Establish the long-term (10 years) predictive value of Modic changes in the course of lumbar pain and the need for surgical treatment.
Material and methodObservational longitudinal prospective cohort study. Comparison of progression at 10 years of 2 groups of patients with chronic lumbar pain: group A with Modic changes in MRI and group B with no Modic changes. Exclusion criteria: neoplasia, inflammatory or infectious diseases, or previous surgery. Assessment was done with the aid of the VAS for low lumbar and radicular pain and the Oswestry Disability Questionnaire. The need for surgical or medical treatment and occupational disability during the study period was analysed. For the statistical analyses, the Mann–Whitney U test and logistic regression were applied.
ResultsSeventy patients, 24 male and 46 female, with a mean age of 56.5 years (35 in each group) were included in the study. No statistically significant differences in the intensity of lumbar pain, degree of impairment, or need for medical or surgical treatment (p>.05) were found in patients with Modic changes types 1, 2, or 3 between the baseline assessment and 10 years after. No statistically significant differences between patients with/without changes in Modic at 10 years of follow-up (p>.05) were determined.
ConclusionsThere is no relationship between Modic changes in MRI and greater intensity of lumbar pain or need for medical or surgical treatment at 10 years of follow-up. Modic changes cannot be considered a sign of bad prognosis by themselves, or an indication for surgery.
Valor de los cambios Modic a 10 años en la evolución del dolor lumbar y requerimiento quirúrgico.
Material y métodoEstudio observacional longitudinal de cohortes prospectivo. Se compara la evolución a los 10 años de 2 grupos de pacientes con dolor lumbar crónico: el grupo A mostraba cambios Modic en la RM y el grupo B no tenía cambios Modic. Criterios de exclusión: neoplasia, enfermedad inflamatoria o infecciosa y cirugía previa. Fueron valorados mediante EVA para dolor lumbar, radicular y cuestionario de discapacidad de Oswestry. Se estudia la necesidad de tratamiento quirúrgico o médico y la obtención de una incapacidad laboral en el periodo de estudio. El análisis estadístico fue realizado mediante U de Mann-Whitney y regresión logística.
ResultadosSe incluyeron 70 pacientes, 24 varones y 46 mujeres, con una edad media de 56,5 años (35 en cada grupo). No se encontraron diferencias estadísticamente significativas en los pacientes con cambios Modic 1, 2 o 3 entre la valoración inicial y la realizada 10 años después en la intensidad del dolor lumbar, el grado de discapacidad o la necesidad de tratamiento médico o quirúrgico (p>0,05). No se observan diferencias estadísticamente significativas entre los pacientes con cambios Modic y sin ellos a 10 años de seguimiento (p>0,05).
ConclusiónLa presencia de cambios Modic en la RM no se relaciona con una mayor intensidad del dolor, de la discapacidad por dolor lumbar o la necesidad de tratamiento médico o quirúrgico a 10 años de seguimiento. Los cambios Modic no pueden ser considerados un signo de mal pronóstico por sí solos, ni una indicación para cirugía.
Low back pain is a symptom leading to a high number of consultations in primary care and trauma surgeries, as a medical problem of the highest order from its rate of incidence on the general population. Low back pain presents with multifactorial aetiology with disc degeneration being one of its main causes. The use of additional tests such as magnetic resonance (MRI) for the study of lumbar involvement has revealed the possible causes of pain in this region. One of the findings assessed in MRI as a probable cause of low back pain are Modic changes.1 These changes are signal changes in the vertebral body which may extend up to the vertebral end plate and are differentiated into 3 types by the author depending on their appearance in sequences T1 or T2 of MRI. The prevalence of Modic type changes in the general population is around 6%, and is most commonly located at levels L4-L5, although L5-S12 is the most common level for people aged between 60 and 65.
There is controversy in the literature regarding the association between the presence of Modic changes in a person and low back pain.3,4 Several studies have demonstrated the existence of an association between the presence of Modic changes and low back pain.5 However, the studies assessed have some limitations, such as the diversity of population studied and the lack of follow-up time of these patients.
The aim of our study is to: establish the clinical value of the Modic type signal changes in the MRI and its association as the cause of low back pain, with a follow-up of 10 years.
Material and methodsA longitudinal analytical study of prospective cohorts was designed.
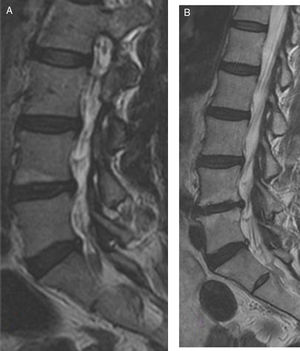
In March 2007 90 patients who had suffered from low back pain of over 6-month duration and for whom an MRI had been requested, were assessed. The intensity of the low back pain and leg pain was assessed using the visual analogue scale (VAS) and the Oswestry disability questionnaire validated into Spanish. Following completion of these data and physical examination, medical treatment was administered based on analgesics and anti-inflammatory drugs aimed at relieving their low back pain symptoms. Furthermore, they were advised to lose weight and to exercise to increase abdominal and spinal musculature. Since the patients did not present with improvement in their symptoms of low back pain after 6 months of applied treatment, a lumbar MRI was performed with protocolised examination using sagittal, coronal and axial slices, with enhanced sequences in T1 and T2 Fig. 1A), which was performed with a mean wait of 3 months since request.
