Distal humerus fractures in the elderly frequently associated with poor bone quality and comminution, making it harder to achieve proper osteosynthesis. Our aim is to evaluate the radiological and functional results of open reduction and internal fixation of these fractures.
Material and methodsRetrospective study of 26 patients treated by open reduction and internal fixation between the years 2005 and 2010. Mean follow-up was 42 months. At final follow-up, a radiography evaluation (Knirk and Jupiter score) and clinical examination using Mayo Elbow Performance Score and Quick-Disabilities of the Arm, Shoulder and Hand Score was performed. Mean age of the group was 76.8 years (65–89), with 83% of the patients being female. Sixteen patients suffered type C fractures and 8 type A by AO classification. All underwent posterior surgical approach.
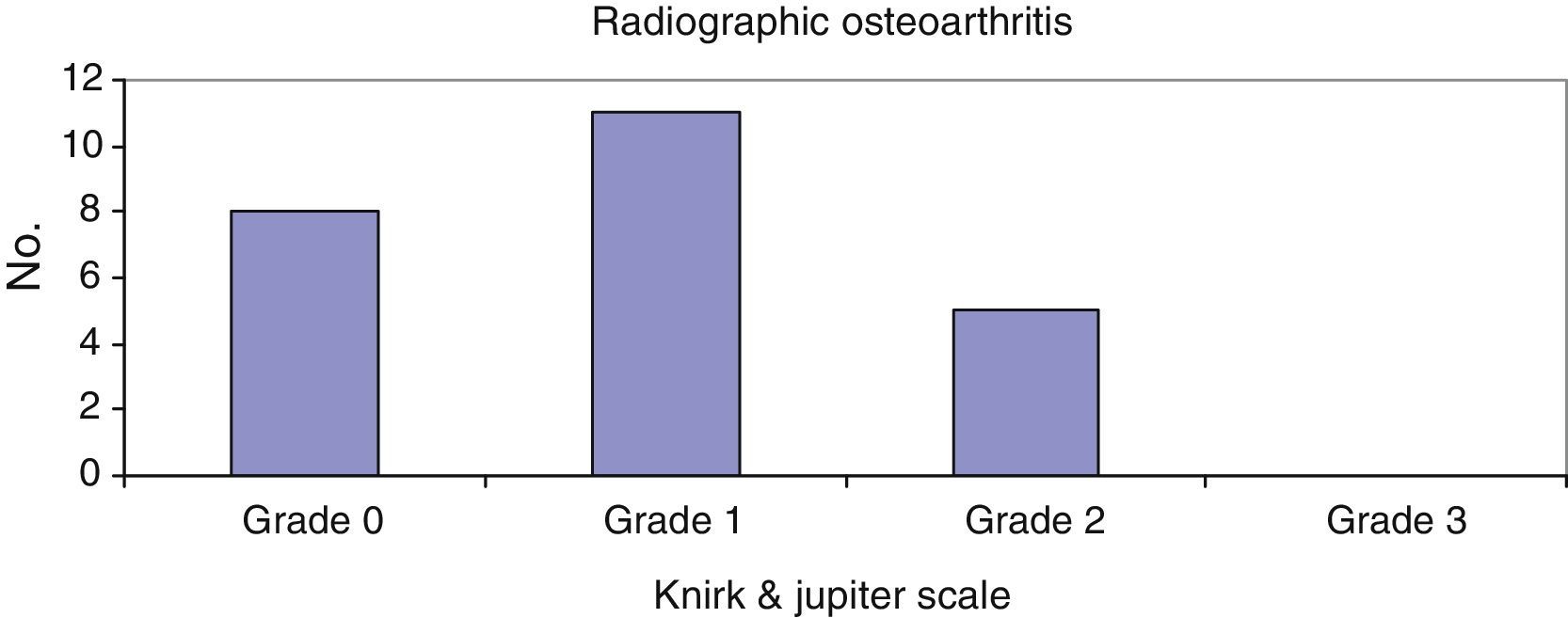
ResultsMean elbow flexion reached 118.86°, with a mean extension deficit of 25°. More than 3 quarters (79.1%) of the patients showed 0–1 grade degenerative changes on the X-ray films at final follow-up. Functional results reached an average 19.87 points on Quick-Disabilities of the Arm, Shoulder and Hand Score, and 85 points on Mayo Elbow Performance Score. Non-union occurred in 2 cases: distal humerus in one patient and olecranon osteotomy in another. Ulnar nerve neuropraxia was recorded in 2 cases, and radial nerve in one. All 3 recovered uneventfully. Revision surgery was required, with 2 patients needing hardware removal and one a new fixation.
