Each region should know which its predominant allergens are. However, in addition to the differences that exist between different geographical areas, variations within the same area should be determined.
ObjectivesTo review the predominant allergens in the paediatric population suffering from asthma or rhinitis in our region and analyse the internal variations and associated factors.
MethodsA cross-sectional, descriptive study reviewing all the patients having a diagnosis of asthma or rhinitis in the paediatric allergy units of three hospitals in a coastal region in the south-east of Spain between 2001 and 2006.
ResultsData on 3066 patients, 2202 (72 %) of whom were atopic, were collected. Atopy was present in 63 % of asthmatics, 90 % of those with rhinitis and 95 % of those with both asthma and rhinitis. The percentage of atopic patients increased with age. Egg was the main allergen in the first 3 years of life, followed by milk. Aeroallergen sensitization started in the second year of life and increased rapidly in subsequent years. The main aeroallergens in our region, in descending order, were: olive, mites, Salsola, Alternaria, cat, dog and grasses. With the five main aeroallergens, 98 % of atopic patients between 6 and 14 years of age, and 94 % of those between 3 and 5 years of age are detected. In children under the age of three it is necessary to combine food and aeroallergens in order to detect most of the atopic patients. Sensitization to Alternaria occurred at an early age but stabilized before that caused by other aeroallergens. Sensitization to mites was very high along the coastline (83 %) but at only 5-30 km inland it decreased by half. On the other hand, sensitization to pollen and Alternaria increased sharply as we move away from the coast.
ConclusionsWe have described the main allergens in children with asthma and rhinitis in a Mediterranean region in Spain, and have found marked differences depending on age and proximity to the coast. The local importance of Salsola, the early sensitization to Alternaria, and the surprisingly short reach of the influence of the coast in favouring sensitization to mites and protecting from sensitization to pollens and Alternaria are noteworthy.
Chronic rhinitis and asthma are a frequent problem in children throughout the world, as shown by the ISAAC study.1 The main recognised risk factor for both diseases is atopy, which is particularly associated with the severity and persistence of symptoms. In addition to the variability of asthma, rhinitis and atopy in the various geographical areas2 due to socio-cultural and bioclimatic differences, the child's age and growth also have an effect. This results in marked variations between different areas and even within the same area or depending on the patient's age. The studies performed have repeatedly emphasised the need to analyse the epidemiology of these diseases and the allergens involved at the local level.
Our group works with a very homogeneous system in three hospitals in the south-east of the Alicante province (Valencian Community, Spain). The majority of the paediatric population with allergy and respiratory diseases in this region attend our clinical settings, since the number of patients attending non-state subsidised doctors' settings exclusively is a minimum. Therefore, we may assume that the patients treated in our hospitals, most of whom have been referred by their general practitioners or paediatricians, account for a significant percentage of all patients suffering from asthma or rhinitis in our region, and the majority of those with non-mild disease. For this reason, we consider it interesting to collect the information obtained during clinical practice in recent years so as to analyse the factors associated with the allergenic profile of asthma and rhinitis in children in our region.
MATERIAL AND METHODSStudy designThis is a cross-sectional, descriptive study reviewing the clinical records of patients attending the paediatric allergy units in the Elche, Elda and Orihuela hospitals of the Valencian Health Agency, which provides public healthcare in the Valencian Community.
Geographical characteristicsThe region covered in the study lies along the south-east coast of Spain and occupies an area of 2890km2. It is very densely populated (838,540 inhabitants on the December 2006 population database, including 135,849 under the age of 15) with both urban and rural nuclei. It has a Mediterranean semi-arid climate, although there is a certain gradation between the coastal plain, strongly influenced by the proximity of the sea, and the mountainous inland, where the climate tends to be somewhat more continental. Therefore, from a geographical point of view, the region has been divided into three zones with mildly different bioclimatic characteristics:
- –
Zone 1: the coastline, including towns and villages less than 5km from the seaside and at an altitude of less than 50m.
- –
Zone 2: further inland, towns and villages in the coastal plain between 5 and 30 kms from the seaside at an altitude of 50–150m.
- –
Zone 3: further inland, towns and villages between 20 and 50km from the seaside at an altitude of 200 to 700m, in the valleys of the mountain ranges in the north of the province of Alicante.