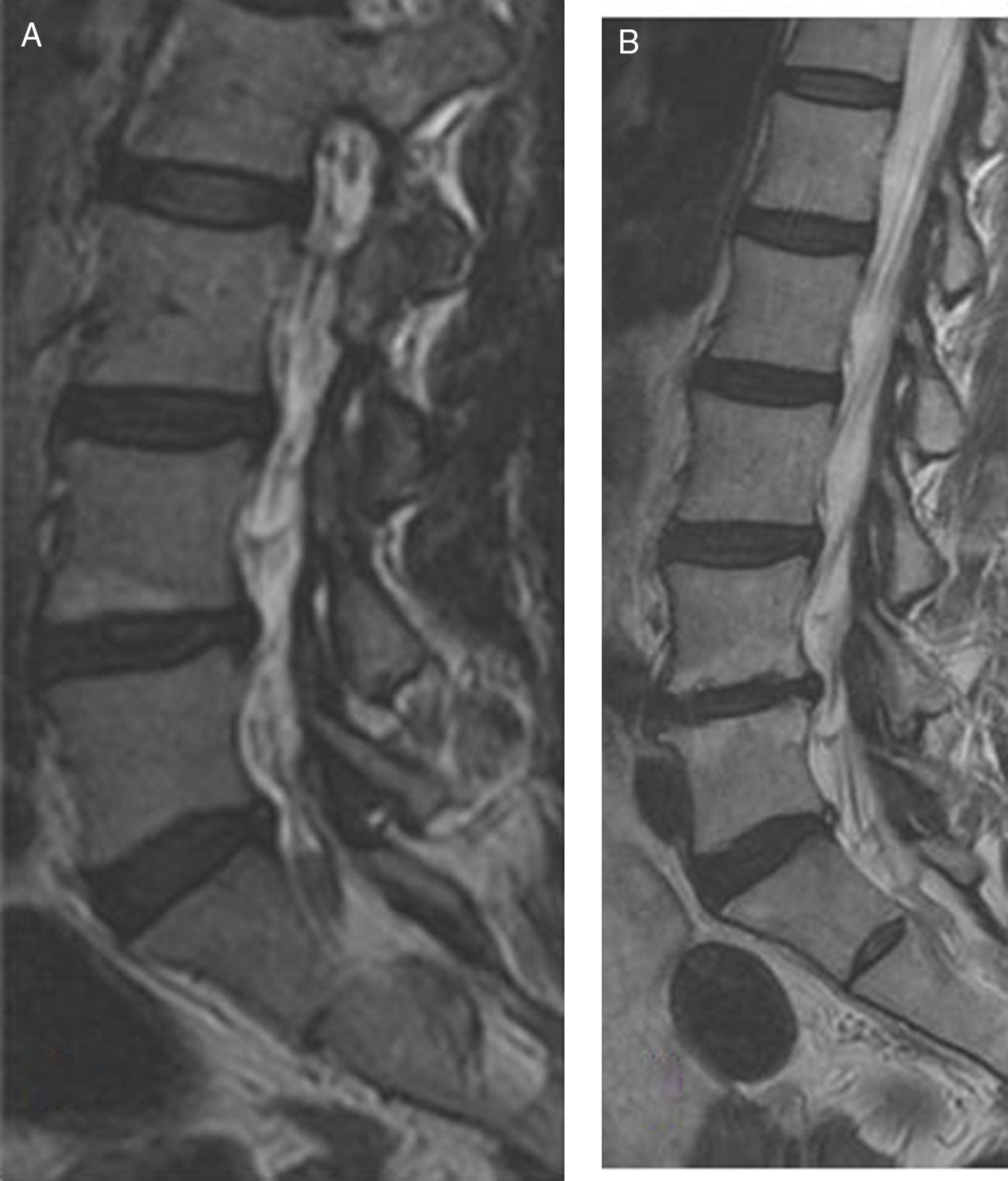
A) enhanced sagittal image in T2 of lumbar MRI of a woman aged 45 where Modic type 1 change is found in the vertebral end plate below vertebra L4. B) Image of enhanced sagittal slice in T2 of lumbar MRI of the same patient after 10 years where we observe Modic type 1 change in vertebral end plate below vertebra L4 and in vertebral endplate above L5. The patient did not require surgical treatment nor occupational disability.
For analysis of the images and their classification into presence or absence of Modic type signal changes a single-blind technique was used. The images were analysed by an orthopaedic surgeon expert in spinal surgery and by a neuroradiologist. The correlation between the findings by one or the other was calculated by the kappa interobserver reproducibility coefficient. The finding was classified as presence or absence of Modic signal changes. The patients with a presence of Modic type signal changes were divided into types 1, 2, and 3.
The clinical correlation with the findings of the MRI were calculated using the Kruskal–Wallis test. Values where p<.05 were considered statistically significant.
In January 2017 the patients who had received a lumbar MRI 10 years previously and who presented with low back pain and Modic type changes and the patients affected by chronic low back pain without Modic type sign changes in the MRI (Fig. 1B) were re-assessed.
Inclusion criteria were: (1) the performance of the lumbar MRI 10 years previously; (2) presence of low back pain of over 6 month duration when the lumbar MRI was performed and (3) assessment of the imaging studies of an orthopaedic surgeon expert in spinal surgery and/or neuroradiologist.
Exclusion criteria were as follows: (1) surgical intervention in the spine prior to the performance of the lumbar MRI intervention; (2) the presence of primary neoplasic or metastatic diseases, and (3) infectious or inflammatory pain at the time of the study.
A sample size of 70 patients was obtained with the inclusion criteria. The 70 patients were classified into 2 groups: group A (35 patients), patients with low back pain and the presence of Modic type changes in MRI, and group B (35 patients), patients with low back pain and the absences of Modic type changes, with minimum 10-year follow-up.
The variables of interest collected for analysis were: demographics, lumbar and radicular VAS at the time of study and currently, Oswestry disability questionnaire due to low back pain validated into Spanish at the time of study and currently, the need for surgical treatment in the lumbar region, the need for medical treatment in accordance with the WHO scales and the requirement of non capacity during the study period.
