Suicide is an important Public Health problem. One of the most relevant known risk factors for suicide is suffering from a mental health disorder, identified in up to 90–95% of completed suicides, with this risk being increased if comorbidity is present. Findings from international research on the most common psychiatric disorders are dichotomous, divided into mood disorders and psychotic disorders. In Spain, data of this kind are scarce.
MethodsThis study describes the psychiatric and forensic characteristics of completed suicide cases (n=79) occurred in a psychiatric hospital healthcare area (in Spain), between 2007 and 2010. The forensic data were obtained from the Institute of Legal Medicine of Catalonia and the clinical data by reviewing the clinical records.
ResultsMost of the subjects in this sample were males (78.5%, 95% CI; 68.4–87.3%). Almost half of the sample (45.4%, 95% CI; 33.8–57.1%, 35/77) had records in the Mental Health Services Network (including substance misuse services). Two of the 79 were under 18, so we were not able to access the records. More than half (54.3%, 95% CI; 37.1–71.4%) of those with psychiatric history suffered from a mood disorder; 37.1% (95% CI; 22.9–51.4% from a depressive disorder; 14.3% (95% CI; 2.9–25.7%) from a bipolar disorder, and 17.1% (95% CI; 5.7–31.4%) suffered from a psychotic disorder. With regard to substance misuse, 42.9% (95% CI; 25.7–60.0%) presented substance misuse, and 48.6% did not.
ConclusionsPsychiatric and forensic characteristics of completed suicide in this Spanish sample confirm previous findings from international studies: there is a high rate of psychiatric disorders in those who complete suicide, and there is a specific pattern as regards the method used to complete it.
El suicidio es un importante problema de salud pública. Uno de los principales factores de riesgo conocidos para el suicidio es el padecimiento de patología psiquiátrica que se identifica en un 90–95% de suicidios consumados, incrementándose el riesgo si existe comorbilidad. Los resultados internacionales sobre la patología psiquiátrica más frecuente son dicotómicos, divididos entre los trastornos del humour y los trastornos psicóticos, si bien los datos en nuestro entorno sobre casos de suicidio consumado son muy escasos.
MetodologíaEl presente estudio describe las características psiquiátricas y forenses de los casos de suicidio consumado (n=79) acontecidos en la región asistencial de un hospital psiquiátrico entre 2007 y 2010. Los datos forenses fueron obtenidos en el Instituto de Medicina Legal de Catalunya y los datos clínicos a partir de la revisión de las historias clínicas.
ResultadosLa mayoría de los sujetos fallecidos por suicidio consumado en la muestra de referencia fueron varones (78,5%) (IC 68,4%-87,3%). El 45,5% (IC 33,8%-57,1%) (35 de 77) de los fallecidos disponía de historia en el circuito de salud mental y/o toxicomanías de la zona, desconociéndose los antecedentes de dos de los fallecidos por tratarse de menores de edad. De los 35 individuos con historia en el circuito de salud mental, el 54,3% (IC 37,1%-71,4%) presentaba un trastorno afectivo; (37,1%, IC 22,9%-51,4%) trastorno depresivo; 14,3% (IC 2,9%-25,7%) trastorno bipolar y el 17,1% (IC 5,7%-31,4%) un trastorno del espectro psicótico. Además, el 48,6% presentaba comorbilidad psiquiátrica no relacionada con tóxicos y el 42,9% (IC 25,7%-60,0%) comorbilidad con trastornos relacionados con sustancias.
ConclusionesLas características psiquiátricas y forenses del fenómeno del suicidio consumado en nuestro entorno confirman los datos internacionales sobre una tasa elevada de patología psiquiátrica y un patrón característico en cuanto a metodología suicida.