DiscussionTreatment by open reduction and internal fixation with plating in elderly people for type A and C distal humerus fractures gives good functional results regarding this population, and thus scarcely disturbs their quality of life.
Las fracturas de húmero distal en ancianos asocian mala calidad ósea y gran conminución, lo que teóricamente dificultaría la síntesis de las mismas. Nuestro objetivo es evaluar los resultados radiológicos y funcionales del tratamiento mediante reducción abierta y fijación interna de estas fracturas.
Material y métodosEstudio retrospectivo entre los años 2005-2010 de 26 pacientes tratados mediante reducción abierta y fijación interna. Seguimiento medio de 42 meses. Al finalizar el mismo se realizó una valoración radiográfica (Knirk and Jupiter scale) y funcional mediante las escalas Mayo Elbow Performance Score y Quick-Disabilities of the Arm, Shoulder and Hand Score. La edad media fue de 76,8 años (65-89) siendo el 83% mujeres. Se encontraron 16 pacientes con fractura tipo C y 8 tipo A (según la AO). Todos fueron tratados mediante abordaje posterior.
ResultadosLa flexión media fue de 118,86° con un déficit de extensión medio de 25°. El 79,1% de los pacientes presentaban un grado 0-1 de artrosis. La media obtenida en las escalas funcionales fue: Quick-Disabilities of the Arm, Shoulder and Hand Score: 19,87; Mayo Elbow Performance Score: 85. Encontramos 2 casos de seudoartrosis: una de húmero distal y otra de la osteotomía del olécranon. Hallamos 2 casos de neuroapraxias cubitales y una radial que se recuperaron sin secuelas. Hubo 3 reintervenciones: 2 retiradas de material y un caso de nueva osteosíntesis.
DiscusiónEl tratamiento con reducción abierta y osteosíntesis con placa para las fracturas tipo A y C de húmero distal en ancianos proporciona unos resultados funcionales satisfactorios para las demandas de este tipo de paciente, lo que altera escasamente la calidad de vida percibida por los mismos.
Fractures of the distal humerus present an incidence of 5.7 per 100,000 people/year distributed in a bimodal form (young people as a result of high-energy traumatisms and a second peak in elderly women, with osteoporotic bone, secondary to low-energy traumatisms). The latest epidemiological data show a considerable increase of this type of fractures in patients aged over 65 years in the last decade.1
There is a controversy over what the ideal treatment to follow in this type of fractures in the elderly. Added to the greater complexity from the comminution associated with them is the problem of fixation of osteosynthesis material in a bone with its altered biomechanical and biological characteristics, which encourages implant failure and alters the process of consolidation. In many occasions, this makes it necessary to have a greater period of joint immobilization after fracture fixation, with the functional repercussions that involves. All of this has made the treatment of these fractures the object of debate in the literature, with opposing therapeutic attitudes that vary from conservative treatment to open reduction or elbow arthroplasty.2,3
The objective of this study was to analyze the functional and X-ray results, along with the complications associated, of open reduction and osteosynthesis with internal plating for this type of fractures in patients aged more than 65 years.
