The Catalonian Arthroplasty Register (RACat) is a public health-based population register used to analyse and evaluate hip and knee replacements in Catalonia. The aim of this study is to present the outcomes after 10 years in operation (January 2005 to December 2014).
MethodologyUsing the information from the RACat and the minimum basic data set at hospital discharge, an analysis was made of the quality and exhaustivity of the data, as well as a descriptive analysis of the patients, prostheses, and care process. Survival was also analysed by calculating the accumulated incidence of revisions (according to the cause of intervention in hip replacements and conservation or sacrifice of the posterior cruciate ligament in knee replacement). The relationship between revision risk and the fixation technique of the prosthesis is also analysed, using competitive risk models adjusted for gender, age, and comorbidities.
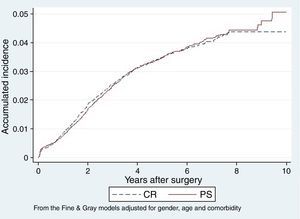
ResultsThe main reason for the primary hip and knee replacement surgery was arthrosis. The accumulated incidence of revisions at 10 years was 3.9% in hip replacements caused by arthrosis, and 2.3% in those caused by fracture. Conservation of the posterior cruciate ligament was achieved in 4.4% of knee replacements, with sacrifice in 5.1%.
DiscussionThe RACat is consolidated as a tool for the evaluation of joint replacements, with great potential in the analysis of medium and long-term efficacy, the study of the variability in clinical practice, and post-marketing surveillance.
El Registro de Artroplastias de Cataluña (RACat) es un registro poblacional basado en el sistema sanitario público para analizar y evaluar artroplastias de cadera y rodilla en Cataluña. El objetivo de este estudio es presentar los resultados tras 10 años de funcionamiento (de enero de 2005 a diciembre de 2014).
MetodologíaA partir de la información del RACat y del conjunto mínimo básico de datos al alta hospitalaria, se analizó la calidad y exhaustividad de los datos y se realizaron análisis descriptivos de pacientes, prótesis y proceso asistencial. Además, se analizó la supervivencia calculando la incidencia acumulada de revisión (según causa de intervención en artroplastias de cadera y preservación o sacrificio del ligamento cruzado posterior en artroplastia de rodilla) y la asociación entre riesgo de revisión y técnica de fijación de las prótesis como modelos de riesgos competitivos ajustados por sexo, edad y comorbilidad.
ResultadosEl principal motivo de intervención en artroplastias primarias de cadera y rodilla fue la artrosis. La incidencia acumulada de revisión a los 10 años fue del 3.9% en artroplastias de cadera causadas por artrosis y del 2.3% en las causadas por fractura. Las artroplastias de rodilla que conservan el ligamento cruzado posterior son el 4,4% y las que no lo conservan, el 5,1%.
DiscusiónEl RACat se consolida como herramienta para la evaluación de las artroplastias con gran potencial en el análisis de la efectividad a medio y largo plazo, el estudio de la variabilidad de la práctica clínica y la vigilancia poscomercialización.
At present, hip and knee replacements are one of the most cost-effective1 medical procedures. Similarly to other countries, due to the increase in degenerative disease resulting from the ageing population and changes in referral criteria, hip and knee replacements significantly increased between in Catalonia between 1994 and 2014.2–5 The increase in these procedures, together with the growing need to provide responses to different clinical research and management issues and the good results from other international expereinces6–8 underlined the need to implement the Catalonian Arthroplasty Register (RACat) 10 years ago.
The hip and knee replacement registers arose as a method for obtaining information about the effectiveness and safety of prostheses following their commercialisation. Although they cannot replace the methodological rigour of clinical trials, they provide long-term safety information,9 and from their results it is possible to identify problems with devices, to be aware of the variability in hospital admittances and the models used in joint replacements, as well as evaluating the survival of the implants and thus the ability to improve healthcare quality and efficacy.3,10,11
The first registers of this type appeared in Scandinavian countries during the 1970s and 1980s—specifically, in 1975 and 1979 Sweden introduced registers of knee and hip replacements, respectively, whilst in Finland and Norway they appeared in 1980 and 1987.4 The satisfactory results obtained in these initial experiences led to the boom of new registers within and outside of Europe.12 According to the Network of Orthopaedic Registries of Europe (NORE) which is a recently founded initiative of the European Federation of National Associations of Orthopaedics and Traumatology (EFORT) and of the International Society of Arthroplasty Registries (ISAR), there are currently over 50 arthroplasty registers worldwide. In Spain there is currently no arthroplasty register within the National health System (NHS). However, the initiative of scientific societies, autonomous communities or of some hospitals themselves has led to the creation of several registers, as is the case of the registers in Andalusia, the Canary Islands, Madrid, the Basque Country and Catalonia.2 These initiatives have not been successful in some cases. At present the Spanish Orthopaedic and Traumatology Society (Sociedad Española de Cirugía Ortopédica y Traumatología “SECOT”) is exploring and leveraging for the possibility of establishing a state register.
The RACat came into being from the common interest of the Catalan Health Service (CatSalut), the Catalan Orthopaedic and Traumatology Society (Sociedad Catalana de Cirugía Ortopédica y Traumatología “SCCOT”) and the Agència de Qualitat i Avaluació Sanitàries de Catalunya (AQuAS), which signed a collaborative agreement in 2005 aimed at developing a joint replacement register. The AQuAS was the entity appointed to carry out the project.2,5 Continuous analysis of data included in the register have led to follow-up, analysis and comparison of RACat results with those of other international registers and also to the observation of the gradual evolution in joint replacement quality and efficiency in Catalonia.3,9,11
The aim of this study is to present the outcomes after 10 years in operation, evaluate the quality and exhaustivity of data, describe the patient characteristics and interventions included, and to assess the survival of the prostheses used, within the framework of the RACat.
MethodologyData managementPrimary and revision hip and knee replacement information recorded in the RACat from January 2005 until December 2014 was used in this study. This information was provided by 53 of the 61 Integral Public Health System centres of Catalonia (SISCAT), which represent over 85% of all public activity executed.
By using a CatSalut IT application, the hospitals sent RACat data on patients, prostheses, surgical intervention and technique. The RACat information and data collection system was designed to involve the minimum workload possible for the Orthopaedic and Traumatology Surgical Services, and also to guarantee the data protection of the people who underwent surgery by using anonymity, in accordance with prevailing law.
From patient identifying data, the register data was linked with that of the Central registry of Insured Persons, from which the vital state of the patient was obtained, and with this the basic minimum dataset of hospital discharge (CMBDAH). Information was thus obtained on the reason for the intervention, the procedures undertaken and comorbidities. The RACat has also produced a catalogue of prostheses from the information provided by the manufacturers and distributors. This catalogue was able to complete the implant information that the hospital sent to RACat (manufacturer's name, reference number, batch of all implanted components and cement used), and also identify the type of component, attachment technique, friction torque (in total hip replacements) and models of the implanted prostheses.