Suicide is a person's own death caused by oneself with the specific intention of ending one's own life. It is an unnatural death in which the intentionality of the act is determinant.1–5
Suicide is an important public health problem6; the World Health Organisation (WHO) indicates that almost a million people die each year through this cause. The WHO reports a mortality rate of 16 per 100,000, or a death every 40s; in addition, in the last 45 years, suicide rates have risen by 60%.7 Traditionally, suicide occurs more often among elderly men, but the rates in young adult populations have climbed until young people constitute the group at greatest risk in a third of the countries in the world.6
The literature in the field points to different factors of risk for suicide.2,8,9 For example, the suicide rates for men are higher than for women, but suicide attempts that fall short of completed suicide (CS) occur more frequently in women.2 The use of less lethal methods of suicide by females than by males has been reported; however, if the self-destructive attempt is defined as serious, the incidence is similar for men and women.8 Adolescence and old age are considered life stages of special risk.2 Suffering psychiatric pathology or the presence of specific psychological symptomatology is a known risk factor.2
As for the relationship between psychiatric pathology and suicide, in most cases suicide is accepted to be the consequence of psychological suffering. In psychological autopsy studies, the existence of at least 1 psychiatric diagnosis at the time of the suicide is seen in 90–95% of the cases.2,10 Disorders in mood, impulse control, anxiety, and consumption of toxic substances, as well as psychotic and personality disorders are all associated with an elevated risk of suicide and suicidal behaviours.2 Comorbidity is associated with an especially high risk of suicide,2 while the psychiatric pathology most often found in cases of CS can be divided into 2 major groups: affective disorders11 and schizophrenia, the latter in samples mainly composed of hospitalised patients or those in peri-admission circumstances.12–14 Patients with an affective disorder have a lifetime mortality rate from suicide that hovers around 15%, with variations that range from 5% to 26% according to the study population; the characteristics of the pathology, as well as its severity and chronicity, are determining factors. Schizophrenia is also associated with an elevated risk of suicide and the standard mortality rate per suicide range between 15.715 and 39.7.16 The percent of subjects with schizophrenia diagnoses that commit suicide during their lifetime also varies notably, from 4.9%17 to 9.7%, according to several studies.18
Apart from the disorder the patient has, there are specific symptoms that can be common to different disorders; these symptoms, as they increase the level of emotional distress, can increase the risk of suicide.
Factors that may protect against suicide include religious beliefs, spirituality, moral objections to suicide and specific environmental elements such as a social network that provides appropriate support. All these factors of risk or of protection require detailed study in assessing suicidal behaviour, given that some of them can have a conditioned action.2
Likewise, some studies have reviewed aspects related to the help that victims of suicide receive. In the period prior to the suicide, contacts with primary care are frequent. Three out of every 4 victims contact primary care during the year before the suicide and approximately a third have contact with mental health services (MHS); 45% contact primary care during the month before and a fifth contact MHS, with the primary care contact rates being higher in older subjects than in young adults, and in females than in males.19
Lastly, the method of suicide refers to the mechanism used to produce death. According to mortality statistics, hanging, strangulation or suffocation (CIE-10 code X70) were the methods most used in suicide deaths in Spain in 2010, followed by falls from heights and posioning.20 In schizophrenia, a greater tendency to use clearly lethal methods in suicide has been described and a history of previous attempts with highly-lethal methods is considered to multiply the risk of completing the suicide by 11.16,21
There are numerous studies on the relationship between suicide and mental pathology with consistent findings at the international level.2
Our study attempts to describe and analyse sociodemographic, clinical and forensic variables associated with the phenomenon of CS in our setting. This information could guide the preparation of preventative and therapeutic measures aimed at approaching suicide adjusted to possible differential cultural or sociodemographic factors.
Material and methodThe sample was taken from all the deaths in the municipalities of Santa Coloma of Gramenet, Badalona and Sant Adrià del Besòs (Spain) during the 2007–2010 period whose medical-legal aetiology was considered suicide after the medical-legal autopsy. The data were obtained from the Institute of Legal Medicine of Catalonia. The estimated total population of the area is 373,050 inhabitants.22 Sample identification was carried out retrospectively by the analysis of the forensic sources. Afterwards, the clinical variables were recorded by revising the clinical histories registered in a database of the MHS centres in the study area (the adult MHS centres, the centre for care and follow-up of drug abuse and the psychiatric hospital of the public health area). Access to the network of primary care that carries out follow-up on mild psychiatric disorders was unavailable. Apart from the clinical variables extracted directly from each subject's clinical history, the researchers added the variable of treatment adherence, reached by consensus upon analysing the subjects’ clinical histories, assessed as adequate, partial or deficient.
The research received the approval of the ethics committee of the hospital of reference in the area of the sample. Statistical analysis was performed using the SPSS version 20.0 statistical package. Descriptive and analytical analyses were performed, using Pearson Chi-square and Mann Whitney U statistical tests.