The data obtained were introduced into an Excel data base (Microsoft Office for Windows Vista). Statistical analysis was performed using the IBM SPSS Statistics 22 for health sciences (SPSS Inc., Chicago, IL, USA). The following were collected as dichotomised variables: gender (1: female; 2: males), need for surgery (1: yes; 2: no) and the presence of disability at the time of study (1: yes; 2: no). The ordinal qualitative variable obtained was medical treatment according to the WHO scale. The continuous quantitative variables assessed were age and the Oswestry scale, and the discreet quantitative variable, the lumbar and radicular VAS.
Calculation of the sample size (n=70) was based on the use of the F test (ANOVA of repeated measurements) to detect an effect size (partial eta-squared value of 0.0175), with an alpha error probability of .05, to the power of .8 and a correlation between the repeated measures of .7.
For current comparison versus 10 years ago relating to low back pain, leg pain and the Oswestry disability scale we used ANOVA repeated measurements. For comparison of both groups (patients with/without Modic type changes) relating to low back pain, leg pain and the Oswestry disability scale, at present and 10 years ago we used ANOVA with age as co variable. For comparison of both groups relating to the requirement for surgical treatment, medical treatment and disability, the chi-square test was used.
ResultsDuring the study period a total of 70 patients were included (24 males and 46 females) with chronic low back pain and a follow-up period of 10 years. Those patients who did not go to an external consultation for assessment and interviews were excluded.
The mean age of the patients was 56 years (range between 43 and 67).
Modic type changes were distributed in Modic type 1 (12 patients, 17%), Modic type 2 (21 patients, 30%) and, finally, Modic type 3 (2 patients, 3%). The Kappa index reflected a moderate interobserver association (k=.50; p=.08).
The most prevalent lumbar level with Modic type changes was L5 in 48 cases (69%), followed by L4 in 22 (31%). The extension of the lesion was of supra or infradiscal location (61 patients, 87%), with a proportionately lower presentation in both locations.
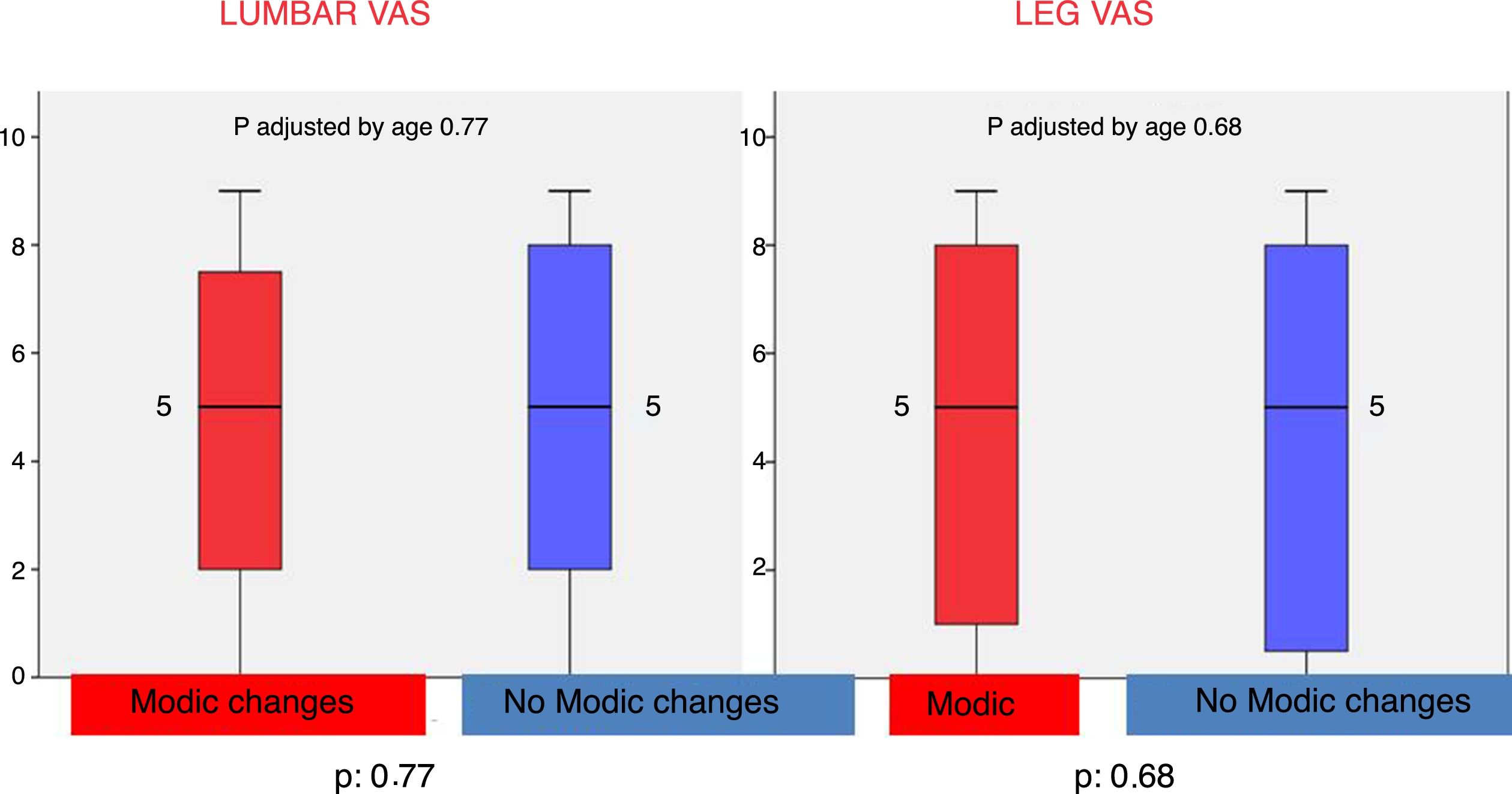
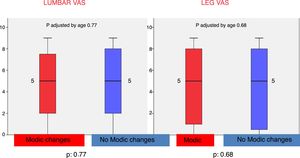
After 10 years of follow-up the mean in the lumbar VAS in patients with Modic type changes was 4.74 (SD 2.89), and 4.89 (SD 3.11) in the group without Modic type changes. The differences obtained were not statistically significant (p=.79) (Table 1).