Material and methodsStudy populationWe performed a retrospective study on the patients who had suffered distal humerus fracture (supracondylar and supra-intercondylar humerus) in the period 2005–2010 in our center. The criteria for inclusion were: patients aged more than 65 years with this type of fracture treated using internal fixation. There were 26 patients who fulfilled these criteria. Twenty-four of the 26 patients were located by telephone and given appointments to receive an X-ray and functional assessment. The 2 patients lost to follow-up were 2 deaths due to causes unrelated to the fracture. Mean follow-up up to the final interview was 42 months (from 15 months to 7 years). Mean patient age was 76.8 years (65–89) and 83% of the patients were women.
Of the 24 patients included in the study, we found 16 cases of intra-articular fractures (Type 13 C1–C3 using the AO classification) and 8 cases of extra-articular fractures (Type 13 A1–A3).
The lesions were caused by own-height falls in all the cases. In 21 of the cases, the fractures were isolated humerus fractures. In 3 cases, there were associated lesions: fracture of the ipsilateral radial head, the ipsilateral coronoid, and the ipsilateral Galeazzi. All cases were closed fractures.
Surgical techniqueThe surgery was carried out in all the cases using a posterior approach. Olecranon osteotomy was performed in 14 of the patients (all with a Type C fracture pattern) and with transtriceps approach in 10 (2 of which had nondisplaced intra-articular involvement demonstrated using computed axial tomography (CAT scan); the other 8 cases were Type A). Various types of implant were used. Mayo plates (Acumed®, Hillsboro, OR, USA) were the most numerous (n=17, using 2 parallel plates in 58.8% of the cases, orthogonal placement in 23.5%, and a single plate in the remaining 17.6%), followed by LCP type (DePuy Synthes, West Chester, PA, USA) (5 cases, in orthogonal placement) and reconstruction plates (DePuy Synthes, West Chester, PA, USA) (2 cases in parallel). The olecranon osteotomy was fixed with transolecranon stems in 3 cases and tension band cerclage in 11.
The ulnar nerve was exposed routinely and 2 anterior subcutaneous transpositions were performed. No patient received a bone graft. The wounds were closed after abundant lavage, without leaving drainage in any of the cases.
Antibiotic prophylaxis was given in all cases, using cefazolin before surgery (2g i.v.) and postoperatively (2g i.v. in 2 doses).
Postoperative periodThe mean hospital stay was 3.5 days. We immobilized the elbow with a brachial splint for 7–10 days, after which the patients began elbow mobilization under doctor's orders. All of the patients, except for 2, received physical therapy rehabilitation in the hospital center after removal of the post-surgical immobilization.
Radiographic and functional assessmentFor the radiographic assessment, simple X-rays and/or CAT scans were assessed pre-surgically to analyze the fracture pattern and classification using the AO system.4
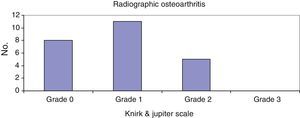
Likewise, during the postoperative period a control X-ray study was performed during the patient interview. Using 2 elbow projections (anteroposterior and lateral), we assessed radiographic consolidation, state of the osteosynthesis material (migration, breakage), and the degree of osteoarthritis according to the Knirk and Jupiter scale.5
Functional assessment was effected by measuring the range of mobility with a manual goniometer, evaluating elbow stability, and using the scales of the Mayo Elbow Performance Score (MEPS)6 (that assesses the arc of joint mobility, stability and functionality of the elbow and the presence or absence of pain) and the Disabilities of the Arm, Shoulder and Hand (DASH)7 (that assesses the degree of disability).
ResultsFunctional evaluationMean joint balance was 118.86° in flexion (70–140°) and 25° in extension deficit (0–40°). There were no final limitations in pronation/supination in any cases, not even in those that presented associated fractures of the radial head, coronoid, or distal ulna. There was no elbow instability after forcing elbow varus/valgus.