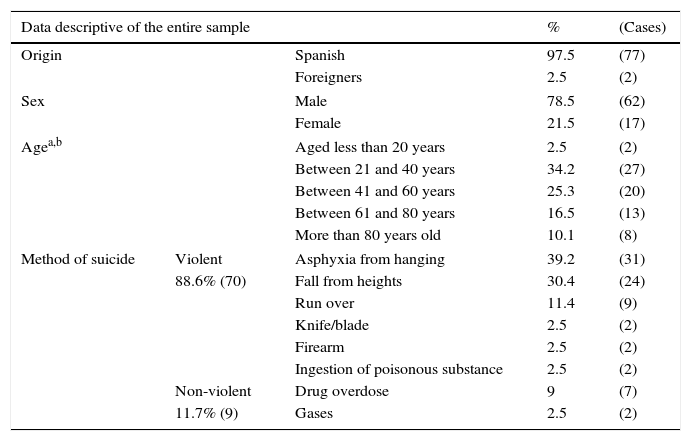
ResultsDuring the period under study, 79 cases of completed suicide were identified. This represents an accumulated incidence of suicide in this population of 21.18/100,000 inhabitants in 4 years (from 2007 to 2010), with a mean incidence of 5.29 suicides per 100,000 inhabitants per year. Table 1 presents the characteristics of the total sample of deaths by CS in the study period. In the sample, 88.6% (confidence interval [CI] 81.0–94.9%) used a violent suicide method (which, in our study, included asphyxiation by hanging, falls from heights, being run over by train, stab wounds, firearm wounds and ingesting caustic substances). The method most often used was asphyxiation by hanging (39.2%, CI 27.8–49.4%), followed by falls from heights (30.4%, CI 21.5–40.5%) and being run over by train (11.4%, CI 5.1–19.0%).
Characteristics of the entire sample of subjects deceased through consummated suicide.
| Data descriptive of the entire sample | % | (Cases) | ||
|---|---|---|---|---|
| Origin | Spanish | 97.5 | (77) | |
| Foreigners | 2.5 | (2) | ||
| Sex | Male | 78.5 | (62) | |
| Female | 21.5 | (17) | ||
| Agea,b | Aged less than 20 years | 2.5 | (2) | |
| Between 21 and 40 years | 34.2 | (27) | ||
| Between 41 and 60 years | 25.3 | (20) | ||
| Between 61 and 80 years | 16.5 | (13) | ||
| More than 80 years old | 10.1 | (8) | ||
| Method of suicide | Violent | Asphyxia from hanging | 39.2 | (31) |
| 88.6% (70) | Fall from heights | 30.4 | (24) | |
| Run over | 11.4 | (9) | ||
| Knife/blade | 2.5 | (2) | ||
| Firearm | 2.5 | (2) | ||
| Ingestion of poisonous substance | 2.5 | (2) | ||
| Non-violent | Drug overdose | 9 | (7) | |
| 11.7% (9) | Gases | 2.5 | (2) | |
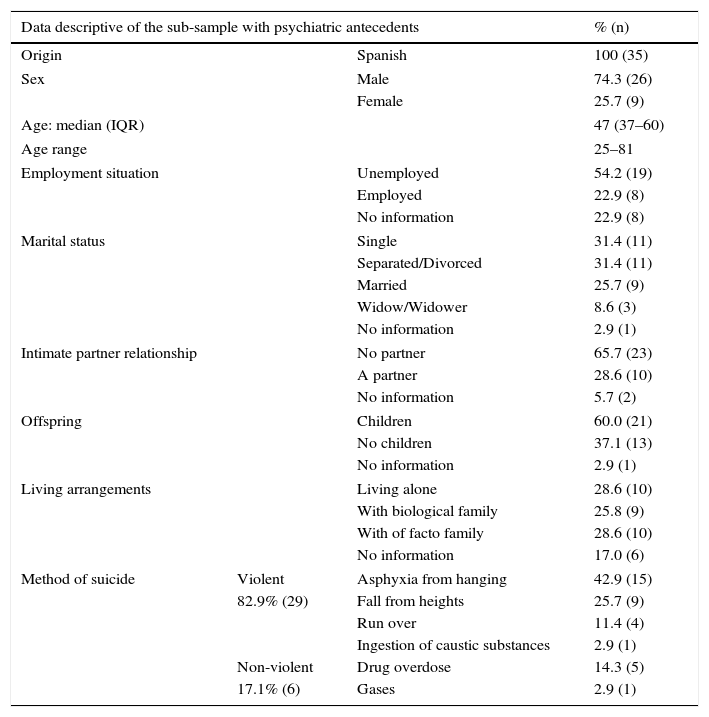
Two of the 79 subjects who died were minors and data on their possible psychiatric antecedents were unavailable due to lack of access to the child-adolescent MHS network. Of the remaining 77 subjects, antecedents were identified in the MHS network for adults in 35 cases (45.4%) (CI 33.8–57.1%). There had been a diagnosis of a psychiatric disorder in 26.0% (CI 15.6–36.4%) of the cases and in 19.5% (CI 11.7–28.6%) there was comorbidity with disorders related with substance abuse. Table 2 shows the characteristics of the subgroup of subjects having psychiatric antecedents.