Patients under the age of 15, attending hospital for the first time between January 2001 and December 2006 and diagnosed as having rhinitis (allergic or non-allergic, not due to infection or secondary to other diseases) or asthma (recurrent bronchitis or wheezing not secondary to other diseases) were included in the study. Patients were interviewed by one of the authors, who decided in each case which allergologic study should be performed. In schoolage children, it generally consisted of a battery of skin tests with more than 20 aeroallergens prevalent in our region. In younger children, tests were usually performed with a selection of airborne and food allergens. The doctor in charge of the patient might order new studies (skin tests or quantification of specific IgE in serum) if he considered them advisable, with clinical orientation. Skin tests were performed by expert nursing staff dedicated to this task during the whole of the study period.
Data collection methodThe data obtained during the patient's first evaluation, usually recorded in the first clinical report, was reviewed. It included all the information collected during the first and immediately subsequent visits, when the data necessary to make a diagnosis and determine the long term treatment were obtained. Information obtained in later visits to verify the patient's progress, usually 6 or more months after the first visit, was not included.
Data recordingA form created with Microsoft Access was filled in for each patient. It included the patient's age (in years), sex, diagnosis, hospital attended, and details on the allergens to which there was sensitization (from positive skin tests or specific IgE in serum above 0.35 kU/L).