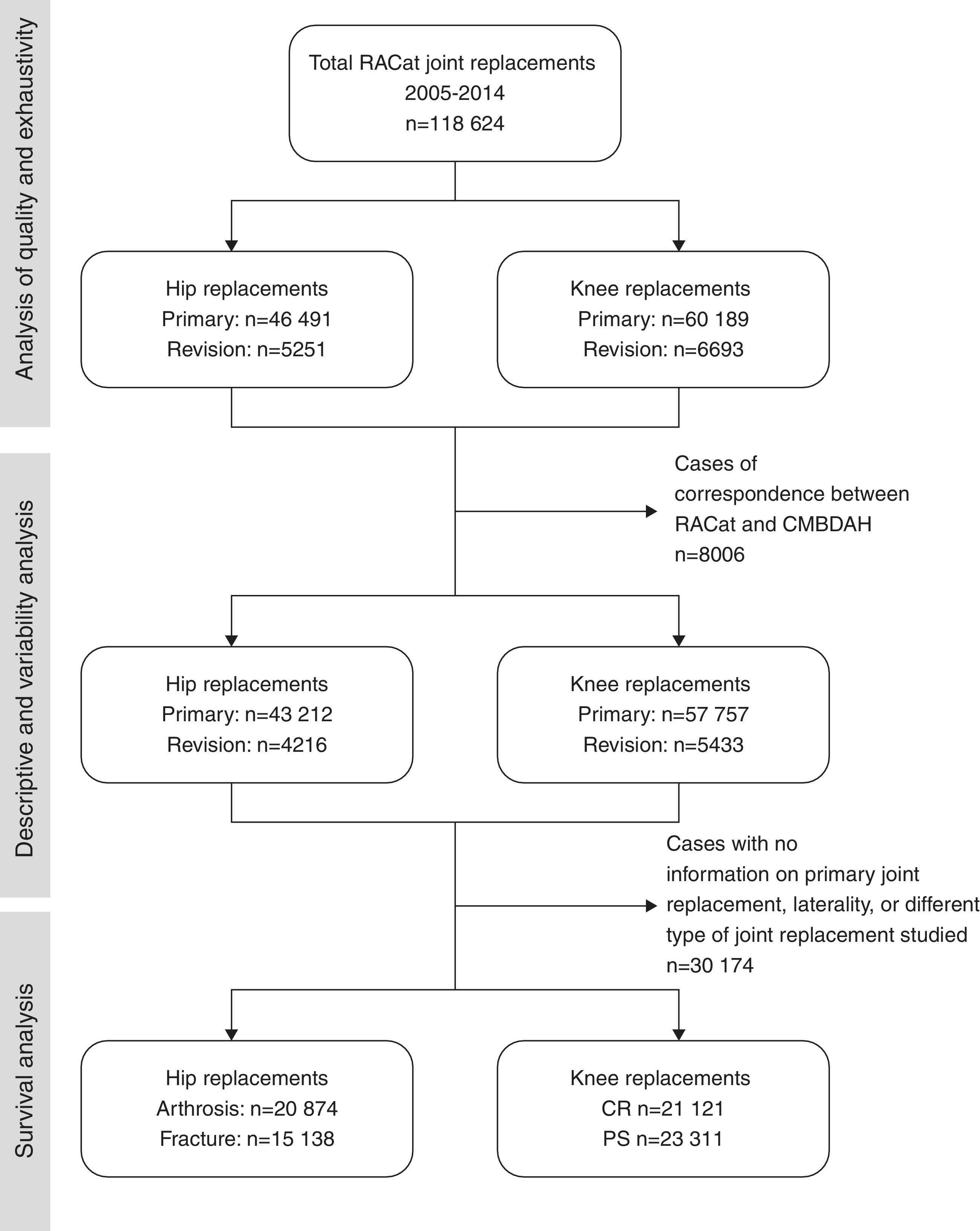
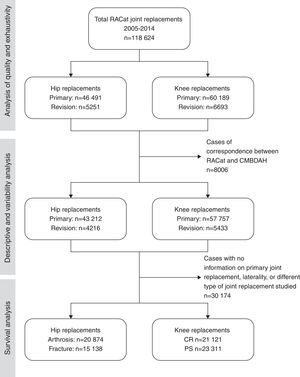
Study sampleAll patients of primary and revision hip and knee replacements performed in public hospitals in Catalonia who sent information to RACat during the 2005–2014 period were included in this study. From the total joint replacements included in the RACat, different inclusion and exclusion criteria were used to select the study sample, in keeping with each of the specific study objectives (Fig. 1).
All the information from the RACat and the CMBDAH was taken into account in order to analyse the quality of the data and the exhaustivity of the information. To this end, all insured persons from the CatSalut who had undergone a knee or hip replacement in a RACat (N=118,624) participating centre between January 2005 and December 2014 were considered for analysis: these included 51,742 hip replacements and 66,882 knee replacements.
For the purposes of descriptive analysis all those cases between 2005 and 2014 where there was some consistency between the RACat and CMBDAH data were selected. 6.8% of cases were excluded due to their lack of consistency. A total of 110,618 replacements (47,428 hip and 61,565 knee) were studied.
For its part, for the survival analysis data, apart from that which was not interlinked between the RACat y el CMBDAH, those cases where the type of knee prostheses did not coincide with posterior-cruciate ligament retainment (CR) or sacrifice (PS), those where the reason for intervention in hip replacements was not arthrosis or fracture, those cases where the location (right or left) could not be determined, and those cases where there was information on the revision surgery but not primary surgery were all rejected. A total of 36,012 hip replacements and 44,432 knee replacements were considered for this analysis.
Data analysisAnalysis undertaken for our study was structured into three areas in accordance with the proposed objectives: quality and exhaustivity of data, descriptive analysis and survival analysis.
Firstly, to assess the quality of the data we undertook analysis of the volume of interventions and exhaustivity, considering the ratio to be between the volume of arthroplasties sent to the RACat and the volume of arthroplasties sent to the CMBDAH (RACat benchmark) by the participating centres. Exhaustivity differentiated between primary hip and knee interventions and revision joint replacements.
Secondly, a descriptive analysis of the frequencies and percentages of both the patient characteristics and the healthcare process was undertaken. Descriptive analysis was also made of the frequency and percentage of the different types of prostheses and fixation, the number of prosthesis models implanted and the variability of use in the different hospitals, with the preparation of graphs to compare joint the replacement volume and diversity of models used in each hospital.
Lastly, survival analysis was performed by considering the time elapsed from primary to revision arthroplasty, regardless of the reason. The accumulated revision incidence was calculated from the competitive risk Fine and Grey models,13 and subhazard ratios (SHR) were calculated together with 95% confidence intervals (95% CI) to analyse the association between the type of prosthesis fixation attachment and risk of revision. The death of a patient by any cause was considered as a competitive risk or event occurring prior to the end of the study period, and which prevented the event of interest (in this case, revision) from taking place.
For survival analysis, analysis was carried our separately depending on the diagnosis (arthrosis/fracture) in hip replacements and according to whether they the posterior-cruciate ligament had been retained or sacrificed in knee replacements (taking into considerations types CR and PS). Statistical significance was fixed at α<0.05. All models were adjusted for age (classified into the following groups: <65 years of age, 65–74, 75–84 and >84 years of age), gender and comorbidities considered from the Elixhauser index, which evaluates the comorbidity prior to surgery and is used in large data volumes.14 All data analysis was performed with STATA version 14.0 software.
