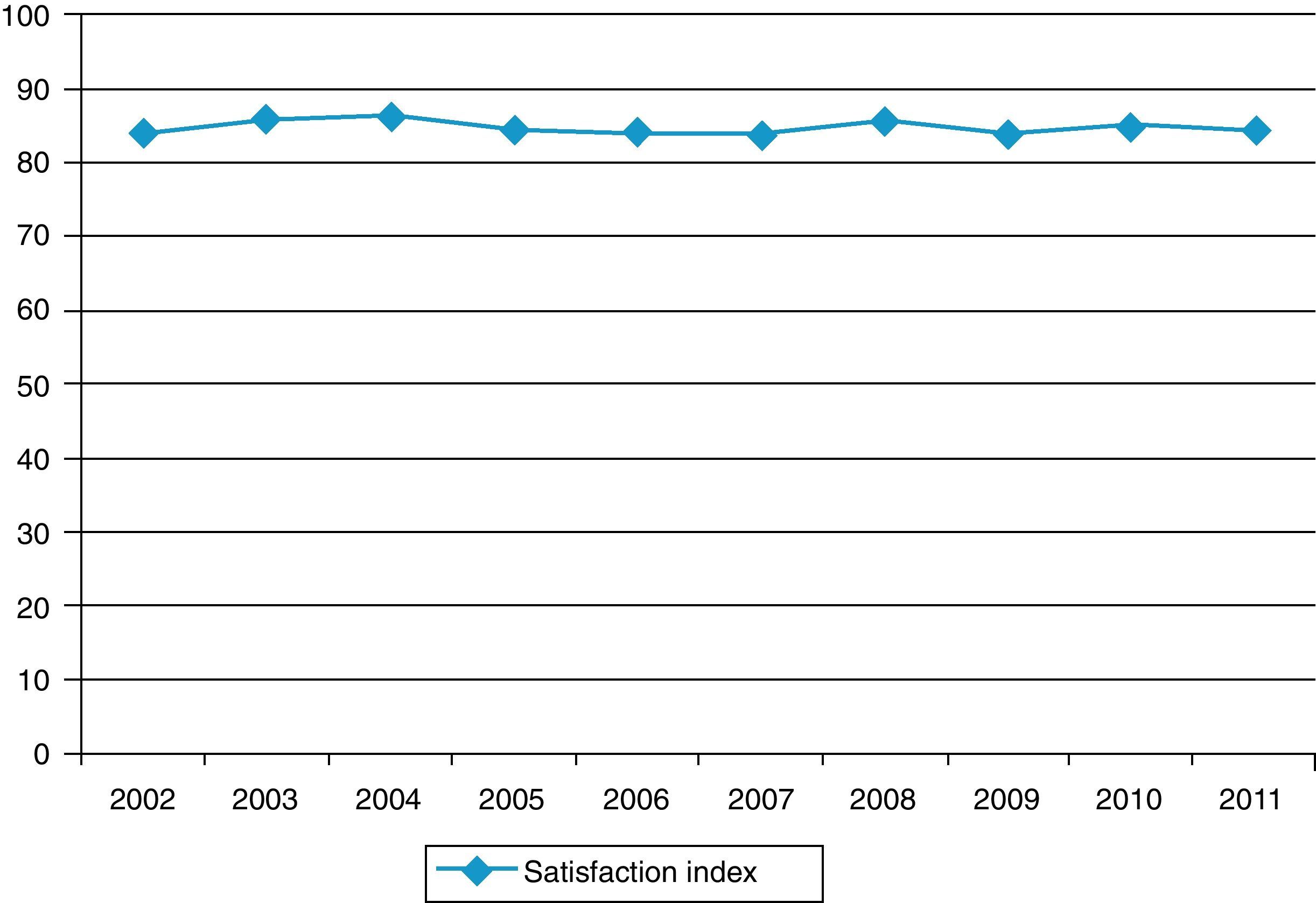
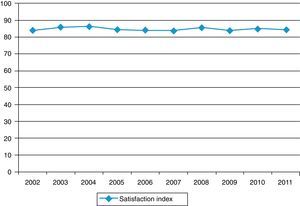
From the point of view of healthcare quality, patient satisfaction with the MAS unit, as measured by the standardised, anonymous survey described in ‘Materials and methods’ section, was 84.1 points out of 100 in 2011. This value remained stable at that level during the entire period considered in this study (mean: 84.64; range: 83.8–86.1) (P=.254) (Fig. 3). We have no record of standardised surveys for the inpatient surgery group, so we cannot provide data on the satisfaction of patients who were operated through that approach.