Characteristics of the sub-sample of deceased subjects with psychiatric antecedents.
| Data descriptive of the sub-sample with psychiatric antecedents | % (n) | ||
|---|---|---|---|
| Origin | Spanish | 100 (35) | |
| Sex | Male | 74.3 (26) | |
| Female | 25.7 (9) | ||
| Age: median (IQR) | 47 (37–60) | ||
| Age range | 25–81 | ||
| Employment situation | Unemployed | 54.2 (19) | |
| Employed | 22.9 (8) | ||
| No information | 22.9 (8) | ||
| Marital status | Single | 31.4 (11) | |
| Separated/Divorced | 31.4 (11) | ||
| Married | 25.7 (9) | ||
| Widow/Widower | 8.6 (3) | ||
| No information | 2.9 (1) | ||
| Intimate partner relationship | No partner | 65.7 (23) | |
| A partner | 28.6 (10) | ||
| No information | 5.7 (2) | ||
| Offspring | Children | 60.0 (21) | |
| No children | 37.1 (13) | ||
| No information | 2.9 (1) | ||
| Living arrangements | Living alone | 28.6 (10) | |
| With biological family | 25.8 (9) | ||
| With of facto family | 28.6 (10) | ||
| No information | 17.0 (6) | ||
| Method of suicide | Violent | Asphyxia from hanging | 42.9 (15) |
| 82.9% (29) | Fall from heights | 25.7 (9) | |
| Run over | 11.4 (4) | ||
| Ingestion of caustic substances | 2.9 (1) | ||
| Non-violent | Drug overdose | 14.3 (5) | |
| 17.1% (6) | Gases | 2.9 (1) | |
IQR: Interquartile range.
In the analysis of the psychiatric antecedents, the 2 subjects aged less than 18 years that died from CS during the study period were excluded, given that their psychiatric antecedents were unknown because there was no access available to the child–adolescent mental health network.
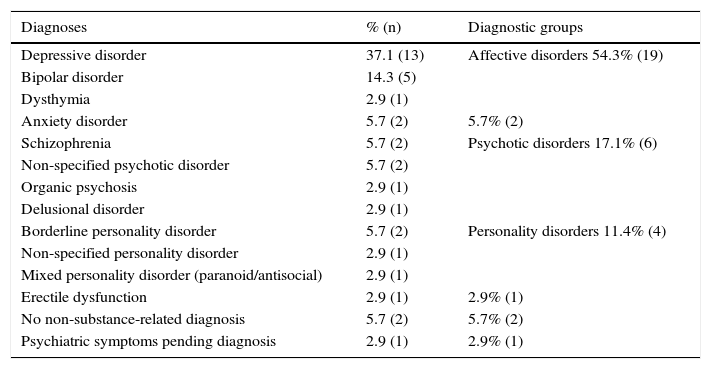
In the group with antecedents registered in their clinical histories in adult MHS, the majority had affective disorders (54.3%, CI 37.1–71.4%) and disorders on the psychotic spectrum (17.1%, CI 5.7–31.4%), as can be seen in Table 3.