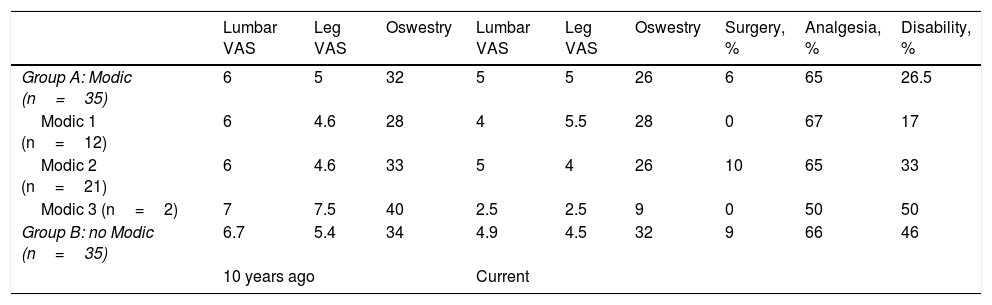
Results obtained from study parameters at the time of the study and currently for each of the groups.
| Lumbar VAS | Leg VAS | Oswestry | Lumbar VAS | Leg VAS | Oswestry | Surgery, % | Analgesia, % | Disability, % | |
|---|---|---|---|---|---|---|---|---|---|
| Group A: Modic (n=35) | 6 | 5 | 32 | 5 | 5 | 26 | 6 | 65 | 26.5 |
| Modic 1 (n=12) | 6 | 4.6 | 28 | 4 | 5.5 | 28 | 0 | 67 | 17 |
| Modic 2 (n=21) | 6 | 4.6 | 33 | 5 | 4 | 26 | 10 | 65 | 33 |
| Modic 3 (n=2) | 7 | 7.5 | 40 | 2.5 | 2.5 | 9 | 0 | 50 | 50 |
| Group B: no Modic (n=35) | 6.7 | 5.4 | 34 | 4.9 | 4.5 | 32 | 9 | 66 | 46 |
| 10 years ago | Current | ||||||||
Furthermore, after 10 years the mean in the pain VAS in the leg was 4.49 (SD 3.44) in the group with en el Group con Modic type changes y de 4.46 (DE 0.34) en el Group sin Modic type changes (Table 2), but these differences were not statistically significant (p=.75) (Fig. 2).
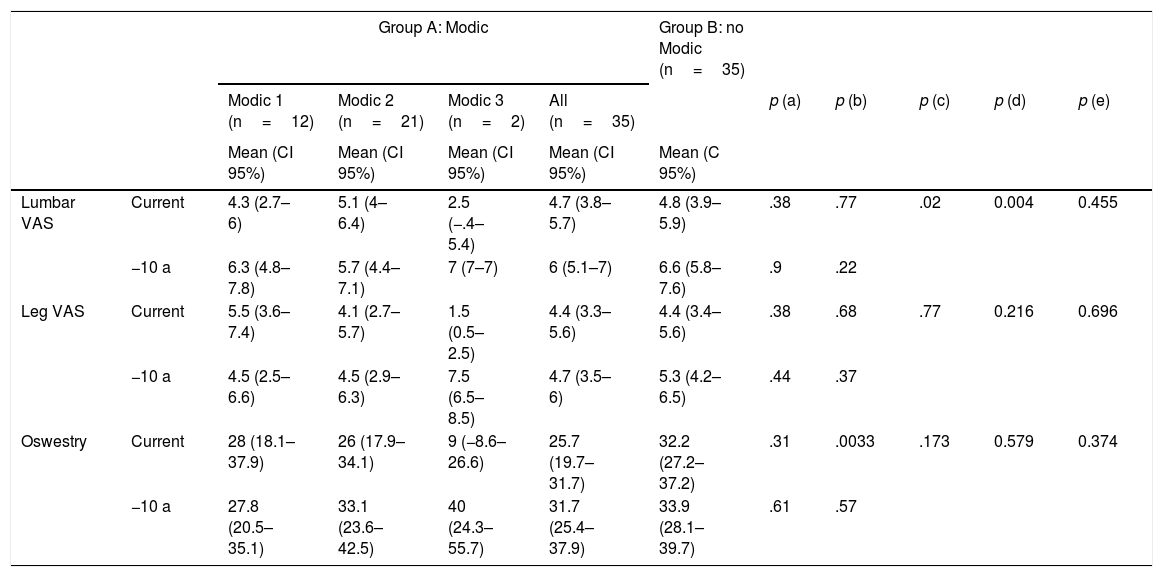
Comparison of both groups with regard to low back pain, pain in the leg and the Oswestry disability scale in patients with/without Modic type changes in lumbar magnetic resonance at 10 years of follow-up.
| Group A: Modic | Group B: no Modic (n=35) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Modic 1 (n=12) | Modic 2 (n=21) | Modic 3 (n=2) | All (n=35) | p (a) | p (b) | p (c) | p (d) | p (e) | |||
| Mean (CI 95%) | Mean (CI 95%) | Mean (CI 95%) | Mean (CI 95%) | Mean (C 95%) | |||||||
| Lumbar VAS | Current | 4.3 (2.7–6) | 5.1 (4–6.4) | 2.5 (−.4–5.4) | 4.7 (3.8–5.7) | 4.8 (3.9–5.9) | .38 | .77 | .02 | 0.004 | 0.455 |
| −10 a | 6.3 (4.8–7.8) | 5.7 (4.4–7.1) | 7 (7–7) | 6 (5.1–7) | 6.6 (5.8–7.6) | .9 | .22 | ||||
| Leg VAS | Current | 5.5 (3.6–7.4) | 4.1 (2.7–5.7) | 1.5 (0.5–2.5) | 4.4 (3.3–5.6) | 4.4 (3.4–5.6) | .38 | .68 | .77 | 0.216 | 0.696 |
| −10 a | 4.5 (2.5–6.6) | 4.5 (2.9–6.3) | 7.5 (6.5–8.5) | 4.7 (3.5–6) | 5.3 (4.2–6.5) | .44 | .37 | ||||
| Oswestry | Current | 28 (18.1–37.9) | 26 (17.9–34.1) | 9 (−8.6–26.6) | 25.7 (19.7–31.7) | 32.2 (27.2–37.2) | .31 | .0033 | .173 | 0.579 | 0.374 |
| −10 a | 27.8 (20.5–35.1) | 33.1 (23.6–42.5) | 40 (24.3–55.7) | 31.7 (25.4–37.9) | 33.9 (28.1–39.7) | .61 | .57 | ||||
95%CI: 95% confidence interval.