Treatment of dataThe data collected were reviewed to avoid duplications as well as any controversial or impossible results, thus eliminating any possible errors that might have been committed during the recording stage. Statistical analysis was done using the programme Epi Info version 3.3.2. The chi-square test was used for comparison of proportions. The 95% confidence intervals (CI) of certain percentages were calculated.
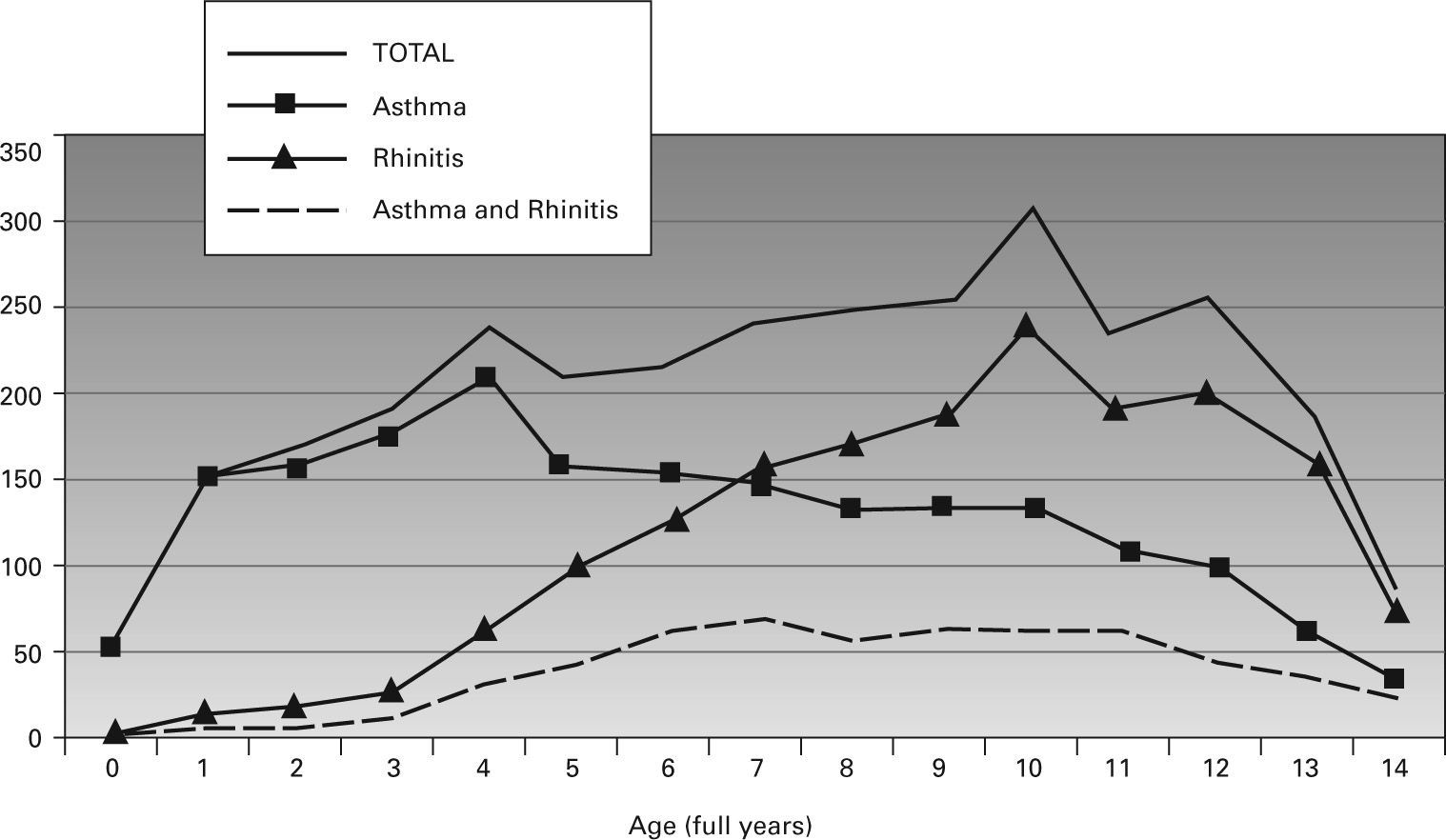
RESULTSInformation on 3066 patients (1855 boys and 1211 girls, ratio 3:2) who fulfilled the criteria for inclusion was collected. Of them, 1935 (63 %) had asthma and 1709 rhinitis (56 %); 578 (19 %) had both asthma and rhinitis simultaneously. Figure 1 shows the number of patients by diagnosis and age.
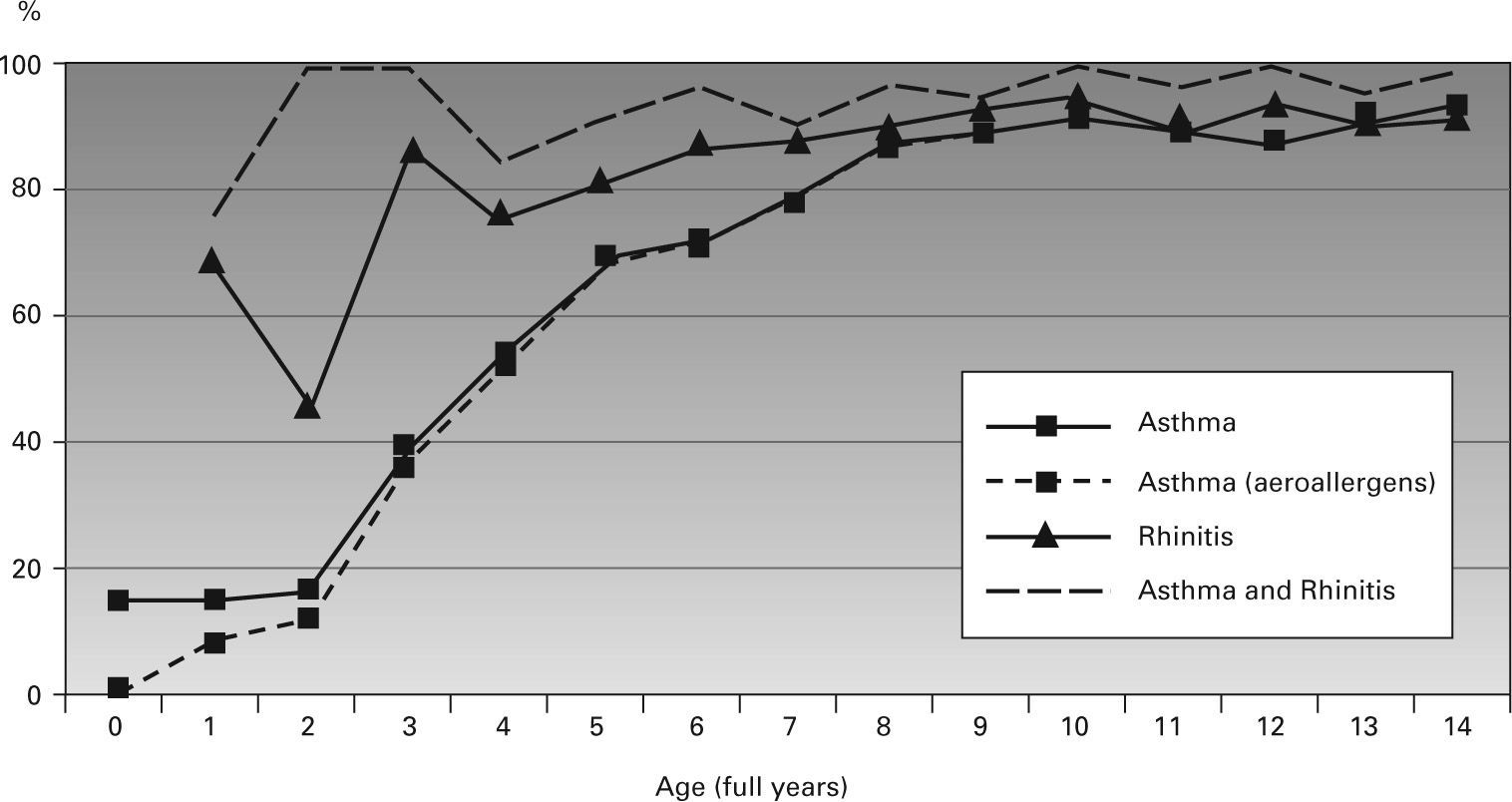
Two thousand two hundred and two patients (72 %) were sensitized to at least one allergen (they may therefore be considered atopic), including 63% of asthmatic patients, 90 % of those with rhinitis and 95 % of those with both asthma and rhinitis. Figure 2 shows the proportion of atopic children by diagnosis and age.
Percentage of atopic patients according to diagnosis by age (in full years). In asthmatic patients, the percentage of patients sensitized to aeroallergens only is shown so as to underline the importance of sensitization to foods in the first years of life. The line corresponding to the percentage of atopic patients in the total study population is not included since it coincides closely over that of the asthmatic patients.