Diagnoses of the subsample of subjects with psychiatric antecedents.
| Diagnoses | % (n) | Diagnostic groups |
|---|---|---|
| Depressive disorder | 37.1 (13) | Affective disorders 54.3% (19) |
| Bipolar disorder | 14.3 (5) | |
| Dysthymia | 2.9 (1) | |
| Anxiety disorder | 5.7 (2) | 5.7% (2) |
| Schizophrenia | 5.7 (2) | Psychotic disorders 17.1% (6) |
| Non-specified psychotic disorder | 5.7 (2) | |
| Organic psychosis | 2.9 (1) | |
| Delusional disorder | 2.9 (1) | |
| Borderline personality disorder | 5.7 (2) | Personality disorders 11.4% (4) |
| Non-specified personality disorder | 2.9 (1) | |
| Mixed personality disorder (paranoid/antisocial) | 2.9 (1) | |
| Erectile dysfunction | 2.9 (1) | 2.9% (1) |
| No non-substance-related diagnosis | 5.7 (2) | 5.7% (2) |
| Psychiatric symptoms pending diagnosis | 2.9 (1) | 2.9% (1) |
The mental health pathology had evolved over more than 20 years in 25.7% (CI 11.4–40.0%) of the cases, while the psychopathological evolution was of 11–20 years in 28.6% (CI 14.3–42.9%) of the cases. In 14.3% (CI 2.9–25.7%) of the cases, the evolution was between 6 and 10 years and in 17.1% (CI 5.7–31.4%), it was 5 years or less. The period of disease evolution was unknown in 14.3% (CI 5.7–25.7) of the cases.
Of the subjects that died with psychiatric antecedents, 48.6% presented psychiatric comorbidity unrelated with substances, while 42.9% (CI 25.7–60.0%) had substance-related comorbidity. The substance found most involved in substance-related disorders was alcohol (86.7%, CI 66.7–100.0%; 13/15), which was present in all the cases of multiple drug use (46.7%, CI 23.1–75%; 7 out of 15). The following substance most consumed was cocaine (33.3%, CI 11.1–58.3%, 5 subjects); 1 subject consumed only this substance, 3 subjects consumed cocaine together with alcohol and 1 other subject consumed it concomitantly with alcohol and cannabis.
Treatment with drugs was being given to 80% (CI 65.7–91.4%) of the cases of completed suicide. Treatment adherence was considered adequate in 46.4% (CI 28.6–65.5%) of the drug treatment cases, partial in 39.3% (CI 21.4–57.7%) and deficient in 10.7% (CI 0.0–23.3%) of the cases (no information was available for 1 of the subjects).
As for hospitalisation, 42.9% (CI 28.6–60.0%) of the subjects had never been admitted to the centre of reference hospital, 22.9% (CI 8.6–37.1%) had been admitted only once, 14.3% (CI 2.9–25.7%) twice and 17.1% (CI 5.7–31.4%) on 3 or more occasions (the maximum was 22 admissions). Two subjects died while hospitalised in the installations of the centre itself (5.7%, CI 0.0–14.3%, of the sample with mental health history).
With respect to the last health care received, the last visit to a place in the network of MHS or area substance-abuse centres had been over 8 months previously in 65.7% (CI 48.6–80.0%) of the cases. It had been between 3 and 5 months previously for 2 subjects (5.7%. CI 0.0–14.3%), between 1 and 3 months for 3 subjects (8.6%, CI 0.0–20%), between 16–30 days for 2 subjects (5.7%, CI 0.0–14.3%) and a period of less than 15 days for 5 of the subjects (14.3%, CI 2.9–25.7%).
In 48.6% (CI 31.4–65.7%) of the cases (17 subjects), the clinical history indicated an antecedent of prior self-destructive attempts. According to these records, a single prior suicide attempt had been made by 22.9% (CI 8.6–37.1%) of the subjects (8 cases); the records indicated that 17.1% (CI 5.7–31.4%) (6 subjects) had made 2–3 prior attempts, while 8.6% (CI 0.00–17.1%) (3 subjects) had made 4 or more attempts (maximum of 6).
Of the subsample having mental health antecedents, 82.9% (CI 71.4–94.3%) used a violent suicide method. The method most used was asphyxia by hanging (42.9%, CI 25.7–60.0%), followed by a fall from heights (25.7%, CI 11.4–42.8%), drug overdose (14.3%, CI 2.9–25.7%) and being run over by train (11.4%, CI 2.9–22.9%).