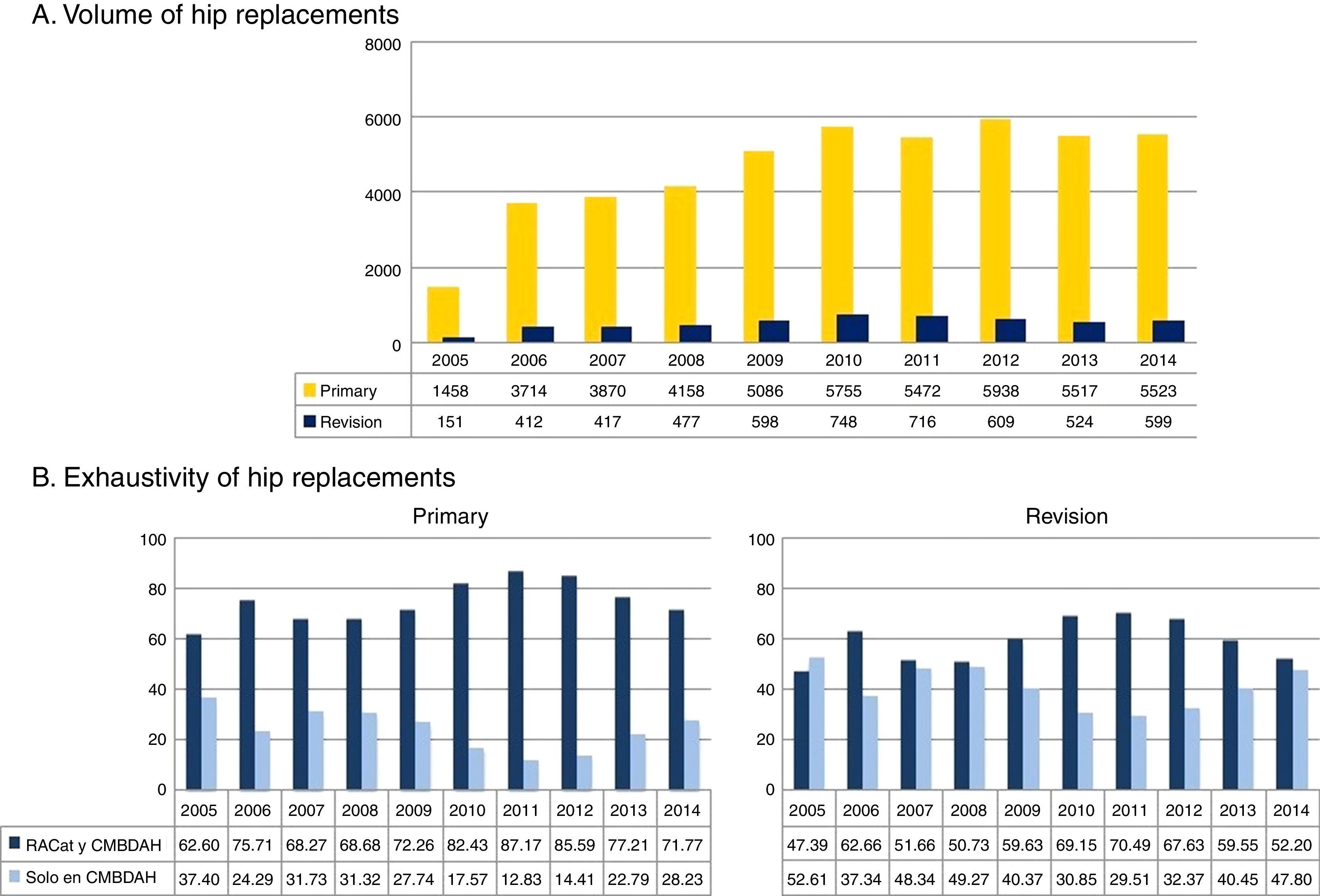
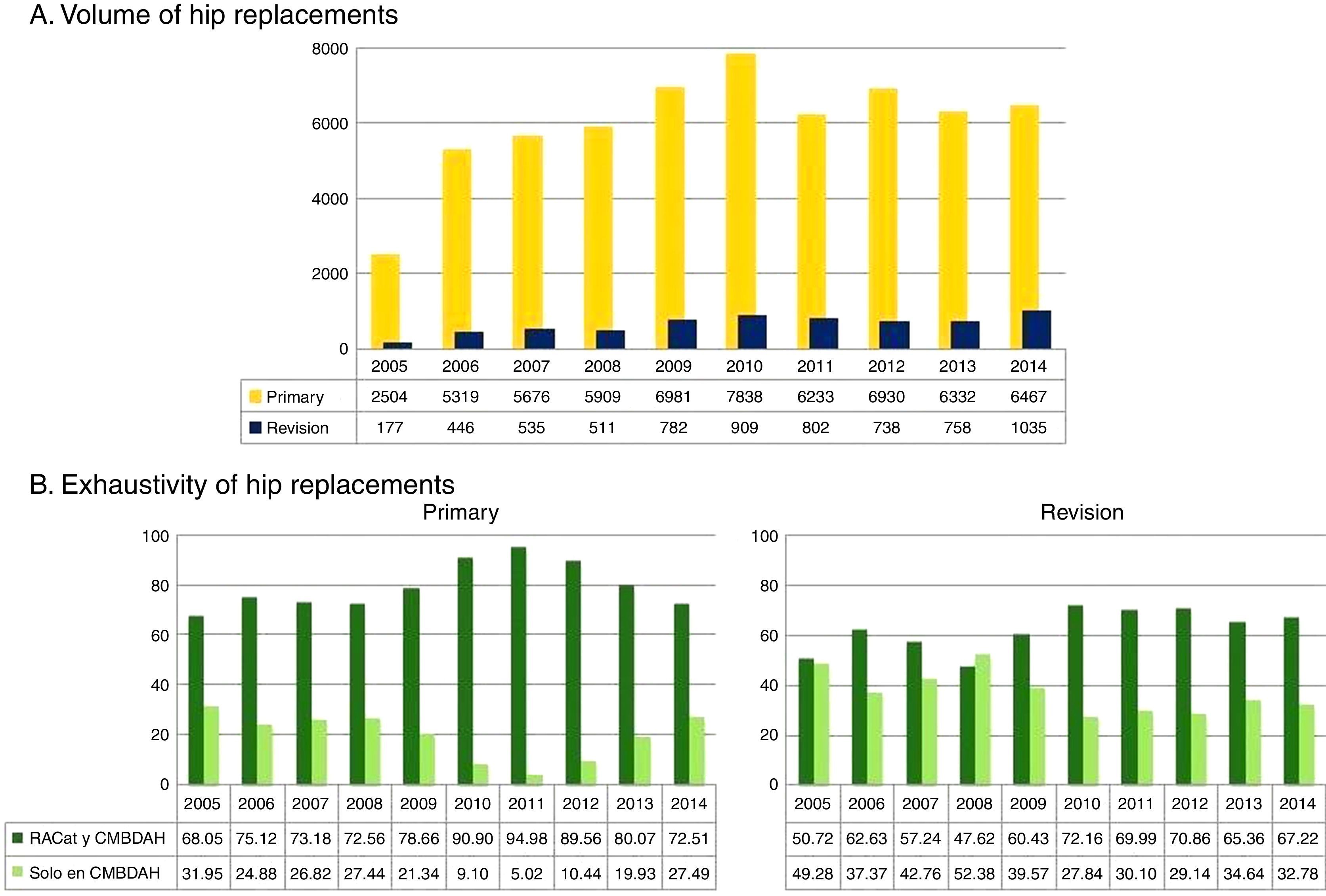
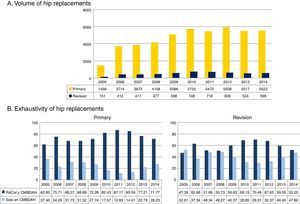
ResultsHip replacementsQuality of the data: volume of surgical interventions and exhaustivityAn upward pattern in the number of primary and revision hip replacements registered to RACat was observed over the 10 years of the register's existence (Fig. 2A). The highest number of primary hip interventions took place in the year 2012, when over 6000 interventions were performed, whilst in 2011 a sudden fall was observed.
