The sexual life of a couple is a dynamic entity, in which the two influence each other mutually, thus the existence of female sexual dysfunction (FSD) can influence the treatment of the man who seeks clinical help. Identify sexual dysfunction in female partners of patients attending an andrology clinic may provide a therapeutic opportunity. The authors aim to assess proportion of FSD in this population by comparison with a control group.
Material and methodsA longitudinal study over 12 months timespan. The female partners of patients attending the andrology clinic participating in the study (study group – SG) completed the Female Sexual Function Index (FSFI), as did the women serving as controls (control group – CG). Further data such as age, duration and quality of the relationship and previous relationships was also collected.
ResultsOf the 30 women included in the SG, 14 (46.6%) considered that their current sex life was worse than in previous relationships. Of the 20 women in the CG, 60% considered that their current sex life was better. In the SG, 22 (73.3%) had FSD, with a mean score in the FSFI of 20.5, whereas only 3 women in the CG (15%) had FSD, with a mean score of 30.7 (p<0.01).
ConclusionsOur study demonstrated that the proportion of FSD in female partners of patients attending an andrology clinic is significantly higher than control group. FSD treatment should be considered as a therapeutic opportunity for the couple in this setting.
La vida sexual de una pareja es una entidad dinámica, en la que ambos se influyen mutuamente, por lo que la existencia de disfunción sexual femenina (DSF) puede influir en el tratamiento del hombre que busca ayuda clínica. Identificar la disfunción sexual en las parejas femeninas de los pacientes que asisten a una Clínica de Andrología puede brindar una oportunidad terapéutica. Los autores pretenden evaluar la proporción de DSF en esta población comparándola con un grupo de control.
Material y métodosEstudio longitudinal durante 12 meses. Las parejas femeninas de los pacientes que asistieron a la Clínica de Andrología y que participaron en el estudio (grupo de estudio) completaron el Índice de Función Sexual Femenina, de la misma forma que las mujeres, que sirvieron como control (grupo de control).
También se recopilaron datos adicionales como edad, duración, calidad de la relación y las relaciones entre los anteriores.
ResultadosDe las 30 mujeres incluidas en el grupo de estudio, 14 (46,6%) consideraron que su vida sexual actual era peor que en relaciones anteriores. De las 20 mujeres del grupo control, el 60% consideró que su vida sexual actual era mejor. En el grupo de estudio, 22 (73,3%) tenían DSF, con una puntuación media de Índice de Función Sexual Femenina de 20,5, mientras que solo 3 mujeres en el grupo control (15%) tenían DSF, con una puntuación media de 30,7 (p <0,01).
ConclusionesNuestro estudio demostró que la proporción de DSF en parejas femeninas de pacientes que acuden a una Clínica de Andrología es significativamente mayor que en el grupo control. El tratamiento de la disfunción sexual femenina debe considerarse como una oportunidad terapéutica para la pareja en este escenario.
Male sexual dysfunction has a negative impact on the quality of life of both the individual and his/her sexual partner.1,2 Several studies have shown that erectile dysfunction (ED), premature ejaculation (PE) or hypoactive sexual desire may have a negative impact on the sexual life of the partner.3–5
On the other hand, some studies have shown that FSD is associated with the sexual function of their partners.6,7 Vaginismus,8 dyspareunia,9 hypoactive sexual disorder10 as well as female orgasmic disorder10 in an individual are associated with an increased risk of ED and premature ejaculatory dysfunction in their male partner.