The men and women that died from CS in the sample studied showed no statistically significant difference with respect to age at death (U=361, P=.589). The median age of deceased females was 40.00 years (interquartile range [IQR] 37–65), while that of the males was 50 (IQR 39–60). Likewise, there was no statistically significant association found between sex and the general methodology of suicide (X2=1, 0.750; P=.386).
As for any association between age and previous registered psychiatric pathology, we found no statistically significant differences in age at death between subjects with a mental health history (median=47, IQR=37–60) and subjects lacking MHS history (median=54, IQR=38.5–75) (U=452.5, P=.125).
With respect to the subsample of subjects having a history in the MHS and substance abuse circuits, there were no statistically significant differences by sex for the level of education (X2=1, 0.27; P=.602), type of psychiatric disorder (X213=16, 637; P=.216), toxic-substance related disorders (X29=9, 15; P=.423), number of psychiatric hospitalisations (U=98, P=.797), suicidal attempts prior to the CS (U=57, P=.070) or length of the course of the main diagnosis (U=56, P=.406).
Marital status at the time of CS was significantly associated with sex (X23=10, 75; P=.013). Two women were single, while 9 men were single; there were no divorced or separated women, while this was the most predominant category of marital status among the men (n=11). Five women were married or had a stable partner, compared with 4 men; there were 2 widowers and 1 widow.
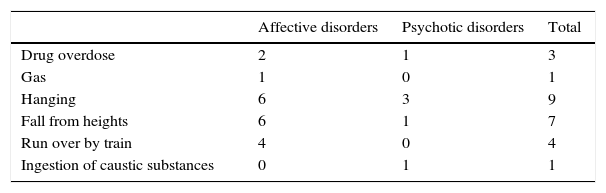
No statistically significant association was found between the type of psychiatric diagnosis and the specific CS methodology (X265=67, 29; P>.05). Likewise, there were no differences in the use of a more violent method for completing the suicide between the subjects having a diagnosis of an affective or a psychotic disorder (X22=0, 934; P=.627). Table 4 shows the frequencies grouped by the 2 most relevant diagnostic spectra.
DiscussionThere are several recent studies that examine relevant aspects in suicide in our setting.23,24 However, to the best of our knowledge, this is the first study in our setting to analyse the clinical and forensic characteristics of all the patients deceased through suicide during a 4-year period of time. The interrelation of the 2 types of variables (clinical and forensic) achieves a comprehensive approximation to the phenomenon of suicide. The analysis presented is possible that to the collaboration between institutions for health care and those of the legal-medical setting (Legal Medicine Institutes25), with the latter being the only sources with access to real data on CS in our setting.26
The suicide rates in the area studied (5 suicides per 100,000 inhabitants) are lower than the 16 suicides per 100,000 inhabitants given by the WHO.6 However, they come close to those provided by the National Institute of Statistics, which were 6.5 suicides/100,000 in 2008.22 These figures confirm that the fact that suicide seldom occurs conditions sample sizes in all studies, including this one.
The analysis of the sociodemographic data confirmed the descriptive findings repeatedly reflected in the literature: a predominance of males among the deceased2 (78.5% [CI 68.4–87.3%] in our sample) and an important percent of elderly subjects2 (26.6% [CI 16.5–35.4%] of our sample were more than 60 years old). The literature indicates contradictory data on the universality of the distribution of these variables, although our study would confirm it. Specific sociodemographic variables could only be studied for the subgroup of subjects having antecedents in the MHS network, which limits the conclusions in this sense. Worthy of special mention is the fact that, with respect to the marital status of the subjects with MHS history, we found statistically significant differences between men and women; women had a better partner situation (more married subjects, none separated or divorced, fewer single subjects and more widows). This could correlate with women having a later onset or a less aggressive progression in specific pathologies than men.
The percentage identified in our sample of subjects with diagnosed mental pathology in the MHS network was noticeably lower than that presented in other publications (45.5% [CI 33.8–57.1%] in our sample vs 95% in Nock et al.2). This strong difference could be related to mainly the impossibility of accessing the data of patients affected by mental pathology that are followed up in primary care or the private circuit. This barrier to information access is often reproduced in clinical health care. Consequently, improvements in this sense would bring about improvements in patient care. In any case, we feel that this study gathers the majority of the subjects having serious mental disorders, with the rest perhaps corresponding to mild, recent-onset or still undetected pathology.
