The purpose of this study is to evaluate the results and complications of hip arthroplasty with conventional stem performed as a salvage procedure after the failed treatment of an intertrochanteric hip fracture.
Materials and methodsBetween 1997 and 2011, 17 patients with a mean age of 76 years were treated with hip arthroplasty for failed treatment of intertrochanteric hip fracture. In all cases a conventional stem was used. The mean follow-up was 6 years (range 1–14 years). Pain, range of motion (Merle d’Aubigné) and functional results (Barthel), as well as implant fixation (Harris and Engh), were evaluated during the follow-up.
ResultsExcept for one case of death (6%) and one case of infection (Girdlestone arthroplasty), all patients were able to walk independently at 6 months. The majority of the patients (87%) had no or mild pain. After 2 surgeries (osteosynthesis and hip arthroplasty) the mean Barthel Score had decreased from 81 to 66 points. Just one case (6%) of stem loosening has been observed.
DiscussionIn older patients, prosthetic replacement after failed proximal femoral fixation is a reliable salvage option. Most patients have good pain relief and functional improvement, although the rate of perioperative medical complications is high. Surgery is less demanding and the operating time is shorter when conventional femoral stems are used.
El objetivo de este estudio es evaluar los resultados del tratamiento del fracaso de la osteosíntesis en fracturas del fémur proximal mediante artroplastia de cadera con vástago convencional.
Material y métodosEstudio retrospectivo de 17 pacientes (edad media 76 años), en las que se implantó una prótesis de cadera tras haber fracasado la osteosíntesis de una fractura pertrocantérica, entre 1997 y 2011. En todos los casos se implantó un vástago femoral convencional. El seguimiento medio fue de 6 años (1–14 años). Se ha evaluado el dolor, la movilidad y la marcha (Merle d’Aubigné) y el resultado funcional (Barthel), así como la estabilidad radiológica del implante según los criterios de Harris y de Engh.
ResultadosExcluyendo un caso de exitus (6%) y una infección tratada mediante artroplastia de resección tipo Girdlestone, a los 6 meses de la cirugía protésica todos los pacientes habían recuperado la deambulación autónoma. El 87% presentaban dolor leve en su cadera o no tenían dolor. Tras las 2 cirugías el Barthel medio había disminuido en 15 puntos (de 81 a 66). Únicamente se ha observado un caso de aflojamiento aséptico del vástago femoral (6%).
DiscusiónLa artroplastia de cadera es un procedimiento efectivo en el rescate del fracaso de la osteosíntesis de fracturas proximales de fémur. Permite un rápido alivio del dolor y una eficaz recuperación funcional, aunque la morbimortalidad asociada es elevada. La utilización de vástagos convencionales y no vástagos largos de revisión permite simplificar la cirugía y disminuir el tiempo quirúrgico.
The incidence of proximal femur fractures among the elderly has experienced a steady increase in recent decades. The treatment of choice in most cases is surgical, via screw-plate systems and intramedullary nailing.1
The failure rate is variable according to the different published series.2 While some authors, such as Baumgaertner et al., have published success rates approaching 100%, other studies, such as that by Haidukewych et al., have reported failure rates up to 56% for certain types of fracture. The causes that have been associated with failure are varied: unfavorable fracture pattern, incorrect implementation of the synthesis system, fracture comminution, poor bone quality and infection.3,4
There are 2 main treatment options for a failure of the primary synthesis: revision of the synthesis or hip replacement, depending on the location of the fracture and the characteristics of each patient. Most surgeons5,6 prefer to carry out a revision of the synthesis, with or without an autogenous bone graft, in young patients and even some active seniors with good bone quality and preservation of the femoral head and articular surfaces. However, in elderly patients with poor bone quality and loss of healthy articular surface, the procedure of choice is to implant a hip arthroplasty.7,8
Most authors advocate the use of revision stems in order to overcome the orifices in the cortex of the femoral diaphysis created by the primary osteosynthesis. Haidukewych and Berry conducted a review of 60 patients intervened due to failure of the osteosynthesis in pertrochanteric femur fractures. They used long stems in 50% of cases.9 Thakur et al. implanted a long, uncemented, modular stem in 15 patients, with a follow-up period of 2.86 years. The mean preoperative score in the Harris scale was 35.90, which increased to 83.0110 after the intervention. Talmo and Bono used an uncemented revision prosthesis in similar patients and obtained a mean postoperative score of 86 points in the Harris scale after 30 months of follow-up.11
The aim of our study is to evaluate the results of hip arthroplasty with a conventional stem as a rescue treatment following failure of the primary osteosynthesis in fractures of the proximal femur among elderly patients. Given that this is a technically demanding procedure, with high associated morbidity and mortality, the use of conventional stems can provide satisfactory clinical and functional outcomes, simplifying the intervention and reducing surgical time in patients with low functional demands and a high rate of associated medical complications.