(A) Evolution of the number of primary and revision hip replacements. (B) Evolution of data exhaustivity in primary and revision hip replacements in the RACat (2005–2014). CMBDAH: conjunto mínimo básico de datos al alta hospitalaria (minimum basic dataset at hospital discharge) RACat: Registro de Artroplastias de Cataluña (Catalan Arthroplasty Register).
With regards to exhaustivity (Fig. 2B), it was observed that the number of RACat cases in which correspondence with the CMBDAH data could be established increased at the beginning of the register up until 2012, when a drop was observed. In the year 2014, exhaustivity of 71.7% was observed in primary joint replacements and of 52.2% in revision joint replacements.
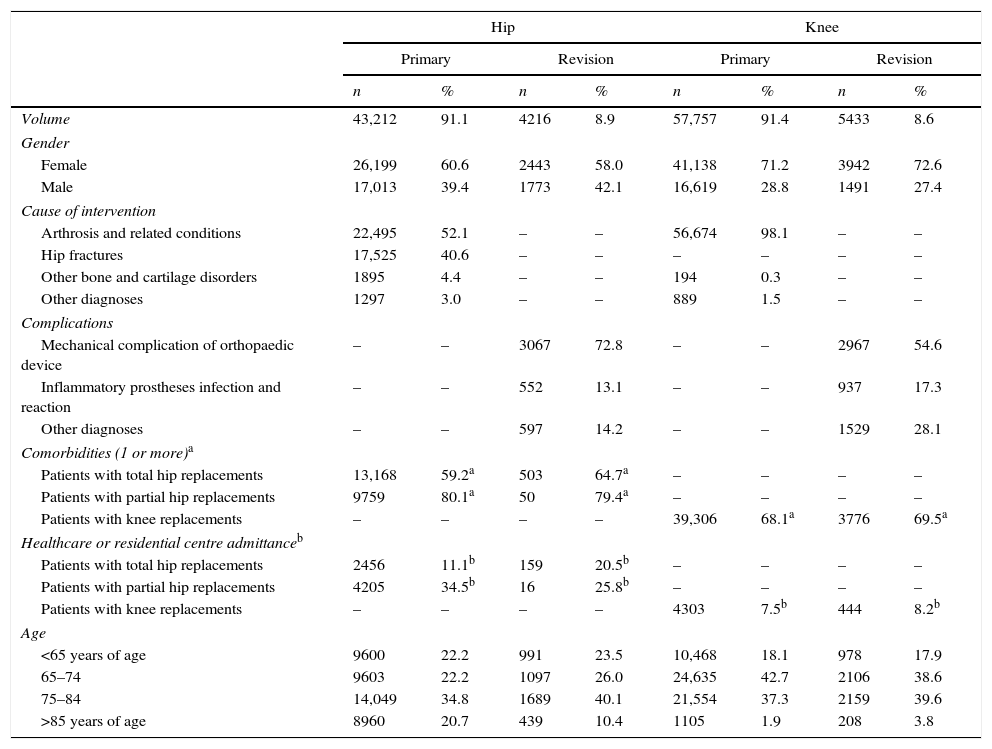
Descriptive analysisPatients and healthcare processAs may be observed in Table 1, a higher number of hip replacements were performed in women than in men (60.6%). Arthrosis was the cause of intervention for 52.1% of primary arthroplasties and fracture for 40.6%. The most frequent reason for revision were mechanical complications of the orthopaedic device (72.8%) and over half the patients presented with one or more comorbidities. Lastly, patients with partial hip arthroplasties presented with a higher percentage of admission to healthcare or residential centres (34% primary and 25.8% revision) than those with total joint replacements (11.1% primary and 20.5% revision).
Descriptive characteristics of the patients and healthcare process according to type of joint and joint replacement in the RACat 2005–2014.
| Hip | Knee | |||||||
|---|---|---|---|---|---|---|---|---|
| Primary | Revision | Primary | Revision | |||||
| n | % | n | % | n | % | n | % | |
| Volume | 43,212 | 91.1 | 4216 | 8.9 | 57,757 | 91.4 | 5433 | 8.6 |
| Gender | ||||||||
| Female | 26,199 | 60.6 | 2443 | 58.0 | 41,138 | 71.2 | 3942 | 72.6 |
| Male | 17,013 | 39.4 | 1773 | 42.1 | 16,619 | 28.8 | 1491 | 27.4 |
| Cause of intervention | ||||||||
| Arthrosis and related conditions | 22,495 | 52.1 | – | – | 56,674 | 98.1 | – | – |
| Hip fractures | 17,525 | 40.6 | – | – | – | – | – | – |
| Other bone and cartilage disorders | 1895 | 4.4 | – | – | 194 | 0.3 | – | – |
| Other diagnoses | 1297 | 3.0 | – | – | 889 | 1.5 | – | – |
| Complications | ||||||||
| Mechanical complication of orthopaedic device | – | – | 3067 | 72.8 | – | – | 2967 | 54.6 |
| Inflammatory prostheses infection and reaction | – | – | 552 | 13.1 | – | – | 937 | 17.3 |
| Other diagnoses | – | – | 597 | 14.2 | – | – | 1529 | 28.1 |
| Comorbidities (1 or more)a | ||||||||
| Patients with total hip replacements | 13,168 | 59.2a | 503 | 64.7a | – | – | – | – |
| Patients with partial hip replacements | 9759 | 80.1a | 50 | 79.4a | – | – | – | – |
| Patients with knee replacements | – | – | – | – | 39,306 | 68.1a | 3776 | 69.5a |
| Healthcare or residential centre admittanceb | ||||||||
| Patients with total hip replacements | 2456 | 11.1b | 159 | 20.5b | – | – | – | – |
| Patients with partial hip replacements | 4205 | 34.5b | 16 | 25.8b | – | – | – | – |
| Patients with knee replacements | – | – | – | – | 4303 | 7.5b | 444 | 8.2b |
| Age | ||||||||
| <65 years of age | 9600 | 22.2 | 991 | 23.5 | 10,468 | 18.1 | 978 | 17.9 |
| 65–74 | 9603 | 22.2 | 1097 | 26.0 | 24,635 | 42.7 | 2106 | 38.6 |
| 75–84 | 14,049 | 34.8 | 1689 | 40.1 | 21,554 | 37.3 | 2159 | 39.6 |
| >85 years of age | 8960 | 20.7 | 439 | 10.4 | 1105 | 1.9 | 208 | 3.8 |
%: percentage compared with the total; SD: standard deviation; n: total number from 2005 to 2014 period.
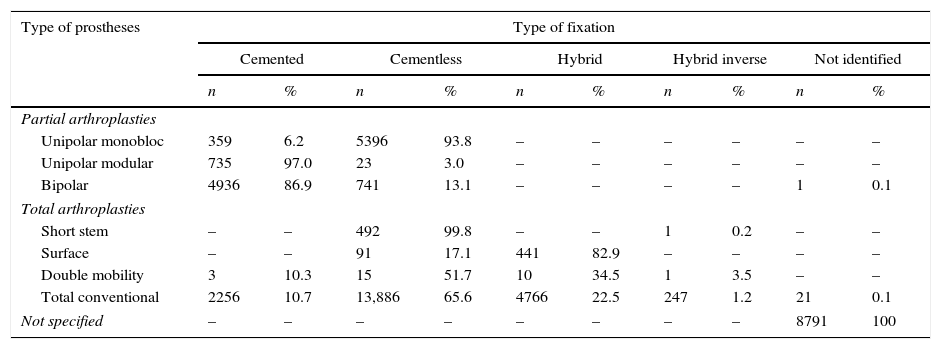
Table 2 lists the type of joint replacements according to the fixation technique for hip prostheses. For partial prostheses the most standard types were the monobloc unipolar and the bipolar types. For the majority of monobloc unipolar prostheses cementless fixation was used (93.8%), whilst for 86.9% of bipolar prostheses cemented fixation was used. With regard to total hip replacements, the most standard type was the total conventional and the most common type of fixation of the prostheses was cementless.
