Patellofemoral arthroplasty is an infrequently used surgical technique because of its controversial results. In an attempt to improve the results, a design with a mobile-bearing polyethylene patellar component has been developed. We describe a clinical case with an unusual complication: the dislocation of polyethylene from the metal backing; and accordingly, we carried out a literature review of this complication.
La artroplastia femoro-patelar continúa siendo una técnica quirúrgica poco utilizada por los discutidos resultados obtenidos. En un intento de mejorar sus resultados se introdujo el diseño con polietileno móvil. Presentamos un caso clínico con una complicación poco frecuente: la luxación del polietileno de la base metálica de la patela; y a propósito realizamos una revisión bibliográfica de esta complicación.
Isolated patellofemoral osteoarthritis remains an unsolved problem in degenerative knee pathology. It is radiographically observed in 11% of men and 24% of women over 55 years in whom a radiographic study is conducted due to a symptomatic knee.1–3 Surgical treatment is reserved for patients with functional failure and severe pain symptoms in whom conservative measures have not been successful. The choice of surgical technique is based on the symptoms, along with objective findings and other factors such as age, level of activity and occupation.4 Such procedures include cleaning arthroscopy, osteotomy, osteochondral transplants and patellectomies, all with poor results.5 Although in older patients total knee arthroplasty seems the best option, in patients under 55–60 years with normal tibiofemoral alignment, without signs of patellar subluxation and with reasonable functional expectations, patellofemoral arthroplasty may be considered as a preferable option as it is less invasive and preserves the tibiofemoral joint.
McKeever created the first design for a patellofemoral prosthesis in 1955, although it was not until the 1970s, with the introduction of the designs by Lubinus and Richard, that their regular use became widespread. In an attempt to improve results, in recent years there has been a renewed interest in patellofemoral arthroplasties which incorporated design changes and enhancements, improved instrumentation for a more accurate surgical technique and an adjustment in the indications. The latest prosthetic design to be introduced has been a patellofemoral prosthesis with mobile polyethylene.
We report a rare complication: dislocation of polyethylene in the patellar metal base. This is the first case reported in the Spanish literature and the tenth worldwide.
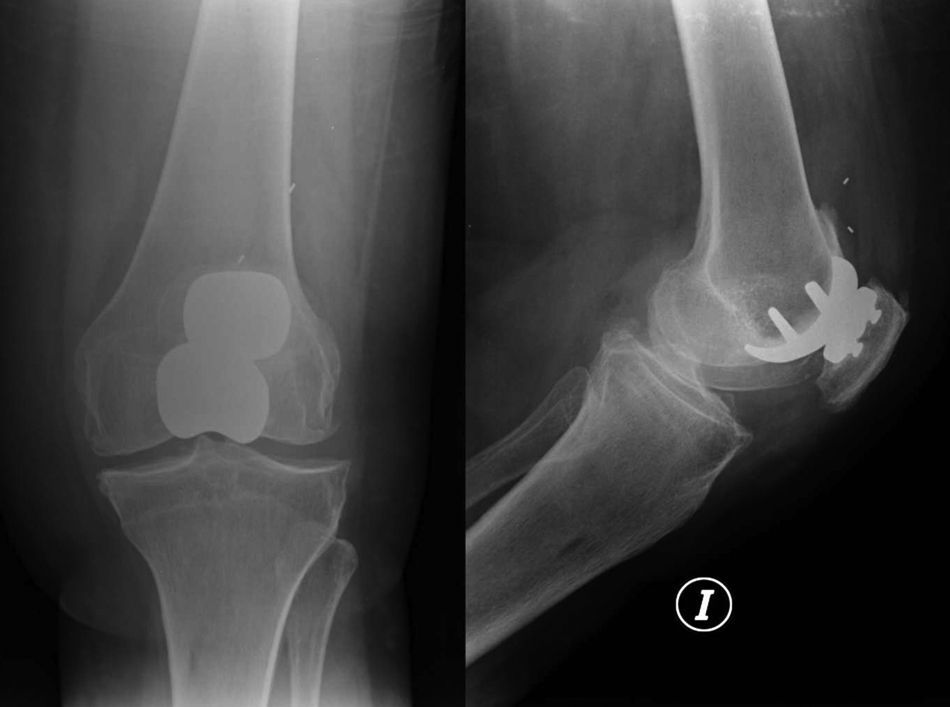
Case reportWe describe the case of a 55-year-old woman who attended our service due to persistent bilateral knee pain after undergoing partial medial patellectomy and arthroscopy on her left knee 1 year earlier. Exploration of the left knee, more symptomatic than the right, revealed patellofemoral findings and a range of movement with 10° extension. Radiographic images showed gonarthrosis, mainly of the patellofemoral compartment (Fig. 1), and a magnetic resonance study revealed a bilateral patellofemoral arthrosic chondropathy.