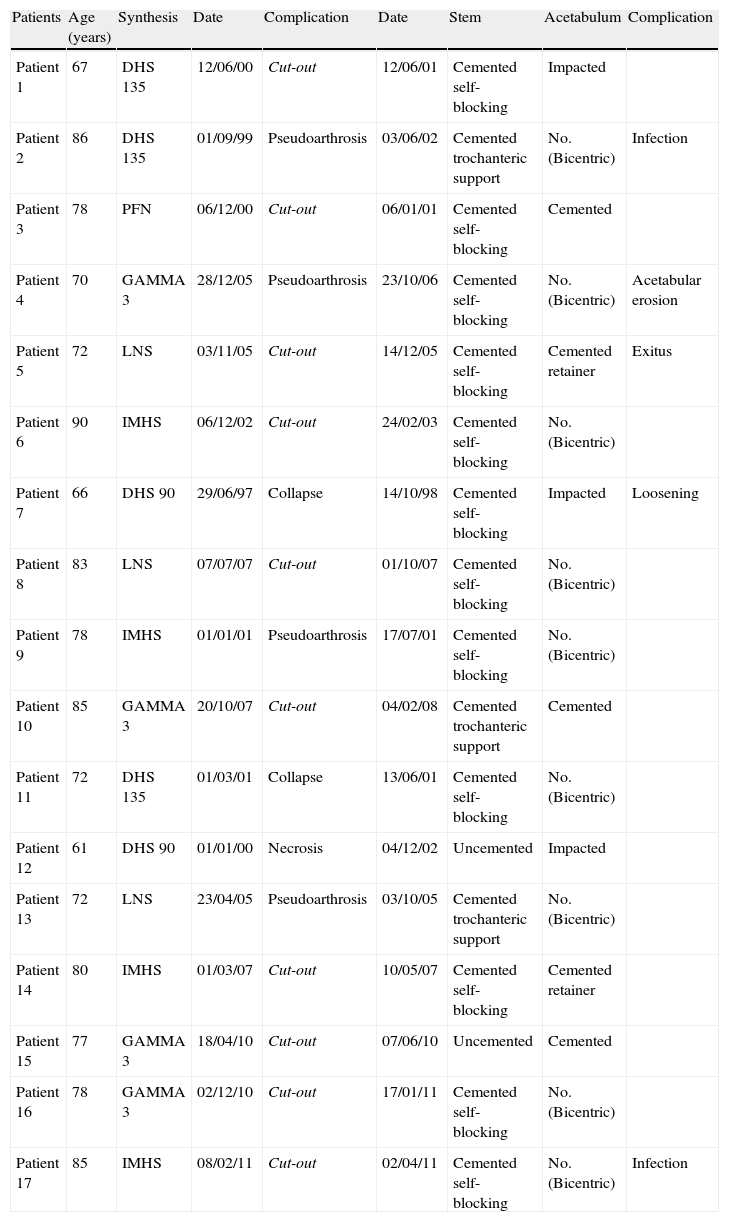
Materials and methodsThis was a retrospective study of 17 patients (17 females) with a mean age of 76 years (range: 61–90 years), who underwent surgery at our hospital between 1997 and 2011, to receive a hip implant after failure of the synthesis of a pertrochanteric femoral fracture. Such failures included cases of pseudoarthrosis (or nonunion), cut-out, osteonecrosis and fracture collapse.