The European and North American Clarifying Vaginal Atrophy's Impact on Sex and Relationships (CLOSER) study revealed that postmenopausal vaginal atrophy (VA) adversely affects both members of the couple. According to women, symptoms of VA led them to avoid intimacy (62%), have less sex (58%), and have less satisfying sex (49%). Men were more likely to say they avoided intimacy (76%) and had less sex because of their partner's VA (61%), but less likely to report diminished satisfaction (28%).11,12
Since the classical studies of Masters and Johnson, it is very well known that, in a relationship, the partner is always involved when sexual dysfunction is present.13 According to Basson14 (2005) and Masters and Johnson (1966), human sexual response endorsements are based on a circular model (being able to experience sexual desire from sexual arousal), and sexual excitement based on a linear model (sequential sexual arousal follows the sexual desire), respectively. The disruption of these phases leads to female sexual dysfunction and further interferes with her partner's sexual performance and reinforces the male sexual dysfunction (MSD).23
Thus, the sexual life of a couple is a dynamic entity, in which the two partners influence each other mutually, so it is natural that the existence of FSD caused or aggravated by the male factor can decisively affect the attempted treatment of the man who seeks the andrology clinic.7,15,16
There have been few studies on the prevalence of FSD as a factor that may influence the diagnostic and therapeutic approach to male sexual dysfunction.2,3 This study aims to identify the proportion of FSD in female partners of patients attending the andrology clinic and compare them with a control group.
We used a validated Portuguese version of Female Sexual Function Index (FSFI). The FSFI has been validated and replicated in multiple studies and evaluates desire, arousal, lubrication, orgasm, satisfaction and pain during sexual intercourse.18 The FSFI clinical cut-off score has been widely used as an index to aid in distinguishing between women with and without clinical sexual dysfunction. An overall score of less than 26.55 is considered indicative of FSD.
To identify the proportion of FSD we asked Forty-eight patients who attended the andrology clinic to give their partners the FSFI questionnaire, of these 30 (62.5%) returned it correctly completed (study group). The average age was 44.1 years (26–63 years) and the average duration of the relationship was 14.1 years (1–42 years). The 20 women who agreed to participate in the study as a control group had a mean age of 39.45 years (28–54 years) and a mean relationship length of 13.6 years (1–29 years).
Material and methodsTo carry out this research study, the female partners of patients attending the andrology clinic, aged 18 years or older, were asked to complete the Portuguese version of the Female Sexual Functioning Index (FSFI).17 Women who reported not having had sexual intercourse in the last 4 weeks were not considered for the study (study group). All types of male sexual dysfunction were included.
We used a convenience sampling and the same questionnaires were distributed to women who served as controls (control group), volunteers selected at random from among the hospital staff, aged 18 years or older, with a stable relationship of at least one year duration, with partners who did not present known sexual dysfunction. Also, women who reported not having had sexual intercourse in the last 4 weeks were not considered for the study.
ProcedureThe FSFI, which is a self-administered questionnaire, composed of 19 questions with the aim of assessing human female sexual function in clinical studies was distributed to women in study group and in the control group. The FSFI evaluates the following domains: desire, arousal, lubrication, orgasm, satisfaction and pain during sexual intercourse.18 The maximum weighted score in each domain is 6 points, and the maximum global score in the 6 domains is 36 points. An overall score of less than 26.55 is considered indicative of FSD.8
Socio-demographic information was also collected such as age, education, existing illnesses, as well as the duration of the current relationship and information on whether the current relationship is better, worse or the same as previous relationships, regarding to sexual life.
In compliance with the Declaration of Helsinki, all participants were informed of the contents of the questionnaire and of the fact that participation was voluntary and confidential. They were also asked to sign an informed consent form. No financial incentive was offered to any of the participants.
Statistical analysisThe internal consistency was done through Cronbach's alpha for the global scale (alpha=0.98). By domain of the FSFI scale, the alpha values are as follows: alpha desire=0.76; alpha excitation=0.98; Lubrication=0.97; alpha orgasm=0.94; alpha satisfaction=0.91and alpha pain=0.98.
The statistical analyses were conducted in Statistical Package for Social Sciences (SPSS) software (version 25) for macOS. The statistical analysis consisted in a descriptive analysis to the FSFI scores in the clinical and control groups through central tendency and dispersion statistics. The FSFI scores were also described for central tendency and dispersion for each FSFI domain according to the normative scores. These scores were then compared using parametric tests for comparing the clinical vs. control group. Independent t Student tests were performed for each statistical comparison on FSFI domains. The alpha level was set at 0.05 for statistical significance.