Frequency of type of prosthesis and fixation technique in hip replacements included in the RACat (2005–2014).
| Type of prostheses | Type of fixation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cemented | Cementless | Hybrid | Hybrid inverse | Not identified | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| Partial arthroplasties | ||||||||||
| Unipolar monobloc | 359 | 6.2 | 5396 | 93.8 | – | – | – | – | – | – |
| Unipolar modular | 735 | 97.0 | 23 | 3.0 | – | – | – | – | – | – |
| Bipolar | 4936 | 86.9 | 741 | 13.1 | – | – | – | – | 1 | 0.1 |
| Total arthroplasties | ||||||||||
| Short stem | – | – | 492 | 99.8 | – | – | 1 | 0.2 | – | – |
| Surface | – | – | 91 | 17.1 | 441 | 82.9 | – | – | – | – |
| Double mobility | 3 | 10.3 | 15 | 51.7 | 10 | 34.5 | 1 | 3.5 | – | – |
| Total conventional | 2256 | 10.7 | 13,886 | 65.6 | 4766 | 22.5 | 247 | 1.2 | 21 | 0.1 |
| Not specified | – | – | – | – | – | – | – | – | 8791 | 100 |
%: Percentage compared with the total; cemented; cemented stem and socket component; hybrids, cemented stem and cementless socket; inverse hybrids: cementless stem and cemented socket; n: total number; cementless: no cemented component.
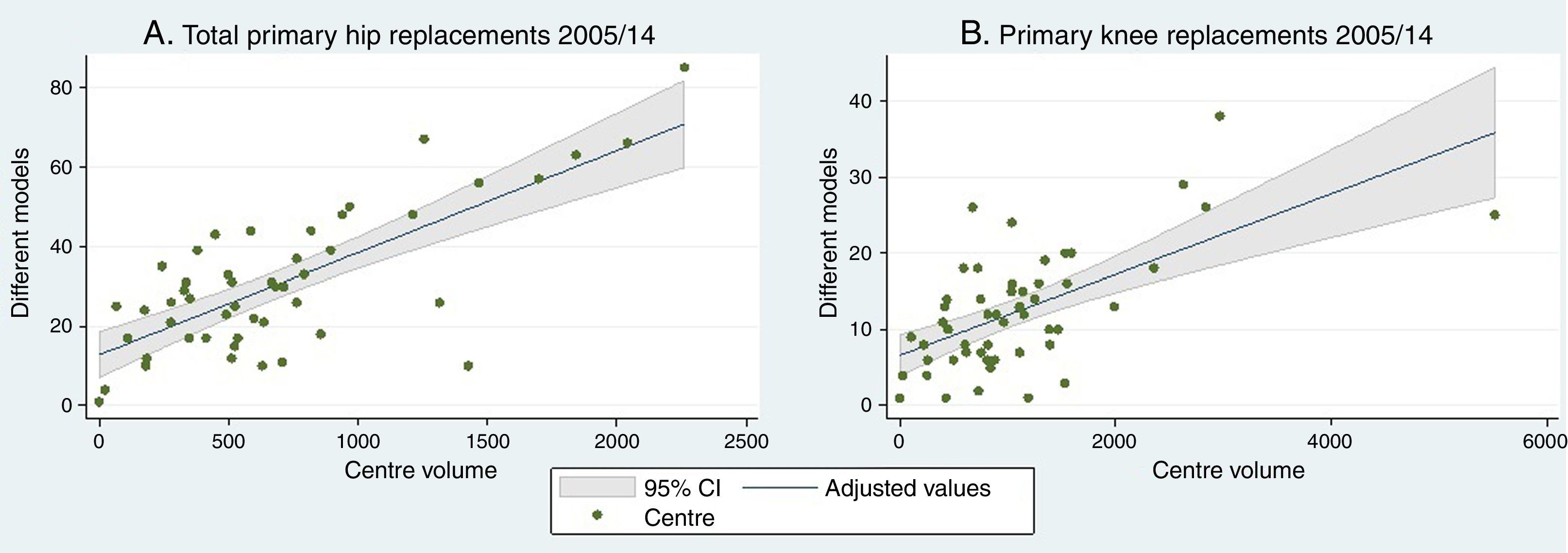
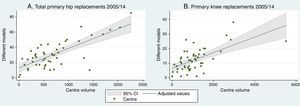
Fig. 3A shows the variability in the use of different models of prostheses in the hospitals participating in the RACat. In the figure, each hospital centre is represented by a point. In general, a tendency to use a higher number of models is observed (vertical axis) as the volume of arthroplasties performed in the hospital (horizontal axis) increases.
In primary total hip replacements the number of socket models used in hospitals was between 1 and 34 different types, with an average of 16 per hospital. Regarding stem, between 1 and 33 were used, with an average of 15 different models per hospital.