Out of the total of 17 patients, 5 had been treated for their pertrochanteric fracture through a screw-sliding plate synthesis system, while in the remaining 12 cases the fracture had been synthesized by antegrade intramedullary nailing (Table 1).
Material and methods.
| Patients | Age (years) | Synthesis | Date | Complication | Date | Stem | Acetabulum | Complication |
| Patient 1 | 67 | DHS 135 | 12/06/00 | Cut-out | 12/06/01 | Cemented self-blocking | Impacted | |
| Patient 2 | 86 | DHS 135 | 01/09/99 | Pseudoarthrosis | 03/06/02 | Cemented trochanteric support | No. (Bicentric) | Infection |
| Patient 3 | 78 | PFN | 06/12/00 | Cut-out | 06/01/01 | Cemented self-blocking | Cemented | |
| Patient 4 | 70 | GAMMA 3 | 28/12/05 | Pseudoarthrosis | 23/10/06 | Cemented self-blocking | No. (Bicentric) | Acetabular erosion |
| Patient 5 | 72 | LNS | 03/11/05 | Cut-out | 14/12/05 | Cemented self-blocking | Cemented retainer | Exitus |
| Patient 6 | 90 | IMHS | 06/12/02 | Cut-out | 24/02/03 | Cemented self-blocking | No. (Bicentric) | |
| Patient 7 | 66 | DHS 90 | 29/06/97 | Collapse | 14/10/98 | Cemented self-blocking | Impacted | Loosening |
| Patient 8 | 83 | LNS | 07/07/07 | Cut-out | 01/10/07 | Cemented self-blocking | No. (Bicentric) | |
| Patient 9 | 78 | IMHS | 01/01/01 | Pseudoarthrosis | 17/07/01 | Cemented self-blocking | No. (Bicentric) | |
| Patient 10 | 85 | GAMMA 3 | 20/10/07 | Cut-out | 04/02/08 | Cemented trochanteric support | Cemented | |
| Patient 11 | 72 | DHS 135 | 01/03/01 | Collapse | 13/06/01 | Cemented self-blocking | No. (Bicentric) | |
| Patient 12 | 61 | DHS 90 | 01/01/00 | Necrosis | 04/12/02 | Uncemented | Impacted | |
| Patient 13 | 72 | LNS | 23/04/05 | Pseudoarthrosis | 03/10/05 | Cemented trochanteric support | No. (Bicentric) | |
| Patient 14 | 80 | IMHS | 01/03/07 | Cut-out | 10/05/07 | Cemented self-blocking | Cemented retainer | |
| Patient 15 | 77 | GAMMA 3 | 18/04/10 | Cut-out | 07/06/10 | Uncemented | Cemented | |
| Patient 16 | 78 | GAMMA 3 | 02/12/10 | Cut-out | 17/01/11 | Cemented self-blocking | No. (Bicentric) | |
| Patient 17 | 85 | IMHS | 08/02/11 | Cut-out | 02/04/11 | Cemented self-blocking | No. (Bicentric) | Infection |
Early failure was defined as that which appeared in the 4 months following surgery, whilst late failure was defined as that occurring after 4 months. A total of 10 patients presented early failure of the system. In 9 of the 10 cases, the cause of the osteosynthesis failure was a cut-out, whereas in 1 case there was a collapse of the fracture and failure of the system. In the remaining patients, the time interval between the first surgery and implantation of arthroplasty was greater than 4 months. Overall, the mean time interval from osteosynthesis until failure and consequent implementation of arthroplasty was 8 months, with a range of 1–36 months.