The main aeroallergens and food allergen are shown in the tabla I. In total, 2136 children were sensitized to one of the seven main allergens (97 % of all those sensitized) and 2120 to one of the 5 main allergens (olive, mites, Salsola, Alternaria and cat; 96 % of all those sensitized). Other aeroallergens responsible for sensitization in our region were (in descending order) Artemisia pollen, rabbit and horse epithelium, Parietaria and Mercurialis pollen, Cladosporium and palm pollen. Each of them accounted for less than 10 % of all atopic patients.
Main aeroallergens causing sensitization in the population studied. Egg is added to this list
| Allergen | N (% of atopic patients) | Mean age of N | Monosensitized (% monosensitized/N) | Mean age of monosensitized |
| Olive pollen | 1,149 (52%) | 9.8years | 45 (4 %) | 7.8years |
| Mites | 977 (44 %) | 9.5years | 277 (28 %) | 8.5years |
| Salsola pollen | 974 (44 %) | 9.9years | 66 (7 %) | 9.3years |
| Alternaria | 731 (33%) | 8.8years | 121 (17%) | 7.3years |
| Cat epithelium | 663 (30 %) | 9.8years | 19 (3%) | 6.4years |
| Dog epithelium | 443 (20 %) | 9.6years | 8 (2 %) | 6.1years |
| Grass pollen | 432 (20 %) | 10.5years | 4 (1 %) | 12.0years |
| Egg | 76 (3 %) | 4.0years | 19 (25%) | 1.4years |
One hundred and seventy children were sensitized to food allergens (8 %); 144 of these (85 %) were sensitized to one of the following: egg (76), peach (50), peanut (32) or milk (27). Forty two children were sensitized to food allergens only (2 % of all those sensitized).
Two thousand one hundred and eighty one children were sensitized to one of the 7 main aeroallergens or 4 main food allergens (99 % of all those sensitized). Five hundred and eighty one children were monosensitized (19 % of the sample and 26 % of the atopic patients). Five children were sensitized to latex (one was monosensitized).