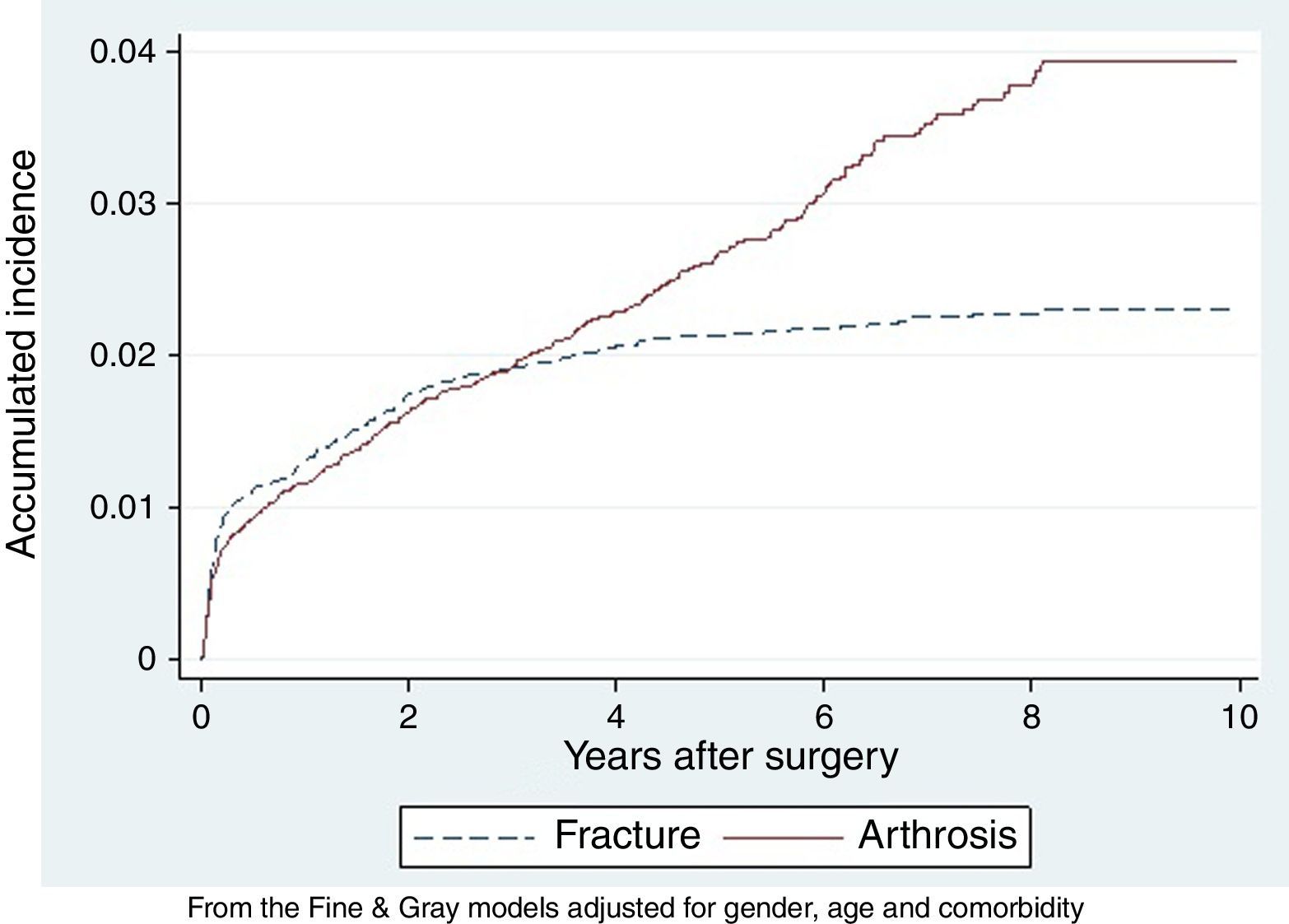
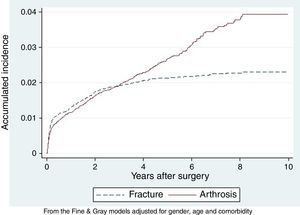
Survival analysisAccumulated revision incidenceFig. 4 shows the accumulated incidence of revision for hip replacements. A different evolutional pattern was observed depending on the causes of intervention: the accumulated incidence of replacement revision caused by arthrosis was 1.2% the first year, rising to 3.9% the tenth year and for fractures 1.3%, rising to 2.3%, respectively.
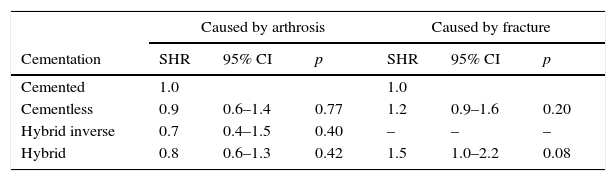
Type of fixation and revision riskWith regard to the fixation used in the hip replacements, during the 2005–2014 period no statistically significant differences were observed in revision risk between the different types of fixation, regardless of whether the cause of intervention was arthrosis or fracture (Table 3).
Relationship between the type of fixation and the risk of revision of hip replacements in the RACat (2005–2014).
| Caused by arthrosis | Caused by fracture | |||||
|---|---|---|---|---|---|---|
| Cementation | SHR | 95% CI | p | SHR | 95% CI | p |
| Cemented | 1.0 | 1.0 | ||||
| Cementless | 0.9 | 0.6–1.4 | 0.77 | 1.2 | 0.9–1.6 | 0.20 |
| Hybrid inverse | 0.7 | 0.4–1.5 | 0.40 | – | – | – |
| Hybrid | 0.8 | 0.6–1.3 | 0.42 | 1.5 | 1.0–2.2 | 0.08 |
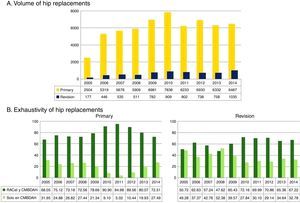
An increase in the number of primary and revision interventions was also noted in both primary and revision knee replacements, reported to the RACat over the 10 years of its existence (Fig. 5A). The largest number of primary interventions was observed in 2010, when over 7000 interventions were performed, whilst in 2011 a sudden fall was observed.
(A) Evolution of the number of primary and revision knee replacements. (B) Evolution of data exhaustivity in primary and revision knee replacements in the RACat (2005–2014). CMBDAH: conjunto mínimo básico de datos al alta hospitalaria (minimum basic data set at hospital discharge) RACat: Registro de Artroplastias de Cataluña (Catalan Arthroplasty Register).
With regards to exhaustivity (Fig. 5B), this increased progressively from the beginning of the register up until 2012. From that year onwards a gradual drop in exhaustivity was observed. In 2014 exhaustivity in primary joint replacements was 72.5% and 67.2% in revision arthroplasties.
Descriptive analysisPatients and the healthcare processAs observed in Table 1 more replacements were performed on women than on men (71.2%). In primary knee replacements, arthrosis was the main cause (98.1% of cases), whilst the most common cause of revision were mechanical complications of the orthopaedic device (54.6%). Regarding comorbidities, over half of the patients presented with one or more. Lastly, in primary knee replacements there was a 7.5% admission of patients to healthcare or residential centre, whilst for revision replacements this percentage was 8.2%.
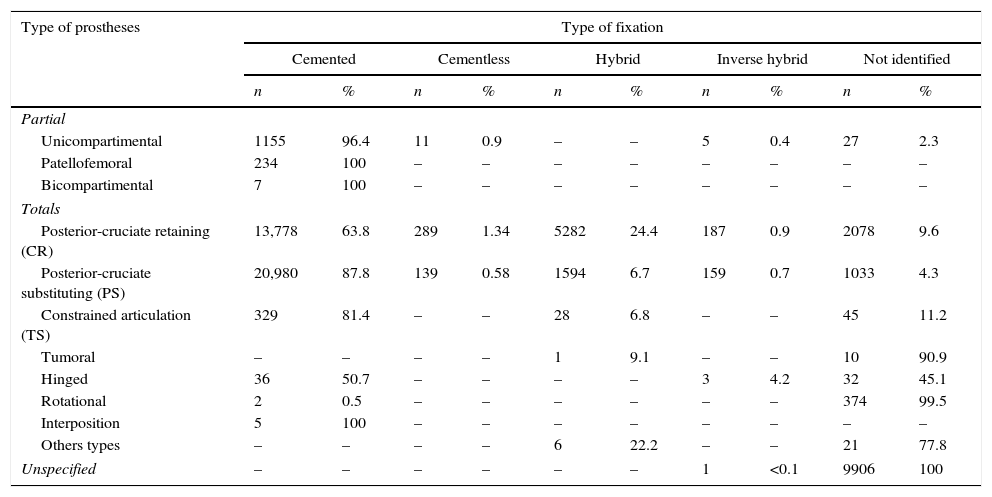
Types of arthroplasty and fixation techniqueThe most frequently used type of joint replacement in partial arthroplasties (Table 4) was unicompartimental, whilst in total arthroplasties the most used types of joint replacements were CR and PS. It was also observed that the most well used fixation technique in both unicompartimental, CR and PS joint replacements was cemented.