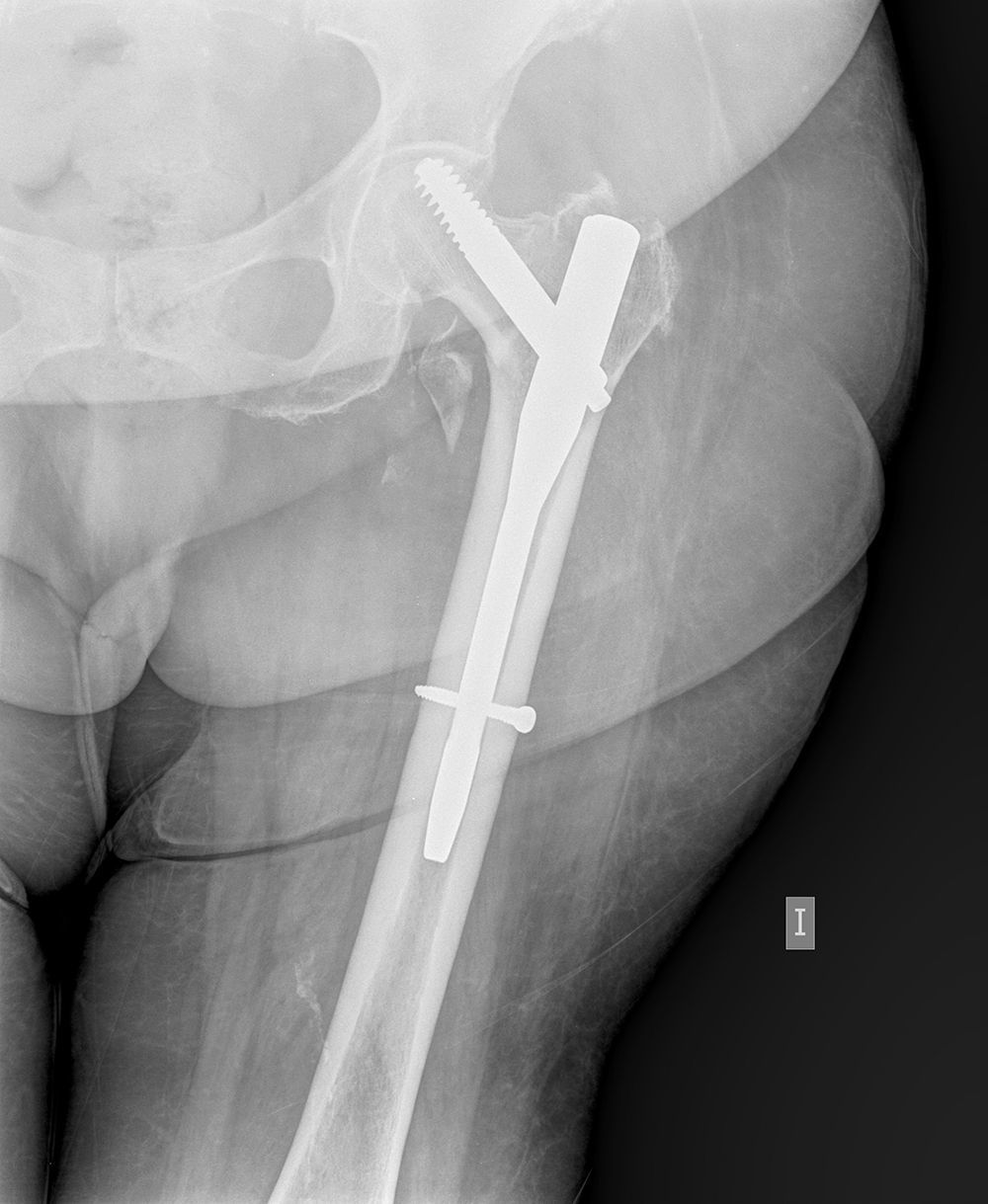
The cut-out phenomenon was the cause of failure of the synthesis in 10 of the 17 cases (59%), whilst a lack of fracture consolidation, nonunion, occurred in 4 cases (24%), in 2 of these associated with failure of the synthesis material (Fig. 1).