p (a): p value comparison Modic 1, Modic 2, Modic 3.
p (b): p value comparison Group A Modic (all) con Group B no Modic. Age adjusted.
p (c): p value comparison current versus 10 years ago, Group A all Modic.
p (d): p value comparison current versus 10 years ago, Group B non Modic.
p (e): p value interaction time×Group (current versus 10 years ago, Group B non Modic versus Group A), age adjusted.
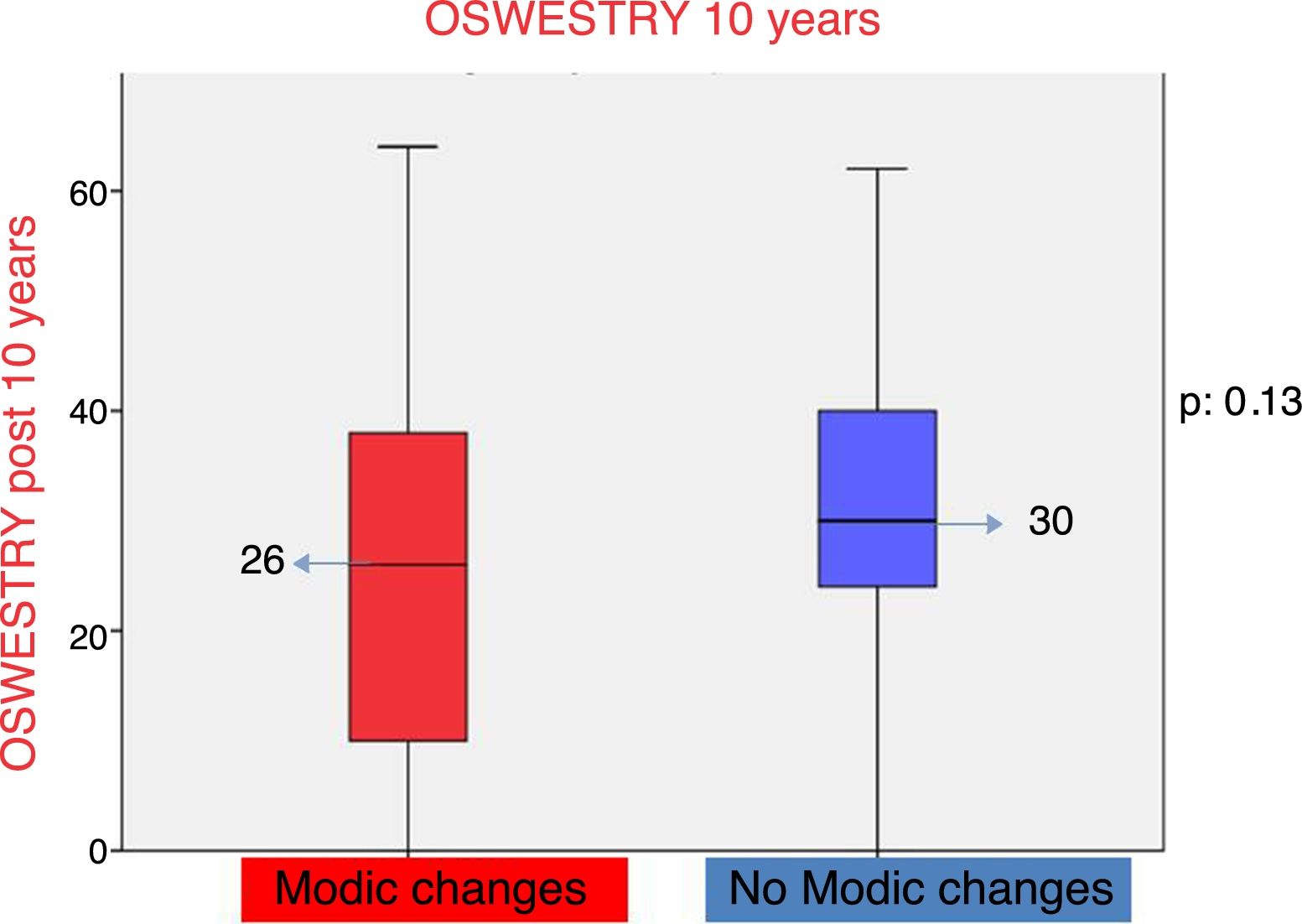
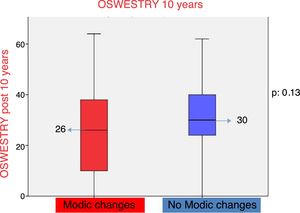
The Oswestry disability questionnaire reflected that patients with low back pain and Modic type changes presented with a score of 26 points and patients with low back pain and the absence of Modic type changes (Table 2) with 32 points. On comparing both groups the differences observed were not statistically significant (p=.13) (Fig. 3).
On comparing the patients affected by Modic changes (Modic type 1 changes compared with Modic types 2 and 3) with a follow-up of 10 years, no statistically significant differences were made in relation to the lumbar VAS (p=.38), and VAS in the leg (p=0.38) and the Oswestry disability questionnaire (p=.31).