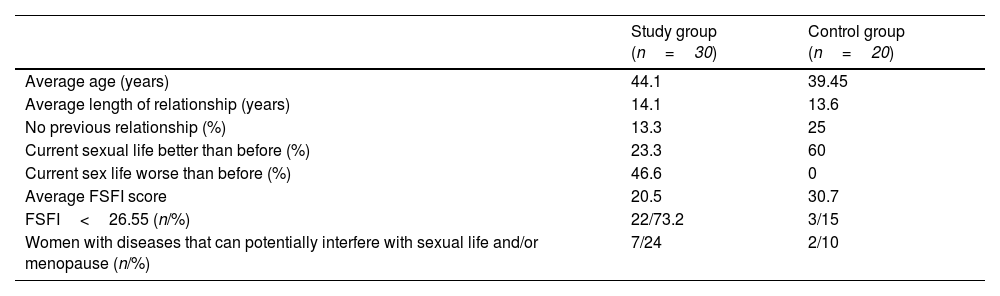
ResultsForty-eight patients who attended the andrology clinic were asked to give their partners the FSFI questionnaire, of these 30 (62.5%) returned it correctly completed (study group). The average age was 44.1 years (26–63 years) and the average duration of the relationship was 14.1 years (1–42 years). Of these 30 women, 14 (46.6%) reported that their current sex life was worse than in previous relationships and 7 (23.3%) that it was better than before. Four (13.3%) women had no previous relationships (Table 1).
Epidemiological data and mean FSFI score of the study group and control group.
| Study group (n=30) | Control group (n=20) | |
|---|---|---|
| Average age (years) | 44.1 | 39.45 |
| Average length of relationship (years) | 14.1 | 13.6 |
| No previous relationship (%) | 13.3 | 25 |
| Current sexual life better than before (%) | 23.3 | 60 |
| Current sex life worse than before (%) | 46.6 | 0 |
| Average FSFI score | 20.5 | 30.7 |
| FSFI<26.55 (n/%) | 22/73.2 | 3/15 |
| Women with diseases that can potentially interfere with sexual life and/or menopause (n/%) | 7/24 | 2/10 |
Regarding the partners of these thirty women who agreed to participate in the study, 21 had complaints of ED, 8 of PE and 1 due to hypoactive sexual desire.
The 20 women who agreed to participate in the study as a control group had a mean age of 39.45 years (28–54 years) and a mean relationship length of 13.6 years (1–29 years). None rated their current sex life worse than before and 5 (25%) said they had no previous relationships. Of these 20 participants, 12 (60%) considered that their current sex life was better than in previous relationships. Both the study and control group groups were statistically homogeneous, regarding age and length of relationships (p>0.05).
Of the 30 women in the study group, 22 (73.3%) had sexual dysfunction (FSFI<26.55), whereas in the control group only 3 women (15%) had sexual dysfunction (FSFI<26.55).
The mean FSFI score (normal<25.66) of the study group was 20.5 (standard deviation: 8.82) and in the control group 30.7 (standard deviation: 4.24). This statistical comparison was performed using a Student's t-test for independent samples and showed a statistically significant difference between the study and control groups (t(48)=−4.689; p<0.001).
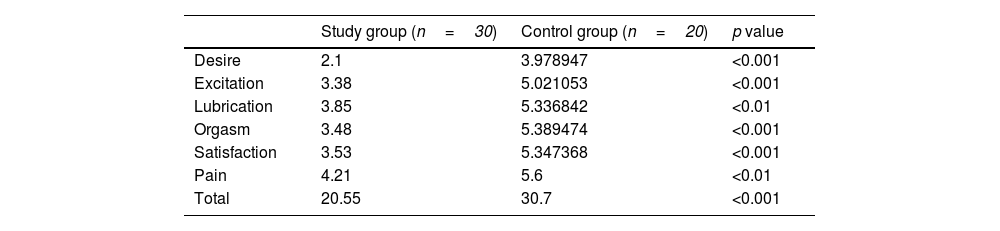
The domains of desire with a score of 2.1 (normal between 1.2 and 6.0), arousal and orgasm with scores of 3.4 and 3.5 respectively (normal between 0 and 6) were the most unfavourable in the study group. The satisfaction domain was equally low with a score of 3.5 (normal between 0 and 6), while the lubrication and dyspareunia domains with a score of 3.8 and 4.2 were the domains that least interfered with female sexual function. It should be noted that in the pain dimension, the highest score means less discomfort or dyspareunia (Table 2).