A total hip prosthesis was implanted in 8 of the 17 patients (47% of cases), while in the remaining 53% we implanted a bipolar hemiarthroplasty. The criteria for the use of one implant or the other were conditioned by the degree of damage to the acetabular cartilage and the general condition of each patient (Fig. 2). In 2 patients, we opted for implanting a constrained hip socket (acetabulum), in order to avoid problems with posterior dislocations, as these patients suffered incipient cognitive impairment. We used a posterior approach in all cases. The decision to perform hip replacement implantation in 1 or 2 stages was determined according to the clinical suspicion of infection of the prior osteosynthesis, as well as the result of the intraoperative histological study which was conducted in all cases in the series in order to rule out acute inflammation (Mirra criteria12).
Following these premises, in 16 patients we proceeded to implant the hip prosthesis in 1 stage, whereas in 1 patient surgery was performed in 2 stages.
In all patients we used a primary stem, in 3 cases for trochanteric support. Of these stems, 88% (15 of 17) were cemented, whereas 12% (2 of 17) were not cemented. We did not use long revision stems in any case.
In 8 cases (47%), reconstruction of the anatomy of the proximal third of the femur was completed with the use of cerclage.
All patients received preoperative antibiotic prophylaxis with 2g of first-generation cephalosporin in a single-dose, as well as postoperative thromboembolic prophylaxis for 30 days with low molecular weight heparin.
The mean follow-up period of patients after implantation of a hip arthroplasty was 6 years (range: 1–14 years). At each postoperative control (1 month, 6 months and annually), we evaluated pain, function and ambulation through the Merle d’Aubigné scale,13 as well as the ability to perform basic activities of daily living (Barthel test14). Adequate stability of the acetabular components, in those cases where they were implanted, and femoral components, both cemented and uncemented, was evaluated radiographically. Radiographic loosening of cemented acetabular components was evaluated using the criteria of Hodgkinson et al.15 Loosening of uncemented acetabular components was determined by the migration of the implant, the presence of a radiolucent line in the implant-bone interface or by the breakage of the acetabular screws. The stability of uncemented femoral implants was evaluated by the criteria of Engh et al.,16 while in the case of cemented implants we followed the criteria described by Harris et al.17 Similarly, we carried out a radiographic control of the evolution of trochanteric fractures treated with cerclage.
ResultsAt the time of the review of cases, 11 patients were still alive and 6 had died. One patient died in the postoperative period, while the remaining 5 died 30 months after surgery. None of them died from causes related to prosthetic surgery. The 16 evaluated patients were monitored for a mean period of 6 years (range: 1–14 years).
In total, 4 of the 17 patients (23%) presented medical complications during the postoperative period after prosthesis surgery. Two patients suffered urinary tract infection, 1 patient suffered an episode of angina and the fourth patient suffered acute kidney failure. Mortality during the first 30 days reached 6% (1 patient out of 17).
Two patients (12%) presented an acute infection of the arthroplasty (<30 days after surgery). In 1 case it was due to a polymicrobial infection, which required 2 surgical debridements and antibiotic treatment, and eventually required a Girdlestone-type resection arthroplasty, whilst the second case was an infection by Staphylococcus epidermidis, which required surgical debridement and 8 weeks of antibiotic therapy (rifampicin 600mg and trimethoprim-sulfamethoxazole orally), with a satisfactory outcome.
We did not observe cases of periprosthetic fractures or dislocations during follow-up.
Before implantation of the hip arthroplasty, all patients reported moderate or severe pain which limited ambulation. Excluding the deceased case and the Girdlestone procedure, all patients had recovered their autonomous ambulation at 6 months of prosthetic surgery.
In total, 13 of 15 patients (87%) reported mild hip pain or no pain, while the remaining 2 patients (13%) suffered localized pain in the region of the greater trochanter. These 2 patients presented radiological findings which revealed an absence of consolidation of the greater trochanter. The mean score on the Merle d’Aubigné scale13 was 14.13 points (range: 10–18 points).