Our findings corroborate most of the clinical data known to date, which indicate the high risk of suicide in males affected by affective and psychotic disorders. Given that this is a retrospective study, factors of risk cannot be established. However, the study data indicate the affective disorders were the pathology most often diagnosed in the sample, in agreement with the authors that point out a predominance of this type of pathology in non-hospitalised patients11 (the majority in the study). In more than half of the cases, the disease progression was above 10 years.
In this study, 88.6% (CI 81.0–94.9%) of the subjects used a violent method in the suicidal behaviour studied. This finding was to a certain degree expected, as violent methodology is deadlier, which is a determining factor in a study on CS. It is also this feature of the study design itself that prevents us from establishing conclusions about the males’ use of more violent methods described in the literature.8 The reason is that those that in fact died probably correspond to the ones that used more lethal methods and the total number of subjects that carried out suicidal behaviour is unknown. Likewise, we found no statistically significant differences in the use of a more violent method to consummate suicide according to whether subjects diagnosed with affective or psychotic disorders were involved. These results differ from previous studies in that suicide by violent acts was more frequent in subjects with diagnosed psychotic disorders (the method most used by this subgroup of patients was falls from heights).16 However, this should be considered in the context of a subsample of analysis of limited size.
ConclusionsSuicides happen rarely and are consequently complex to study, in addition to being hard to prevent and stop. In over half of the deaths (54.5%, CI 42.9–64.9%; 42/77) in our sample, there was no record of contact with the MHS network in the area. Consequently, we emphasise the need to boost the efforts to detect cases of subject at risk of suicide and to refer them to the MHS circuit. However, even though contact with the specialised network of MHS is considered a factor of protection against suicide, it cannot by itself protect all the patients from dying by SC. In the sample studied, 2 of the subjects died in the installations of the health care institution itself and 20.0% (CI 8.6–34.3%) had visited the MHS network within the previous 30 days. Consequently, it is felt that detailed protocols should be developed to gather all the suicide-associated factors of risk.27 These known factors of risk are not found in all the cases (e.g., 51.4% [CI 37.1–68.6%] of the subjects in our sample committed suicide without any known prior suicide attempts), which undeniably complicates the task of prevention.
At present, mental health problems continue increasing. During the last several years (2006–2010), Spain has experienced a considerable growth in the number of primary care visits because psychological distress, associated with the negative personal consequences involved in the economic crisis.28 It is relevant to evaluate the risk of suicide that might exist in these cases to make preventing it possible, in agreement with the results obtained, that highlight the fact that 54.5% (CI 42.9–64.9%; 42/77) of the CS cases had never contacted the MHS network (considering only the adults).
Studies like this one help to describe the phenomenon of suicide in our setting, providing data needed to prevent this type of violent death. In this respect, we consider relevant the variables present in the CS deaths in our sample such as sex (male), unemployment, marital status (single, divorced or separated), the lack of an intimate partner relationship and the existence of psychiatric antecedents, especially depressive disorder. Finally, it should be remembered that increasing research efforts on this serious public health problem is needed; likewise, the coordination of all the resources of the health care and forensic network have to be improved to attempt to lower the suicide rates of our population.29,30
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments on human beings or animals have been carried out in this investigation.
Data protectionThe authors declare that they have followed their work centre's protocols on the publication of patient data and that all the patients included in the study have received sufficient information and have given their written informed consent to participate in this study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflicts of interest to declare.
We are grateful to the centres previously known as the Emili Mira i López Health Care Centres (currently part of the Parc of Salut Mar Neuropsychiatric and Addiction Institute), to the Mental Health Centres Badalona 1 & 2 in Badalona and Martí i Julià in Santa Coloma de Gramanet, to the Delta Centre for Care and Follow-up in Drug Addictions and to the professionals that made this study possible.
We would also like to thank the Institute of Legal Medicine of Catalonia, especially the Forensic Pathology Centre in northern Barcelona (Collserola).
Please cite this article as: Gómez-Durán EL, Forti-Buratti MA, Gutiérrez-López B, Belmonte-Ibáñez A, Martin-Fumadó C. Trastornos psiquiátricos en los casos de suicidio consumado en un área hospitalaria entre 2007–2010. Rev Psiquiatr Salud Ment (Barc.). 2016;9:31–38.