The patients affected by Modic type changes did not require surgery during the study period in 94% of cases, but it was required in 6%. The cause of surgical treatment in 2 patients was secondary to non controllable medical and rehabilitating treatment of low back pain, and was performed with posterolateral lumbar arthrodesis of the affected levels. With a follow-up of 5 years after lumbar arthrodesis, the patients had substantially improved in symptoms. The patients with an absence of Modic type changes did not require surgical treatment in 91% of cases. Of the remaining 9% of patients without Modic type changes (3 patients), required surgical treatment during the period study secondary to an incapacitating low back pain 2 patients, with posterolateral arthrodesis being necessary in both. One patient presented with a hernia of disc L5-S1 with radicular pain of over 3 month duration, requiring a simple discectomy. The patients who underwent surgery clinically improved after surgery after a follow-up of 5 years. Comparative analysis showed no statistically significant differences when surgical treatment was required between those patients with a presence of Modic type changes compared to those that did not present with them (p>.05) (Table 3).
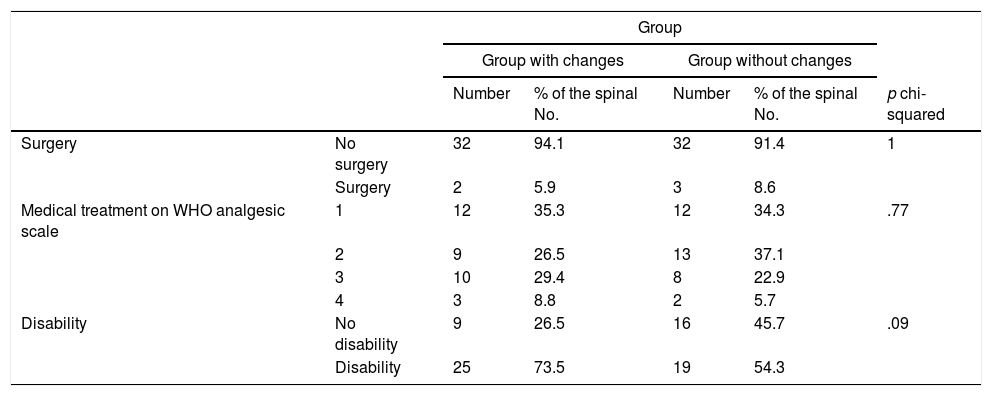
Comparison of both groups with regards to the requirement for surgical treatment, medical treatment and disability in patients with/without Modic type changes in lumbar magnetic resonance imaging at 10 years of follow-up.
| Group | ||||||
|---|---|---|---|---|---|---|
| Group with changes | Group without changes | |||||