In February 2005, the patient underwent a patellofemoral arthroplasty with a left Low Contact Stress (LCS) patellofemoral prosthesis (DePuy, Warsaw, IN, USA) (Fig. 1). She progressed satisfactorily, reporting clinical improvement and personal satisfaction. Two years later, plain radiographs showed no change compared to the initial images and the range of motion was −5°/130°. Three years after the surgery, radiographic images remained unchanged and the range of motion was 10°/130°.
At 4 years after surgery, the patient consulted due to persistent knee pain without history of trauma and with an evolution of various months. Plain radiographs showed a separation of the polyethylene component from the patellar metal base. According to its markers, the polyethylene was located at the bottom of the external quadricipital recess (Fig. 2). We considered replacing the partial patellofemoral arthroplasty with a total knee arthroplasty. During surgery, we confirmed that the patellar polyethylene component was dislocated and free within the knee. In addition, discrete metallosis was also observed in the periprosthetic soft tissues, supposedly due to the dislocation and the duration of knee pain. Once removed, the implant showed metal–metal friction marks. Review surgery was performed using a complete LCS primary prosthesis with rotating platform (DePuy, Warsaw, IN, USA), without incident and with a good subsequent evolution. Three years after surgery, the patient remained asymptomatic, presented a good range of motion (−5°/100°) and manifested her satisfaction.
DiscussionDifferent causes of patellofemoral arthropathy require different treatments, with the most common causes being malalignment, dysplasia, instability, trauma, inflammatory arthritis, obesity and osteoarthritis. The choice of treatment is based on the symptoms, on objective findings and on other data such as age, activity and occupation.4 According to Witjes, the best candidates for patellofemoral arthroplasty are patients younger than 55–60 years with normal tibiofemoral alignment and without signs of patellar subluxation.4
A literature review resulted in the identification of the following contraindications for patellofemoral arthroplasty: first treatment choice being without having tried other conservative options, tibiofemoral joint osteoarthritis, systemic inflammatory joint disease, unevolved patellofemoral osteoarthritis, low patella, instability with patellofemoral misalignment, tibiofemoral mechanical malalignment (more than 5° varus or more than 8° valgus), active infection, clinical symptoms of complex regional pain and limitation of knee motion (−10° extension and 110° flexion).5 In any case, it should be noted that this literature review was conducted on very few studies, all with a low number of patients and limited available data. The problems leading to failure of a patellofemoral arthroplasty include progression to tibiofemoral osteoarthritis, patellar pain, subluxation due to poor balance of soft parts, poor surgical technique with malposition of the components and design problems.6
Most current patellofemoral arthroplasty designs are based on total knee arthroplasty patellofemoral designs with certain modifications such as intramedullary instrumentation, a greater range of sizes, providing compatibility of the patellar prosthesis with total review arthroplasty, a minimal incision, improved cementing techniques and better polyethylene materials, a superolateral extension of the trochlear ridge to improve patellar capture and a less constrained trochlear angle to reduce path errors of the patellar prosthesis.7
It was Merchant who, in 2001, designed a modular patellofemoral prosthesis based on the design of the LCS total knee prosthesis, with some design inspiration from Richards.8 This was a patellar implant prosthesis with mobile and congruent anatomical polyethylene seated on a thin metal base. Congruence improved any potential polyethylene wear problems, whereas mobility decreased shear forces and thus reduced loosening. This patellar component was articulated with a metallic trochlear component.9
The percentages of reviews in LCS patellofemoral arthroplasties with mobile polyethylene have been high, even leading some authors to abandon their use.9 The weakest point of the LCS patellofemoral prosthesis lies in the interface of the articulated polyethylene insert with the metallic base.10
Dislocation of the polyethylene component is a rare complication. So far, we found 9 reported cases in the literature of polyethylene dislocations in LCS patellofemoral prostheses: Witjes et al. reported 2 cases in 2009,4 Van Jonbergen et al. reported 2 cases in 2009,3 Sreekumar et al. reported 1 case in 2009,6 Arumilli et al. reported 2 cases in 1 patient (repetition) in 201010 and Charalambous et al. reported 2 cases in 2011.2
The causes of component dissociation would be multifactorial: poor surgical technique regarding the placement of implants, prosthetic design and selection of patients.