Mean score for each domain of the FSFI and total score between the study group and the control group.
| Study group (n=30) | Control group (n=20) | p value | |
|---|---|---|---|
| Desire | 2.1 | 3.978947 | <0.001 |
| Excitation | 3.38 | 5.021053 | <0.001 |
| Lubrication | 3.85 | 5.336842 | <0.01 |
| Orgasm | 3.48 | 5.389474 | <0.001 |
| Satisfaction | 3.53 | 5.347368 | <0.001 |
| Pain | 4.21 | 5.6 | <0.01 |
| Total | 20.55 | 30.7 | <0.001 |
Compared to the control group, in each domain, all differences in study group were significant lower: Desire domain (t(48)=−7.918; p<0.001), Arousal domain (t(48)=−3.900; p<0.001), Lubrication domain (t(46.42)=−3.367; p<0.01), Orgasm domain (t(40.77)=−4.709; p<0.001), Satisfaction domain (t(47.13)=−5.486; p<0.001), and in the Pain domain (t(36.36)=−3.369; p<0.01).
The study also showed that seven (24%) of the women assessed in the andrology clinic reported illnesses that could potentially interfere with their sexual function namely diabetes, early menopause or psychiatric pathology. Of these seven women who reported some pathology, 6 had sexual dysfunction (Table 1).
DiscussionFSD affects approximately 40% of women of reproductive age (25–63%) worldwide.1,19 This may result from changes in desire, arousal, orgasm or pain during sexual intercourse and has an important impact on women's well-being and quality of life.1 FSD have a bio-psychosocial aetiology, i.e., they can be caused by organic, psychological and social conditions or be associated with emotional and interpersonal factors.1,20
Several studies have related male sexual dysfunction such as ED, PE and hypoactive male sexual desire, as well as other emotional factors associated with relationship with FSD causing changes in desire, arousal and orgasm.1,20 McCool-Myers et al.1 published in 2018 a meta-analysis in which male partner sexual dysfunction corresponds to an increased risk factor for FSD in virtually all domains, with the exception of pelvic pain. On the other hand, an affectionate and communicative relationship decreases the risk of FSD.1
The multinational FEMALES study (Fisher et al., 2005)4 assessed 293 women and showed a significant decrease in desire, arousal and orgasm after partners developed ED. Similarly, there was an improvement in sexual dysfunction in female partners of patients on phosphodiesterase inhibitors treatment.21
Other studies (E. Maseroli et al.)3 point to the perceived lack of sexual desire or interest from the partner, and not so much ED or PE, as important causes of FSD. In this study, on the male factors associated with FSD, more than 150 heterosexual women with FSD, (with mean Female Sexual Function Index [FSFI] total score of 20.8) reported of having a partner with perceived sexual problem, that is, 33.3% reported a reduction in the partner's sexual desire, 24.4% with ED, and 13.5% with PE, respectively. Only measurements on perception were documented, and no valid instruments were used to validate the male partner's SD.
Our study shows that an important proportion of women (73%), partners of patients attending the andrology clinic present sexual dysfunction (FSFI<25.66). This proportion was statistically significant when compared to the control group (15%) (p<0.001). Although other aspects of the relationship were not analyzed, both groups were homogeneous in relation to age and duration of the relationship, the main difference was the existence of male sexual dysfunction in the study group. In this group there was a significant reduction in desire, arousal and orgasm.