DiscussionSince their inception over 20 years ago, MAS units have grown progressively.6 Other implications of this growth of outpatient surgery units have been the development of anaesthetic techniques which allow patients to recover in a few hours and a correct selection of those involved in the process.7
The overall rate of ambulatory cases at our centre increased from 14.6% in 2002 to 24.6% in 2011,17 with this index being very sensitive to procedures considered likely to be performed in ambulatory surgery regime. Despite showing a significant increase, it did not reach the mean Spanish value (approximately 40%). In this sense, Redondo Jiménez et al.15 argue that this variability stems from competition by evening programs and the absence of some specialties from the major surgery program. The characteristics of the population in our healthcare area, such as a G3–G4 dispersion grade, a distance of over 100km from the main centre and an aged population may have also exerted a notable influence on the value of this index.
We studied 2 patient samples according to the type of admission employed to perform hallux valgus surgery. The fact that we found no differences regarding gender, anaesthetic risk or in terms of meeting the selection criteria for the ambulatory surgery program, since we excluded patients who underwent surgery during admission but did not comply with the criteria,8 leads us to believe that our patient groups were homogeneous and, hence, comparable. The proportion of unilateral and bilateral diagnoses did show statistical significance (P=.014). We believe that this significance was influenced by the impression that there was an increased risk of complications and higher morbidity among patients who were operated on both feet at the same time. In this regard, Lee et al.10 published a review of 52 patients (69 feet) comparing unilateral and bilateral surgery and concluded that there were no differences in the complications experienced or the satisfaction level of both groups. Other published studies11,28 found no differences in morbidity, complications and reoperation rates, and further concluded that bilateral surgery is economically more efficient. In our series, we did not find a higher rate of complications nor an increased risk of unwanted admissions associated to MAS (P=.837) among patients who had been operated on both feet compared to those who only underwent unilateral surgery.
The replacement rate of the process increased from 10.52% in 2002 to 56.04% in 2011, remaining far from the 100% substitution rate proposed by the Ministry of Health for a condition included in group A of procedures susceptible of being performed via this approach.9 However, there was a progressive advance of replacement and we believe that this could increase even further if the size of the ambulatory surgery unit was increased significantly.
As described in the results section, the mean expenditure on hospitalised patients was 5.19 WCU compared to only 0.305 WCU for an outpatient process. Since, under normal conditions, inpatient spending should be 2.5 WCU,4,5 this figure doubles the estimated expenditure for hallux valgus with inpatient surgery. It is surprising to find that the most common source of delay of discharges in the sample of inpatients was requesting a control radiograph, whereas for outpatients this radiograph was requested during the first postoperative visit. Although at present the most widely used measurement of spending is no longer the WCU and current models are based on process costs associated with DRG, we believe that the hypothesis test is sufficiently innovative as to assess the results obtained as representative, since the measurement is simple and easily understood.
Although an adequate management of health resources is a key aspect for the future of public healthcare, it is imperative that its development runs in parallel with the implementation of quality protocols which prevent a decline of the service.12 We believe that the most important criteria in this respect are admission rates, complication rates and patient satisfaction. In our case, the admission rate which met the MAS discharge criteria was only 2.39%,1 although the literature reports figures for unscheduled admissions between 0.5% and 12%,13 an admission rate less than 5% is generally considered as a quality standard in ambulatory surgery.14,18 Moreover, patient satisfaction in the MAS program was very high, with a satisfaction rate of 84.64 points out of 100. The most commonly identified areas for improvement were preoperative delay and control of postoperative pain.15 Nevertheless, these data may be influenced by the fact that the survey was anonymous and had to be sent by patients after discharge, so it only recorded an average of 51% of all patients.
The observations were not only related to the fact that this model of outpatient surgery generates less disruption in the life of patients, improves personalised care and availability information, thus reducing the stress of surgery, but also to preoperative and postoperative control through telephone surveys conducted by the nursing team of the unit.16 In this sense, adequate patient selection, considering the social and demographic characteristics of each individual, is crucial. In our view, the elements determining patient selection should include the type of process, social factors such as adequacy of housing, presence of company, distance to the hospital under 1h and availability of a telephone and an elevator, as well as psychological factors like understanding of instructions, voluntary acceptance of outpatient treatment and, of course, general status with specific evaluation of any associated conditions. The absence of any of these elements should deter us from including patients in the ambulatory surgery program since, for the first few hours after the intervention, it will be necessary for patients and their companions to take active responsibility for postoperative control and compliance with postoperative instructions and regulations without feeling abandonment.17
Despite the potential limitations of the study, mainly due to it being a retrospective review, the homogeneity of the samples in terms of features, the magnitude of the series and the statistical significance of the results make us believe it possible to propose a progressive increase of the substitution rate of hallux valgus process up to the maximum level permitted by the MAS program selection criteria. In the long term, this would produce a significant decrease in spending associated with hallux valgus without reducing quality of service or patient satisfaction.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Torres Campos A, et al. Coste-efectividad del proceso hallux valgus en cirugía mayor ambulatoria. Rev Esp Cir Ortop Traumatol. 2013;57:38–44.