Leadbetter collects a personal communication by Fulkerson, stating that high patella leads to a risk of collision in the first degrees of flexion of the patellar component at the top ridge of the femoral prosthesis, with this posing a risk of dislocation.5 This would be a cause of residual clicking and locking sensation in the initial designs of Lubinus, which Argenson et al. attempted to compensate by inserting the femoral component slightly deeper, with the drawback of creating a femoral notch.11
Other authors have noted that dislocation occurs when the polyethylene rotates over 30°, at which point it jumps over the pin anchoring it to the metal base, which stays in place. In other words, the problem would be a wrong position of the patellar insert, leading to a rotation of the polyethylene over 30° on the base. In order to avoid this, we must be careful when orienting the patella, as this orientation takes place with the patella in an everted position, and its transverse axis is not the same when everted as after being reduced. With an everted patella, the patellar guide should be placed with about 20° inferior deflection. Thus, when its transverse axis is reduced, it will be parallel to the transverse axis of the knee.9 But even after adequately orienting the patellar metal base, patellofemoral malalignment or instability represent contraindications, as they may require a rotation of the polyethylene over 35°.4 A wrong patellar path could cause the corner of the polyethylene component to become caught in the margin or corner of the femoral trochlear component, leading to polyethylene dislocation.2
One advantage introduced by the LCS design in patellofemoral arthroplasties is that, in case conversion into total knee arthroplasty becomes necessary, it is not necessary to replace the patella. Obviously, if a dislocation of the polyethylene from the patellar base takes place, total replacement will be required in order to correct the deficiencies leading to this complication.
In the case described it seemed that a previous high patella (with an Insall–Salvati index of 1.29) was the reason that led to a high prosthetised patella with respect to the trochlear insert, eventually leading to the polyethylene becoming caught on the trochlear edge and dislocating upon flexion.
The use of patellofemoral arthroplasties remains controversial. Arumilli et al. observed high rates of review after a short series of mobile patellofemoral arthroplasties, leading them to abandon the technique.10 Charalambous et al. conducted an independent, short-term review of mobile LCS patellofemoral prostheses with disappointing results. They reported a high percentage of reviews and concluded that their use could not be recommended.2 In any case, patellofemoral prostheses do not replace patellofemoral realignment, and in the event of there existing a patellofemoral misalignment and obviously also a high patella, these should be corrected during the same surgical procedure of patellofemoral prosthesis, adapting the technique to the previous pathology.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animals. The authors declare that this investigation did not require experiments on humans or animals.Confidentiality of data. The authors declare that this study does not reflect any patient data.Right to privacy and informed consent. The authors declare that this study does not reflect any patient data.
Please cite this article as: Sangüesa Nebot MJ, et al. Luxación del polietileno en prótesis patelo-femoral con patela móvil. Caso clínico. Rev Esp Cir Ortop Traumatol. 2012;56:385–8.