| Number | % of the spinal No. | Number | % of the spinal No. | p chi-squared | ||
| Surgery | No surgery | 32 | 94.1 | 32 | 91.4 | 1 |
| Surgery | 2 | 5.9 | 3 | 8.6 | ||
| Medical treatment on WHO analgesic scale | 1 | 12 | 35.3 | 12 | 34.3 | .77 |
| 2 | 9 | 26.5 | 13 | 37.1 | ||
| 3 | 10 | 29.4 | 8 | 22.9 | ||
| 4 | 3 | 8.8 | 2 | 5.7 | ||
| Disability | No disability | 9 | 26.5 | 16 | 45.7 | .09 |
| Disability | 25 | 73.5 | 19 | 54.3 | ||
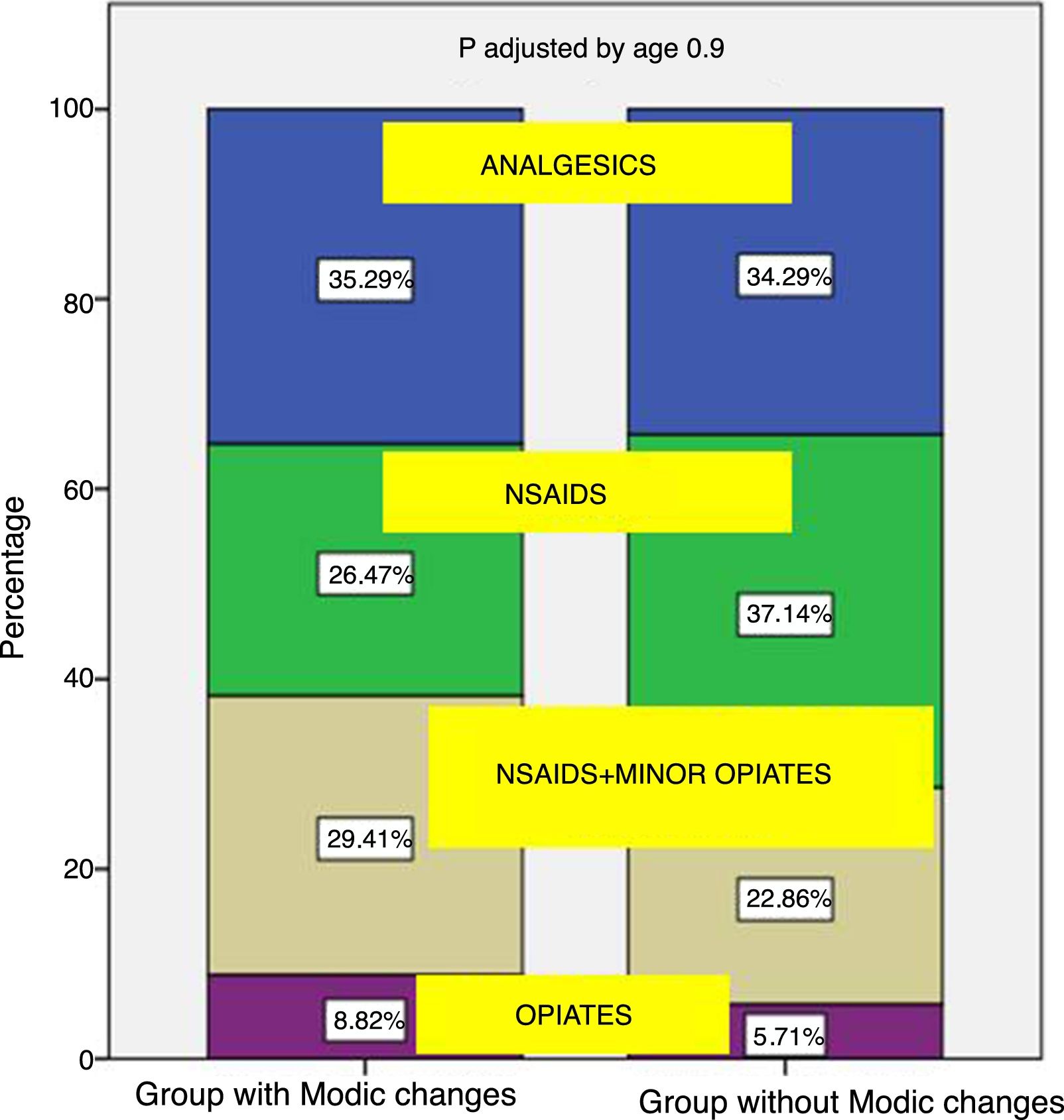
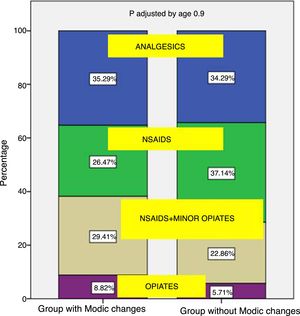
With regard to medical treatment, between the patients with Modic type changes in MRI, 61% used NSAIDS as treatment and non opiate analgesics, with more powerful opiates being required as treatment for their lumbago in 9% of cases. The patients without Modic type changes required NSAIDS and non opiate analgesics in 71% of cases, with the need for more powerful opiates for treatment in 6% of cases. No statistically significant differences were found between the need for further medical treatment in patients with presence of Modic type changes compared with patients who did not present with them (p=.77) (Fig. 4).
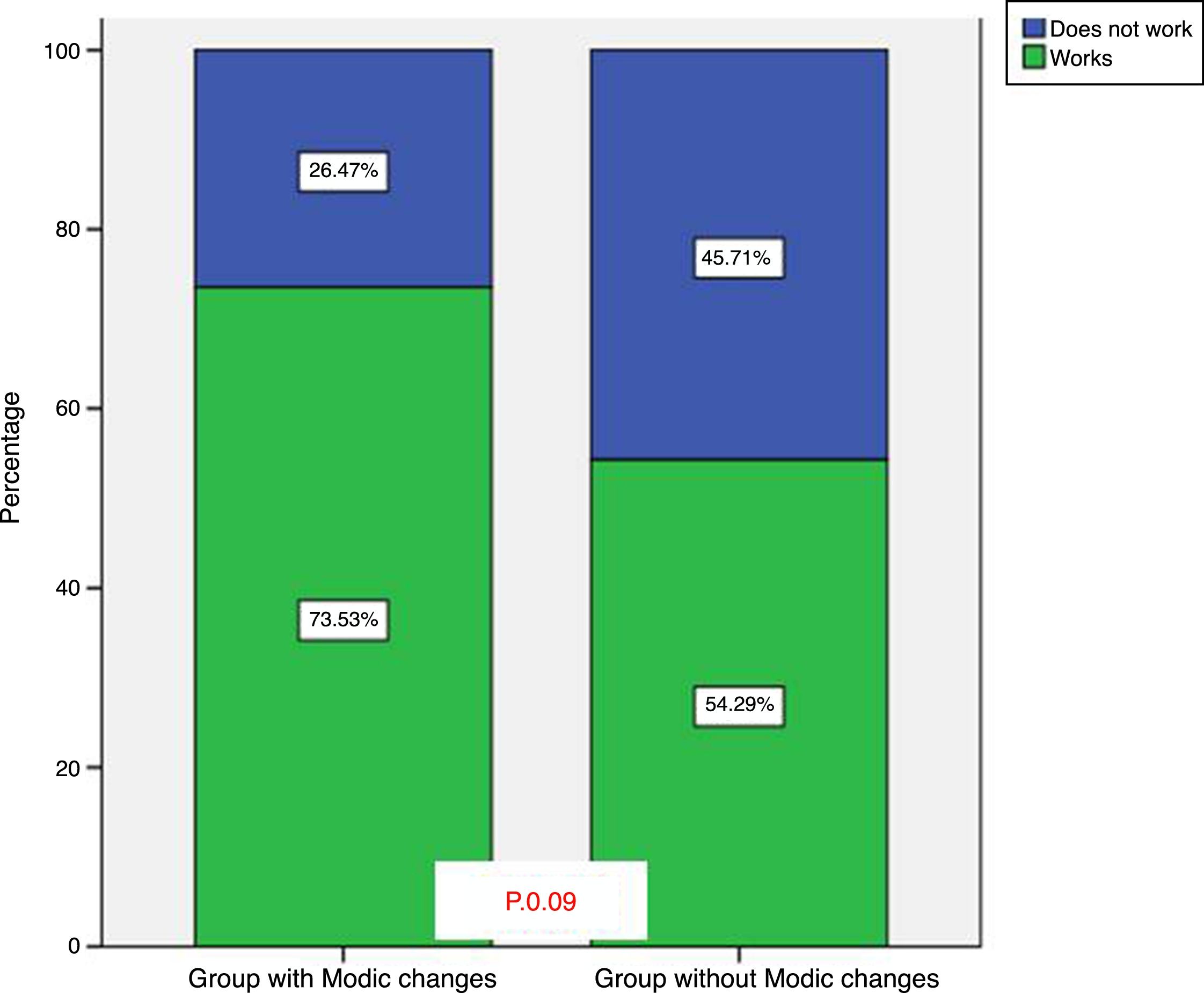
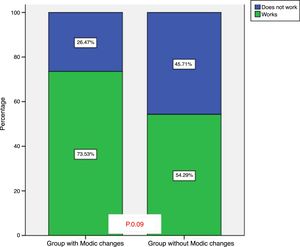
When comparing the requirement for occupational disability during the study period between those with Modic type changes and those who did not present with them, no statistically significant differences were observed either (p=.09). Disability after 10 years of follow-up was found in 26% of patients with Modic type changes and in 46% of patients without Modic type signal changes (Fig. 5).