The mean score in the Barthel scale14 prior to the fracture was 81 points, while at 8 weeks after the implantation of arthroplasty this increased to 66 points (range: 20–100 points), following osteosynthesis surgery and replacement of arthroplasty.
In 4 cases we performed a second surgery after implantation of the arthroplasty. Two patients presented an acute infection; 1 patient who had undergone implantation of a bipolar arthroplasty required the implantation of a cemented acetabular component due to a mechanical-type inguinal pain at 12 months after surgery and after a septic process had been ruled out. The other patient was reoperated due to aseptic loosening of the femoral component, which had to be replaced by a long stem with a distal diaphyseal anchor, 6 years after its implantation.
We did not observe any of the criteria by Hodgkinson et al.15 which could reveal loosening of the cemented acetabular components. We observe neither the migration of any of the uncemented acetabular implants, nor presence of radiolucent lines in the implant-bone interface or breakage of the acetabular screws.
According to the criteria by Engh et al.16 and Harris et al.17 we only observed 1 case of aseptic loosening of a cemented femoral stem (6%), caused by a rupture of the cement mantle.
In 8 cases, reconstruction of the proximal femur was completed with the use of cerclage. In subsequent controls we observed pseudoarthrosis in 3 of the 17 total patients (18%), coinciding with pain in that region in 2 of the cases, without having considered any further treatment. The third patient is currently asymptomatic despite the lack of consolidation.
DiscussionFollowing the failure of a previous osteosynthesis, the implantation of a hip arthroplasty as a solution allowed pain relief and effective functional recovery in the majority of patients in the present study. Despite being a demanding surgery, there were few long-term complications related to the femoral prosthetic implant, with only 1 case (6%) of aseptic loosening being recorded.
In the last decade, the literature on the use of hip arthroplasty as a treatment for failure of osteosynthesis of pertrochanteric fractures has reported similar results to ours in terms of functionality and rate of revisions. Zhang et al. presented a retrospective study in which 19 patients underwent implantation of a hip prosthesis after failure of a previous osteosynthesis. A conventional femoral stem was used in all patients. These authors observed an increase of 40 points in the Harris scale (from 38.4 to 79.8) and none of the patients had to undergo reoperation after a mean follow-up period of 7.4 years.18 Thakur et al. published a study in which 15 patients were treated with a long, uncemented, modular stem, with an increase of almost 50 points in the Harris scale (from 35.90 to 83.01) and only 1 reported case of loosening, after a mean follow-up period of 2.86 years.10 In the series published by Talmo and Bono, all patients reported an effective relief of pain and recovery of ambulation after 30 months of follow-up. The mean score in the Harris scale was 86 points, with a single case of loosening of the femoral stem (10%).11
All published studies refer various technical difficulties that may be encountered in these cases. As noted by Syed et al., this surgical procedure is not without complications and various factors should be taken into account in order to obtain satisfactory results.19
The first of these factors is the occasional difficulty presented by the extraction of the previous synthesis. Bone loss at the calcaneus level is common and may force the use of implants which replace the bone defect in an attempt to maintain the length of the limb or else the proximal part of the stem to be left without support or with unstable support. Haidukewych and Berry used stems with calcaneus substitution in 58% of cases9 while Mortazavi et al. used these stems in 76% of cases.20 Secondly, most authors consider the use of revision stems with distal diaphyseal anchoring to achieve a “bypass” effect of the cortical defects and orifices left by the synthetic material. Haidukewych and Berry recommend the use of the femoral head to fill cortical defects, in an attempt to avoid cement pressurization and leakage problems, as well as the use of long stems in 22% of patients.9 Mortazavi et al. used long stems in 50% of cases in order to overcome distal cortical defects.20 D’Arrigo et al. implanted long revision stems in 14 of 19 patients (73%).8 However, in our study we only observed 1 case of aseptic loosening of a cemented femoral stem (at 6 years of implantation), despite the fact that, using conventional stems, we did not exceed the most distal orifices and did not occlude them with a femoral head autogenous