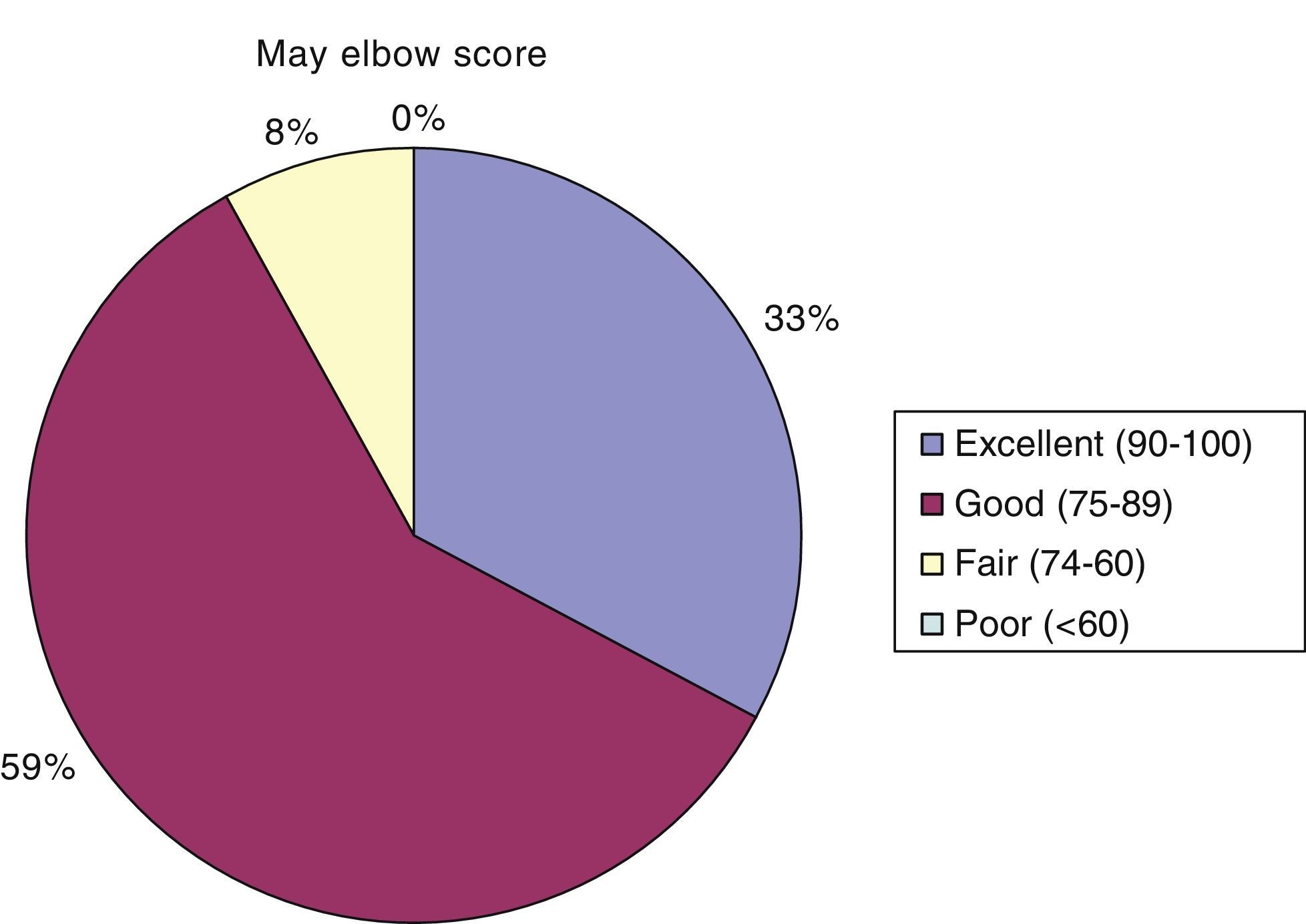
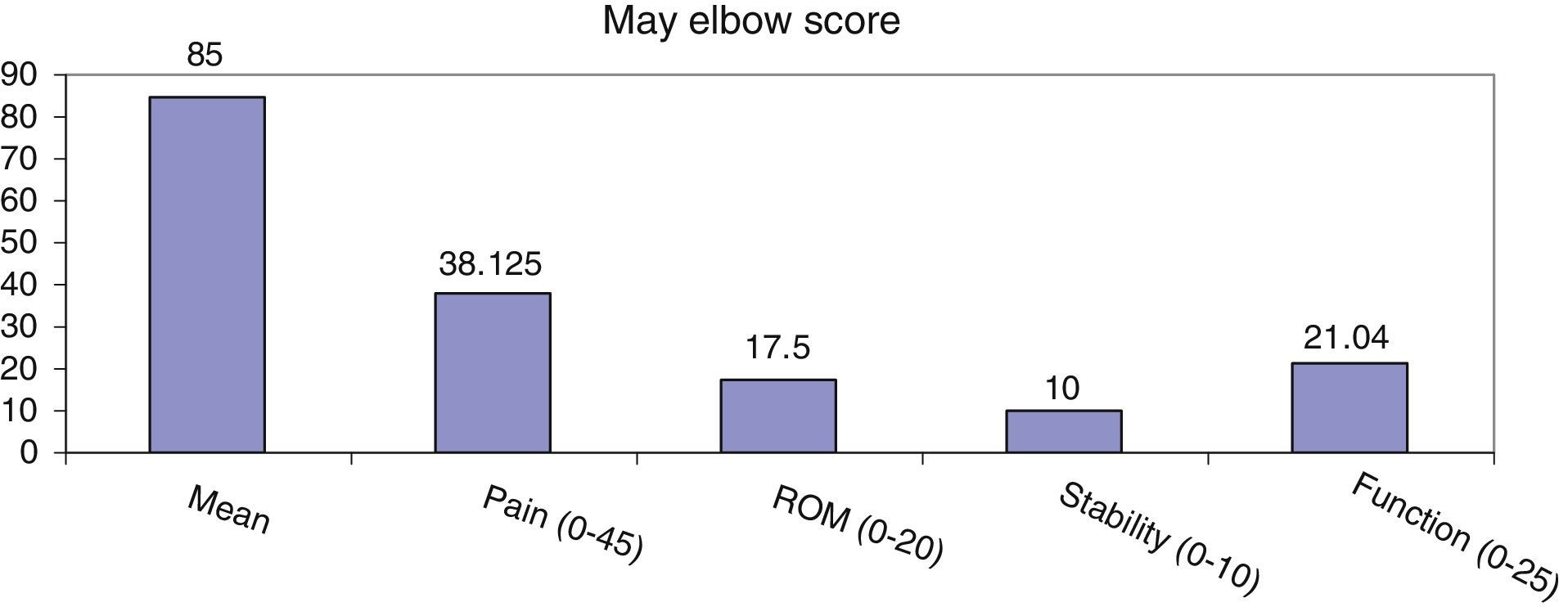
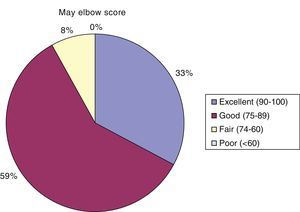
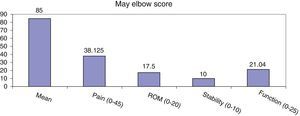
At the end of follow-up, the mean DASH score was 19.87 (range, 0–63.63). Mean MEPS scale outcome was 85; there were 8 patients with a mean excellent result (90–100), 14 with good (75–89), and 2 patients with a fair result (60–74) (Fig. 1).
The score obtained in the various parameters that the scales used measure are shown in Figs. 1 and 2.
Radiographic assessmentThe assessment of the degree of X-ray osteoarthritis at the end of follow-up showed that 79.1% of the patients presented Grade 0 or 1 (Fig. 3).