DiscussionIn this study results showed that the presence of Modic type changes in patients with low back pain do not implicitly lead to a poorer follow-up regarding pain or the need for surgical intervention. Furthermore, the results obtained reflect that the patients with the presence of Modic changes do not require more medication for the relief of symptoms nor present higher levels of sick leave after 10 years compared to patients who do not present with these changes in lumbar MRI. The association between Modic changes and low back pain symptoms have been studied in recent years in the reviewed literature. The results assessed were contradictory in the studies made with a series of patients. There are studies which associate low back pain with the presence of Modic changes.5–12 Kjaer et al. Published a study in which 412 patients were assessed who were classified according to MRI findings in keeping with the presence of disc degeneration and Modic changes, only disc degeneration or neither of the 2 changes. This concluded that the presence of Modic changes associated with disc degeneration could be considered a different clinical entity from isolated disc degeneration, given that these patients presented with a different clinical profile.5 Toyone et al. confirmed there was an association between type 1 changes and low back pain. 73% of patients with Modic type 1 changes presented with significant low back pain. In contrast 11% of patients with Modic type 2 changes presented with significant pain.6 Braithwaite et al. Reflected a high specificity and positive predictive value for all types of Modic changes as an indicator of disc change in the discography.7 However, other recent studies showed no such association.8–10 Sandhu et al. did not find any association between the changes in the vertebral bodies and the provocation of the pain in the discography.8 Secher and Karppinen, in a systematic review of the literature, highlighted a prevalence of Modic type changes in 6% of the population without signs of low back pain and that the presence of this entity in the MRI was associated with patients without pain in the low back region.9
Similarly to the results obtained in our study, Corniola et al.10 found that with a sample size of 284 patients, those with Modic type changes in the MRI of the spine did not show statistically significant differences related to low back pain assessed with VAS or quantified disability with the Oswestry questionnaire, compared with those patients without presence of Modic type changes in the spine (p=.98).
The most frequent subtype assessed in this study is type 2. These results are comparable to others assessed in the literature, such as that of Wang et al.,11 in which type 2 was the most common subtype (29.2%) and type 1 represented 6.4%.
In our series, the patients with Modic type changes did not require surgical treatment in 94% of cases, with this data being similar to those of our area of influence.12 Despite the fact 9% of patients without the presence of Modic changes required surgical treatment (3 patients) compared with 6% of the patients with Modic type changes in the MRI (2 patients), the differences assessed were not statistically significant. For this reason, although the results may reflect that more patients in the group without Modic changes undergo surgery, these differences are not significant. Several authors confirm, similarly to our study group, that the referral for surgery on patients with chronic low back pain and the presence of Modic type changes is exclusively determined by the clinical signs and not by the presence of these findings in the MRI.12 Sorlie et al. published that the patients who underwent lumbar disectomy presented with the same follow-up regarding pain as other patients with others types of Modic changes.13
The most highly accepted causal theories in the literature are biomechanical theories, where the disc damage increases the load force to the vertebral plates which induce its damage, and are the cause of the appearance of Modic changes. At present theories regarding an origin in infection are gaining ground, which involve Propionibacterium acnes as the precursor of the origin of the Modic changes in the lumbar region.14 These studies affirm that the Modic changes may be secondary to bacterial infections from low grade germs which originate in the vertebrae adjacent to the infected disc. However, these findings were not corroborated by other authors.15
One limitation of our study that needs highlighting is that it has not been possible to conduct a new study with lumbar MRI in all patients aimed at assessing the Modic type changes after 10 years. For this reason it has not been possible to assess the evolution of Modic changes in the MRI in the study period in patients who already presented with them at the beginning of the study compared with those who did not. Furthermore, we lost 20 patients out of the existing 90 at the beginning of the study. However, we consider that this loss of patients does not affect the external validity of this study, given that those who were lost were similar to those included in the study.
We believe that the limitations do not undermine the study conclusions, which, on the other hand, have the strength of a follow-up greater than 10 years and that the study was executed on a group of consecutive patients in a highly homogeneous clinical environment, without the presence of selection bias. The diagnostic and therapeutic process was carried out by the same medical team. Our series is higher in size to the majority of those published previously and the data collected prospectively. For this reason the results of this study may be extrapolated to the general population.
To conclude, and based on our results, we cannot affirm that the presence of Modic changes in the lumbar MRI are related to greater intensity of pain and disability in the lumbar region with respect to those patients in whom it did not appear. The Modic changes cannot alone be considered a bad prognosis. However, further prospective studies are required to seek probable aetiologies for the appearance of Modic type changes in MRI.
Level of evidenceLevel of evidence ii.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments have been conducted on humans or animals for this research study.
Confidentiality of dataThe authors declare that they have adhered to the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare
Please cite this article as: Romero-Muñoz LM, Barriga-Martín A, Segura-Fragoso A, Martín-González C. ¿Supone la presencia de cambios Modic en pacientes con dolor lumbar crónico una peor evolución clínica y una mayor posibilidad de precisar cirugía? Evolución a 10 años. Rev Esp Cir Ortop Traumatol. 2018;62:274–281.