Frequency of the type of prosthesis and fixation technique in the knee replacements included in the RACat (2005–2014).
| Type of prostheses | Type of fixation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cemented | Cementless | Hybrid | Inverse hybrid | Not identified | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| Partial | ||||||||||
| Unicompartimental | 1155 | 96.4 | 11 | 0.9 | – | – | 5 | 0.4 | 27 | 2.3 |
| Patellofemoral | 234 | 100 | – | – | – | – | – | – | – | – |
| Bicompartimental | 7 | 100 | – | – | – | – | – | – | – | – |
| Totals | ||||||||||
| Posterior-cruciate retaining (CR) | 13,778 | 63.8 | 289 | 1.34 | 5282 | 24.4 | 187 | 0.9 | 2078 | 9.6 |
| Posterior-cruciate substituting (PS) | 20,980 | 87.8 | 139 | 0.58 | 1594 | 6.7 | 159 | 0.7 | 1033 | 4.3 |
| Constrained articulation (TS) | 329 | 81.4 | – | – | 28 | 6.8 | – | – | 45 | 11.2 |
| Tumoral | – | – | – | – | 1 | 9.1 | – | – | 10 | 90.9 |
| Hinged | 36 | 50.7 | – | – | – | – | 3 | 4.2 | 32 | 45.1 |
| Rotational | 2 | 0.5 | – | – | – | – | – | – | 374 | 99.5 |
| Interposition | 5 | 100 | – | – | – | – | – | – | – | – |
| Others types | – | – | – | – | 6 | 22.2 | – | – | 21 | 77.8 |
| Unspecified | – | – | – | – | – | – | 1 | <0.1 | 9906 | 100 |
%: Percentage compared with the total; cemented; cemented stem and socket component; hybrids, cemented stem and cementless socket; inverse hybrids: cementless stem and cemented socket; n: total number; cementless: no cemented component.
As shown in Fig. 3B, in primary knee replacements there was a tendency towards a greater number of models the greater the volume of replacements performed. The number of models used by the different hospitals ranged between 1 and 38, with a mean of 12.
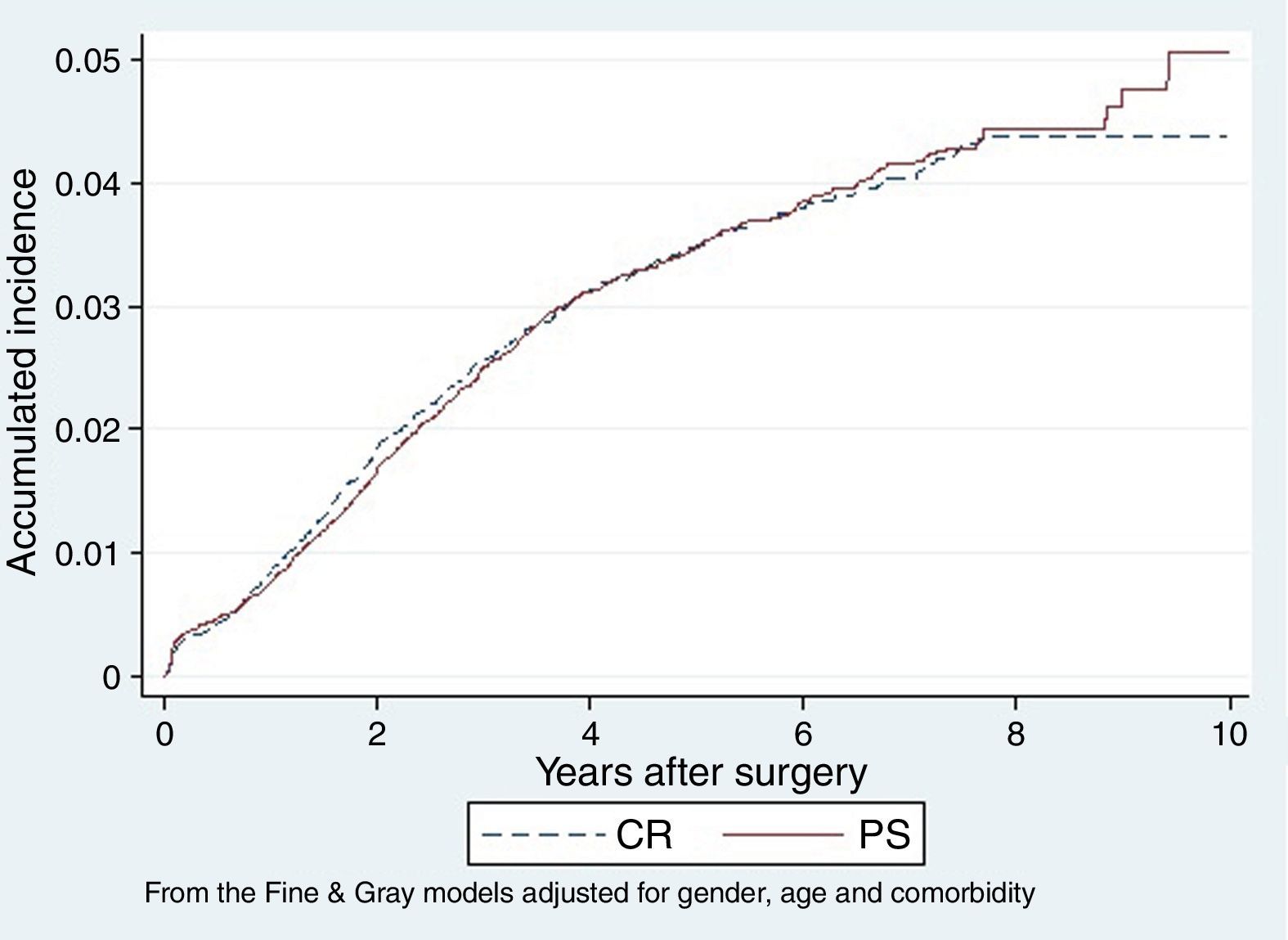
Survival analysisAccumulated revision incidenceThe pattern of accumulated incidence in knee arthroplasty revision (Fig. 6) is similar among CR and PS types. Accumulated incidence of revision for CR prostheses was 0.8% the first year, rising to 4.4% the tenth year, whilst among the PS it was 0.7% the first year and rose to 5.1% during the tenth year.
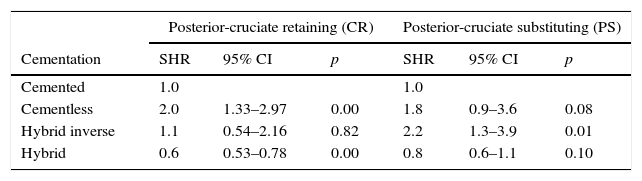
Type of fixation and revision riskDuring the study period (Table 5), among the CR type a higher risk of revision was observed among the cementless replacements (SHR: 2.0; 95% CI: 1.3–3.0) than among the cemented ones, plus a lower risk among the prostheses where the fixation technique was hybrid (tibia, not femoral cementation) compared with the cemented ones (SHR: 0.6; 95% CI: 0.5–0.8). For its part, among the PS type a higher risk of revision was observed in those where fixation was inverse hybrid (femoral, not tibial cementation) than those that were cemented (SHR: 2.2; 95% CI: 1.3–3.9), with no differences being found between cemented, cementless and hybrids.