All the fractures consolidated except one, which remained as painless pseudo-osteoarthritis in a patient with scant functional demands. In another case, the osteotomy of the olecranon lacked consolidation as well. The patients did not require reoperation in either of these cases.
ComplicationsWith respect to complications directly related to the osteosynthesis material, we found 1 case in a Type A fracture that required reosteosynthesis 1 month after surgery due to displacement from insufficient initial fixation (single posterior plate). The patient was reoperated after 1 month, removing the first implant and synthesizing the fracture again with 2 parallel Mayo plates. In addition, 1 of the tension bands from an olecranon osteotomy was removed and a stem from a plate was extracted due to migration. The osteotomy was consolidated and, in the case of the stem migration, it was unnecessary to remove the rest of the osteosynthesis material.
In the immediate postoperative period, we found 2 cases of surgical wound infection. These were treated with antibiotic therapy, evolving favorably.
Other complications were 2 ulnar neuroapraxias and 1 radial neuropraxia. These recovered fully during follow-up without any associated sequelae (see the summary in Table 1).
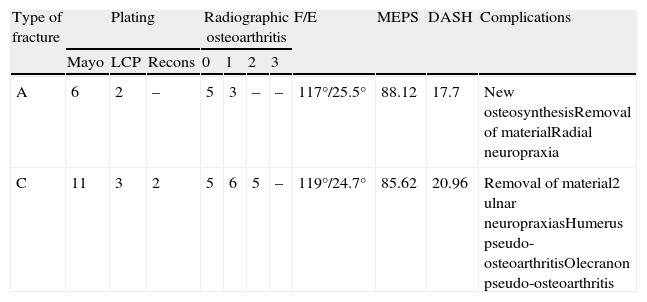
Results and complications according to fracture type.
| Type of fracture | Plating | Radiographic osteoarthritis | F/E | MEPS | DASH | Complications | |||||
| Mayo | LCP | Recons | 0 | 1 | 2 | 3 | |||||
| A | 6 | 2 | – | 5 | 3 | – | – | 117°/25.5° | 88.12 | 17.7 | New osteosynthesisRemoval of materialRadial neuropraxia |
| C | 11 | 3 | 2 | 5 | 6 | 5 | – | 119°/24.7° | 85.62 | 20.96 | Removal of material2 ulnar neuropraxiasHumerus pseudo-osteoarthritisOlecranon pseudo-osteoarthritis |
Osteoporotic bone differs from healthy bone biologically in that it presents lower mineral density (which mainly affects spongy bone), which makes it biomechanically inferior.8 This also gives it less resistance, especially to the axial compression forces, facilitating the presence of complex fracture patterns that affect epiphyseal–metaphyseal areas (Type C fractures) with greater frequency. In osteosynthesis, this translates into vacant areas that make it easier for the implant to fail.9 We defined osteoporotic bone according to the presence or absence of risk factors.10,11 These features make treating these fractures in the elderly a subject for debate in the literature, with therapeutic attitudes that can range from a conservative treatment, an open reduction plus osteosynthesis, or an elbow arthroplasty.
The appearance of new implants designed specially for osteoporotic bone has been a revolution in this sense, decreasing postoperative immobilization time and preventing the appearance of important joint rigidities. In spite of this, some authors defend the performance of a total elbow arthroplasty as the initial treatment in the elderly. McKee et al.12 carried out a randomized prospective study with 42 patients aged over 65 years with Type C fractures treated by arthroplasty or osteosynthesis with a mean follow-up of 2 years. Patients in the arthroplasty group showed significant improvement in the MEPS scale results both at the beginning and at 2 years of follow-up. However, the results obtained for the DASH scale were the same for both groups at 1 year after the operation. Although the range of reoperation in the osteosynthesis group was higher (27% against 12%), the differences in this aspect were not statistically significant.