graft. Since the majority of patients in our study had been previously treated with antegrade intramedullary nailing, the number of distal cortical orifices was lower than that observed after removing a screw-plate system. Likewise, Zhang et al., who also used conventional stems in the 19 patients in their series, did not have to conduct any revision surgical procedures secondary to mechanical failure of the implant.18 Finally, there have also been reports of intraoperative periprosthetic fractures, originating from the distal diaphyseal orifices remaining after primary osteosynthesis. Milling of the medullary canal and the need to obtain a correct distal diaphyseal anchoring could be the cause of these fractures. Mehlhoff et al. conducted a study in which 13 hip arthroplasties were implanted after failure of the prior osteosynthesis, and reported 2 intraoperative periprosthetic fractures.21 In the study published by D’Arrigo et al. there was also 1 intraoperative periprosthetic fracture, out of a total of 21 intervened patients.8 In our study, the implantation of a conventional stem, in most cases cemented, allowed us to simplify the surgical procedure, reducing the potential risk of intraoperative periprosthetic fracture. Moreover, as outlined by Zhang et al., although the length of the femoral stem did not exceed the distal diaphyseal orifices, we observed no stress fractures during the follow-up period.18
Two patients in our series (12%) required reoperation due to periprosthetic infection. Haidukewych and Berry reported a total reoperation rate of 8% (5 out of 60 patients), with only 1 patient suffering surgical wound problems.9 In the series of Mortazavi et al., 11 patients (7%) required reoperation due to presenting persistent drainage of the surgical wound.20 Srivastav et al. published a series of 21 patients in which 2 of them were reoperated due to superficial or deep infection (9.5%).22
One of the most commonly reported complications in the literature is dislocation of the arthroplasty. In our series, there have been no cases so far, although we have used constrained acetabular components on 2 occasions and bipolar arthroplasties on 9. Zhang et al. presented a postoperative dislocation rate of 16%.18 In the study by Mehlhoff et al. there were 3 dislocations (23%) out of 13 patients.21 Haidukewych and Berry reviewed 60 patients and only observed 1 dislocation (2%).9
As noted by Mortazavi et al., patients requiring hip arthroplasty as a treatment for failure of a previous osteosynthesis often present associated medical complications. This is to be expected, since the average age of these patients is usually higher than that of patients in whom primary hip arthroplasties are implanted. Moreover, it is a more complex surgery, with a prolonged surgical time and increased blood loss volume.20 In our series, 4 out of 17 patients (23%) suffered some form of medical complication, a percentage similar to that observed by Haidukewych and Berry in their series, in which the rate of medical complications was 20%.9
Most of the implants were functional, with good clinical and radiographic results being observed, bearing in mind that these patients suffered impaired functional capacity, as reflected by the decrease in the Barthel test score from 81 points prior to fracture to 66 points after 2 interventions: osteosynthesis and arthroplasty.
Our study has room for improvement. Firstly, it was a retrospective study, which entails inherent limitations. The long follow-up period implied a loss of some of patients due to death during the study. Moreover, the primary osteosynthesis employed a wide variety of implants and involved different groups of surgeons. However, we do not believe that these weaknesses should condition the conclusions drawn from the study. Moreover, the study has several strengths. It is one of the few studies in which all patients were intervened using the same posterolateral approach and in which all the stems used were conventional primary stems, cemented or uncemented, with no revision stems being used. Lastly, the mean follow-up period of patients after implantation of hip arthroplasty was over 5 years.
In conclusion, we have observed that the use of conventional stems, cemented or uncemented, may be a good option to treat failures of osteosynthesis of pertrochanteric femur fractures. This procedure facilitates revision surgery and enables satisfactory functional and radiographic results in patients with limited functional demands and significant, associated comorbidity.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Castillón P., et al. Artroplastia de cadera con vástago convencional en fracasos de osteosíntesis de fracturas del fémur proximal. Rev Esp Cir Ortop Traumatol. 2013;57:194–200.