Relationship between type of fixation and risk of revision in knee replacements in the RACat (2005–2014).
| Posterior-cruciate retaining (CR) | Posterior-cruciate substituting (PS) | |||||
|---|---|---|---|---|---|---|
| Cementation | SHR | 95% CI | p | SHR | 95% CI | p |
| Cemented | 1.0 | 1.0 | ||||
| Cementless | 2.0 | 1.33–2.97 | 0.00 | 1.8 | 0.9–3.6 | 0.08 |
| Hybrid inverse | 1.1 | 0.54–2.16 | 0.82 | 2.2 | 1.3–3.9 | 0.01 |
| Hybrid | 0.6 | 0.53–0.78 | 0.00 | 0.8 | 0.6–1.1 | 0.10 |
This study shows that, according to RACat, accumulated revision incidence 10 years after primary hip replacement (caused by arthrosis or fracture) and after primary knee replacement (CR or PS types) is, in general, similar to that observed in other registrers.6,8 Moreover, it has been shown that both data quality and the number of joint replacements has progressively increased, as occurred in other countries,15 with a large variability being observed in the number of prostheses models used by each hospital participating in the register.
Data quality: volume and exhaustivityAfter a progressive increase in the number of hip and knee episodes from 2005, a drop in the volume of interventions in both joints was observed in 2011. This drop was linked to the hospital healthcare restructuring which took place that year, since after 2012 once again there was a gradual increase in the volume of interventions. However, the increase in the number of joint replacements during the last period is not reflected in the exhaustivity of data sent to RACat, since at the end of 2013 the hospitals were obliged to temporarily stop the notification of data to be able to adapt their IT systems to the technical requirements of the CatSalut IT application, which included a new process of communication in Web Services. For this reason the exhaustivity values from the RACat dropped during the last 2 years. It is probable that in upcoming years they will improve due to the satisfactory settlement of this situation.
Description of the patients, healthcare process and prosthesesAs previously stated,5 the results of this study show that more knee and hip replacements were performed in women, with arthrosis and related processes (code 715 of the International codification of diseases [CIE-9]) being the major causes of primary joint replacement surgery.9 Furthermore, mechanical complications of the orthopaedic device were the main reason for revision arthroplasties. This event had already been previously observed in other European registers, where aseptic loosening was the most frequent cause.4,16 In the RACat register aseptic loosening was analysed together with other diagnoses, such as luxation or wear and tear of the contact surface, under the concept of mechanical complications, due to the defects found in the CMBDAH coding for causes of intervention.
Results also showed that the majority of patients who underwent surgery presented with some type of comorbidity, a fact which could be related to both the increase in life expectancy and the improvement of surgical techniques. These improvements have made it possible to operate on people of very advanced ages, who usually present with a larger number of comorbidities.11
With regard to hospital discharges, most patients went home and therefore, despite this being apparently better for recovery, patient satisfaction and healthcare costs, there is no clear evidence on the impact the discharge had on the recovery process.17 For this reason, it could be interesting for further studies to contemplate possible readmittance of patients depending on the type of discharge, to obtain greater proof of the healthcare quality of this practice in surgical procedures and more specifically in joint replacements.
With regard to the number of prosthesis models used, a large variability was found depending on the hospital. Several studies3,18 indicate that using a high number of models could constitute a revision risk factor. We determined from the results of the Swedish register that the number of available models had been limited, in expectation of reducing the risk of revision. Should this measure be confirmed, it could be of interest to consider in Catalonia, given the high variability observed between hospitals.
SurvivalConsidering the protocols prepared by Ranstam et al.19,20 for joint replacement register data analysis, survival of the prosthesis was used as the main criteria for joint replacement effectivity.3,4 Competitive risk models were used for the survival models instead of the traditional methods of Kaplan–Meier and Cox.9 This decision was taken based on the proposal in different studies in which it was shown that, in the presence of competitive risk, as is our case, the Kaplan–Meier and Cox models would overestimate the accumulated incidence.13,19–21 Moreover, the existing comorbidities, as previously proposed, were included as adjustment variables in the analysis,22 since they could constitute a source of bias when data were analysed.
Accumulated revision incidence in hip replacementsWe observed that after 10 years the accumulated incidence of revision was higher in those prostheses caused by arthrosis (3.9%) than those caused by fractures (2.3%), and that there were also differences in the pattern of development.23 This could be explained by age differences of the patients who underwent surgery due to arthrosis and fracture, since generally the patients operated on for fractures were of a more advanced age and therefore usually presented a lower risk of revision, as previously stated.5,8
Accumulated revision incidence in knee replacementsNo differences were observed for these prostheses regarding accumulated revision incidence between CR and PS types. The risk evolution pattern is similar in both types, at least up until the seventh year, after which the number of revisions is very low. These results are in contrast to those observed in previous studies, and also in other registers such as that of England and Wales or Sweden in which the survival of CR is generally higher than that of PS.8,24 Notwithstanding, in order to explain these differences, it could be a good idea to conduct further studies in which other factors were taken into account, such as underlining the cause of revision or the level of involvement of the posterior-cruciate ligament, among others.
Type of fixation and revision riskWith regard to the types of prostheses and fixation used, the results from this study are similar to those previously obtained with the RACat data with a shorter follow-up period5,9 and those reported by other joint replacement registers.6,7,25 They confirm greater revision risks in cementless and inverse hybrid knee prostheses than in cemented prostheses. However, a lower revision risk was observed between the hybrid knee prostheses than between the cemented ones, a fact that contrasts with most registers and which could be explained by the possible differences in analysis methodology used or in the study sample characteristics.
LimitationsWith regards to the limitations of this study, we would note one limitation which is inherent to all joint replacement registers and that is the observational, non-experimental nature of the information. However, the registers are a useful tool of information and guidance in clinical practice. They have a high ecological validity since in general their data involve populations, not samples, and this means possible selection biases in participant recruitment may be avoided.
Another limitation is the high number of cases where type of fixation was unspecified, especially during the first few years of recording. The lack of homogeneity and specificity in coding reasons for revision could also be an important factor in the loss of cases reported to the RACat. During those years, priority focused on the implementation and start-up of the register, without so much emphasis being placed on data quality. It is therefore to be expected that in upcoming years the percentage of non-identified cases in the RACat will gradually decrease, as has been occurring. With regards to limitations related to the study sample survival, it was observed that from the seventh year onwards there were few cases of follow-up, and the results obtained must therefore be interpreted with precaution from this point.
Despite the before-mentioned limitations, and the difficult and high cost of implementing and maintaining a register of these characteristics,8 we can confirm that, after 10 years in existence, the RACat has become a highly powerful tool for mid and long term affectivity analysis of hip and knee replacements, for the study of clinical practice variability and post-market monitoring.
ConclusionsFollowing its 10-year existence, the increase and improvement in data quality of the RACat has been confirmed. Having analysed the data, we may state that primary hip and knee replacements in Catalonia were mainly performed on women and that the main cause was arthrosis. The prostheses survival observed for the different types of joint replacements is in keeping with international standards and may be considered a benchmark when evaluating both intervention and healthcare quality in the different centres. For all of these reasons, the RACat has become a useful and necessary informative tool outlining areas of improvement in the healthcare process.
Level of evidenceLevel of evidence I.
Ethical responsibilitiesProtection of people and animalsThe authors declare that for this research no experiments on human beings or animals have been conducted.
Confidentiality of dataThe authors declare they have adhered to the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors of the article have no conflict of interests to declare in the preparation of this document, nor does any personal or financial relationship exist which could influence the methodology of the study or the analysis of study findings.
Please cite this article as: Arias-de la Torre J, Capdevila A, Martínez O, Domingo L, Marinelli M, Robles N, et al. Una década del Registro de Artroplastias de Cataluña (RACat): exhaustividad, variabilidad y supervivencia de las prótesis entre 2005 y 2014. Rev Esp Cir Ortop Traumatol. 2017;61:70–81.