Likewise, Frankle et al.3 compared the results for both functional and mobility in 2 groups of patients older than 65 years treated using internal fixation or arthroplasty in Type C fractures. They recommend the use of total elbow arthroplasty in elderly patients with significant comminution and in those with underlying pathology (rheumatoid arthritis, chronic steroid use, etc.). However, they maintain the recommendation of internal fixation with plates for patients with good bone reserves.
Although in our series, as in others,13 the complications directly related to failure of osteosynthesis material are not high, there are series gathering figures of up to 29.5%.14 It is precisely these high rates of complications with the osteosynthesis material that encourage some authors to use arthroplasty as the initial treatment for these fractures. In our study we found 3 (12.5%) complications derived directly from problems with the osteosynthesis material (break or migration). Two of these complications were minor (1 removal of a tension band and 1 of a stem) without affecting the course or the natural development of the fracture, while the other complication required a new synthesis because the first one turned out to be insufficient.
Another of the parameters that defenders of arthroplasty as initial treatment for these fractures is the presence of less pain following its implantation than following the performance of an open reduction.3–12 However, the patients in our series presented a mean of 38.12, the entire set falling among the groups with slight or absent pain according to the MEPS scale. These results coincide with those obtained by other authors, with means of 41.715 and 41.85.16
It is true that the immediate functional results obtained after the arthroplasty were favorable in these studies. However, we should interpret them with caution and bear in mind the long-term complications of elbow prostheses, above all those related to component removal and periprosthetic fractures.17,18
In the postoperative period, we maintained immobilization in all the cases for less than 10 days and with exclusively analgesic and anti-inflammatory purposes. Just as in other studies,1–19 we consider this essential for rapid recovery of function in elbow surgery on the elderly patient.
Pseudo-osteoarthritis rates after surgical treatment of fractures of the distal humerus are found in the range of 0–11%.1 In our series, in spite of the fact that osteoporotic bone is a bone at greater risk of presenting alterations in consolidating (delay or pseudo-osteoarthritis), all of the humerus fractures except 1 (4.16%) consolidated.
Insofar as infection rates in elbow arthroplasty (a complication that is devastating), they are approximately 7–16%12–18; these are slightly higher than those found for osteosynthesis, which are about 2–13%,12–19 In our series, we found 2 cases of superficial infection (8.3%), which were solved with antibiotic therapy, and 0 cases of deep infection. We consider that appropriate closure with good coverage of osteosynthesis material and pre- and post-surgery antibiotic prophylaxis is essential for preventing this type of complication. In our center, we use cefazolin pre-surgically (2g) and post-surgically (2g in 2 doses) as the protocol.
The presence of symptoms related to the ulnar nerve is another fact to bear in mind. The incidence of severe ulnar neuropathy after prosthesis implantation is approximately 5%,17–20 although it can vary between 2% and 26%18 (this variability is probably due to the lack of mention of purely sensitive problems in many of the studies). In osteosynthesis, the percentage of ulnar neuropraxia is considerably lower, oscillating between 0%2 and 6.25%.15 In our study, we found 2 cases of ulnar neuropraxia (8.3%), and the nerve was left in situ in both cases; its systematic transposition is controversial, with up to 4 times greater possibility of neuritis being described.21
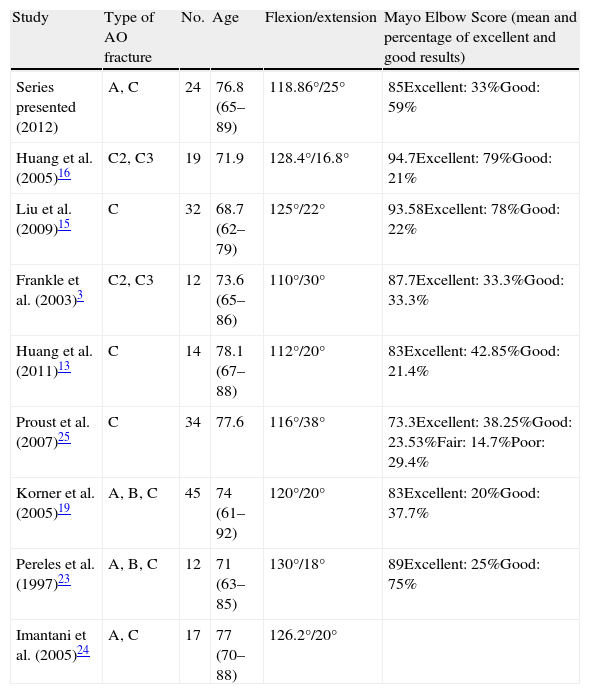
Although there is a consensus in the literature as to the fact that advanced age is not a contraindication per se for carrying out a synthesis, we found few studies about the subject.3,13,16,19,23,24 Our functional results were excellent or good in 92% of the patients; this is in keeping with those obtained by other authors (Table 2), some of whom managed to obtain up to 100% of good and excellent results in their series.15,16
Comparison of series of elderly patients with fractures of the distal humerus under treatment with osteosynthesis.