In our study, almost half of the women (46.6%) in the SG classified the current relationship as worse than previous relationships and this may be perceived by the partner. In de CG women classified the relationship as equal (35%) or better (60%) than previous ones. Corona et al. in a study published in 2010 found that men's perception of a moderate or severe decrease in female sexual desire is related to a decrease in the frequency of sexual intercourse, lower self-esteem and ED.22
In a recent published meta-analysis and systematic review, Chew et al. suggest that men partnered with women with FSD is associated with an increased risk of erectile and ejaculatory dysfunction. They found a consistent association between men who were partnered with female with FSD and with a 3-fold increase risk in male sexual dysfunction (MSD). Among subtypes of MSD, the likelihood increased 4-fold for ED and that of PE doubled.23
In ED, besides organic causes, psychogenic and relationship-related causes also contribute, which are not always fully investigated in clinical context. Sexual stimulation is important for sexual functioning in men to activate the dopaminergic–oxytocinnitric–oxide neural pathway and the lack of stimulation may lead to the impairment of this neural pathway leading to ED.24
In the case of FSD it is natural that this partner will feel less committed to participating in the treatment of the sexual dysfunction, whether by supporting the adoption of general measures such as a healthier lifestyle, or more specific measures such as encouraging compliance with the prescribed therapy. They may also feel less motivated to provide sexual stimulation, which is important when we use drugs that requires an initial boost for their efficacy such as phosphodiesterase inhibitors or alprostadil.7
Thus, the dysfunction of one of the elements of the couple may have the effect of originating and/or aggravating eventual sexual dysfunction in the partner. In another independent observation, 2 studies25,26 reported that the female and male sexual functioning, that is, the FSFI and IIEF was correlated (r) at 0.3 and 0.42, among couples in health profession25 and infertile women seeking treatment,26 respectively. This correlation may reflect the importance of understanding the dyad of interrelationship between FSD and MSD and its implications for bio-psycho-social education and intervention.23
This dysfunction involving the couple and their sexual dynamics leads to a cycle of negative, vicious events which damage the relationship as a whole and the sexual relationship in particular.7,11
Men who attended the andrology clinic usually did so alone, often without informing their partners that they had search for assistance in a specialized clinic. Frequently, when partners are asked to attend, the invitation is declined. In fact, of the 48 women invited to participate, 18 (37.5%) refused or were not even informed about the study.
In our sample, 7 women (24%) of the study group had diabetes, menopause and/or psychiatric pathology, diseases that may interfere with their sexual function. Of these 7 women, 6 presented sexual dysfunction (FSFI<25.66). Currently many of the underlying causes of FSD are potentially treatable.
This review has several limitations. First, relatively small sample size, although the difference was statistically significant and indicates a higher prevalence of FSD in partners of patients who attend an andrology clinic. Second the results were derived from patients consulting an andrology clinic, which could have different characteristics from those consulting general practitioners or not seeking medical care for sexual dysfunctions. We used only one questionnaire, the FSFI to assess female sexual dysfunction, and important aspects of the relationship such as communication, intimacy were not assessed. More studies are needed to see if this couple-based approach will improve sexual health outcomes, as hypothesized.
ConclusionsAlthough the definition of ED is the inability of men to initiate or maintain erection, our study showed that this problem can also affect their sexual partners in a significant proportion. Thus, FSD is common in partners of patients who attend the andrology clinic and we must bear in mind that this dysfunction can act as a precipitating factor, maintenance or obstacle to treatment.
Although the mutual interaction and influence in the sexual sphere of a couple is often overlooked during an andrology clinical context, some studies have advocated a more comprehensive approach to sexual dysfunctions, always as a problem of the couple, suggesting an assessment of both the man and the woman.7 These findings support the notion that clinicians should evaluate sexual function in both male and female partners, encompassing several dimensions, and needing an interdisciplinary approach.
In conclusion, FSD is frequent in the context of an andrology clinic and should be seen as a therapeutic opportunity.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.