| Study | Type of AO fracture | No. | Age | Flexion/extension | Mayo Elbow Score (mean and percentage of excellent and good results) |
| Series presented (2012) | A, C | 24 | 76.8 (65–89) | 118.86°/25° | 85Excellent: 33%Good: 59% |
| Huang et al. (2005)16 | C2, C3 | 19 | 71.9 | 128.4°/16.8° | 94.7Excellent: 79%Good: 21% |
| Liu et al. (2009)15 | C | 32 | 68.7 (62–79) | 125°/22° | 93.58Excellent: 78%Good: 22% |
| Frankle et al. (2003)3 | C2, C3 | 12 | 73.6 (65–86) | 110°/30° | 87.7Excellent: 33.3%Good: 33.3% |
| Huang et al. (2011)13 | C | 14 | 78.1 (67–88) | 112°/20° | 83Excellent: 42.85%Good: 21.4% |
| Proust et al. (2007)25 | C | 34 | 77.6 | 116°/38° | 73.3Excellent: 38.25%Good: 23.53%Fair: 14.7%Poor: 29.4% |
| Korner et al. (2005)19 | A, B, C | 45 | 74 (61–92) | 120°/20° | 83Excellent: 20%Good: 37.7% |
| Pereles et al. (1997)23 | A, B, C | 12 | 71 (63–85) | 130°/18° | 89Excellent: 25%Good: 75% |
| Imantani et al. (2005)24 | A, C | 17 | 77 (70–88) | 126.2°/20° |
With respect to the range of mobility obtained after osteosynthesis, we observed a decrease in the arc of mobility mainly affecting flexion-extension (mean of 118.86° of flexion and 25° of deficit in extension) with slight incidence on pronation–supination. This drop in the arc of mobility (already indicated in previous series,3–24 as the assessment scale demonstrate) is sufficient for the functional requirements of this type of patients, barely altering the quality of life that they perceive.
Our study has several limitations. It is a retrospective study, it includes articular and extra-articular fractures, and the number of patients is relatively small. However, in spite of these limitations, the results obtained show that the treatment of fractures of the distal humerus with appropriate osteosynthesis in patients aged more than 65 years in whom early mobilization is initiated yield good functional results with few complications and reoperations. That is why we recommend osteosynthesis whenever its performance is possible, reserving total elbow arthroplasty just for elderly patients with scant functional requirements who present fractures on which performing a reconstruction is impossible.
Level of evidenceLevel of evidence 4.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments on human beings or animals were performed for this research.
Data confidentialityThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Serrano-Mateo L, Lopiz Y, León-Serrano C, García-Fernández C, López-Durán-Stern L, Marco F. Resultados de la reducción abierta y osteosíntesis de fracturas de húmero distal en mayores de 65 años. Rev Esp Cir Ortop Traumatol. 2014;58:31–37.