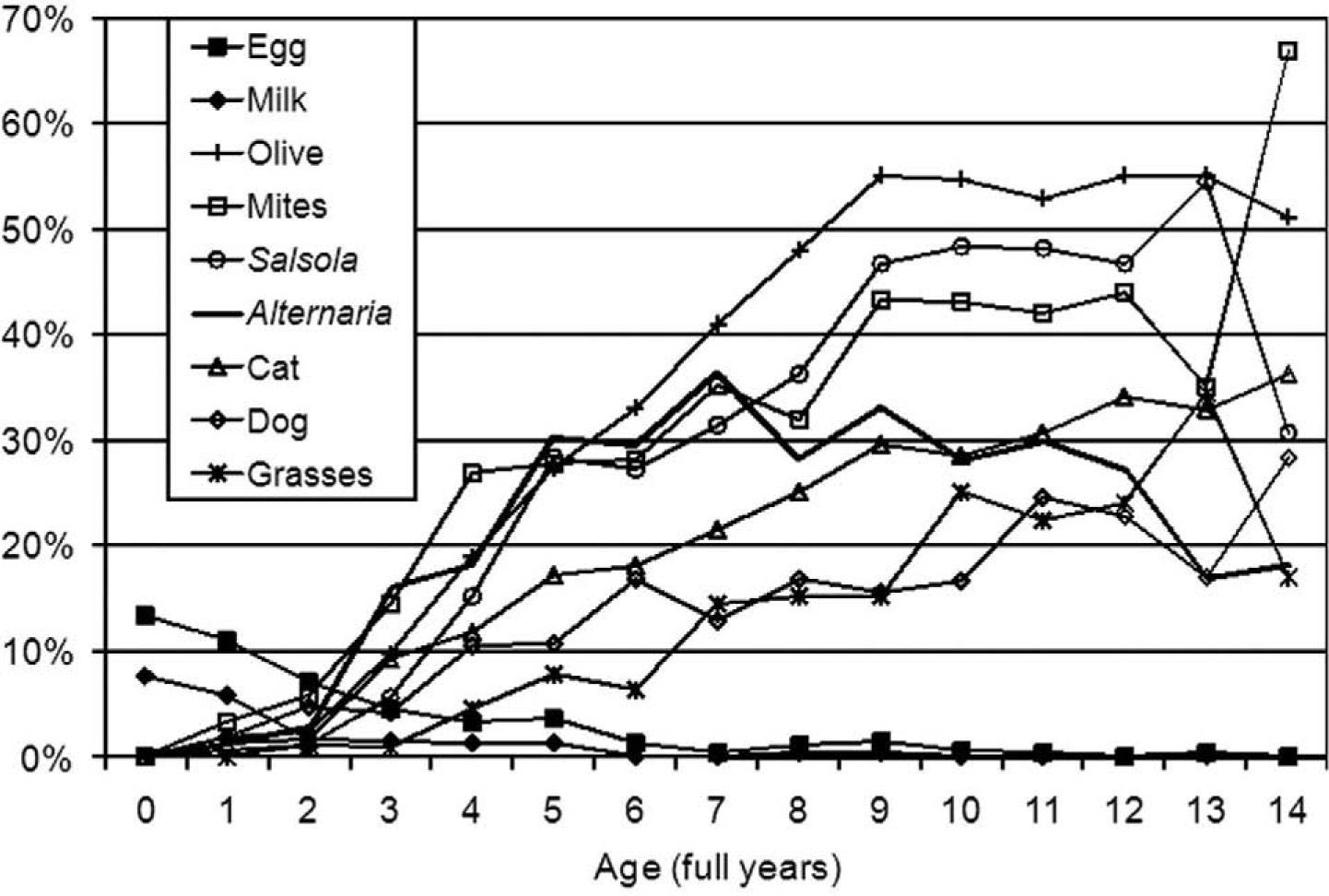
Figure 3 shows the percentage of children sensitized to the main allergens by age. The aeroallergens not represented in this figure followed a similar pattern of increasing prevalence with the patient's age, although this was less marked than in the aeroallergens shown. Other food allergens (peach and peanut) reached a discrete maximum between the ages of 2 and 6years but persisted at a low level in older children. By age group, the combinations of allergens that enabled the greatest number of atopic patients to be recognised were the following:
- –
6 to 14years: 87% were atopic, 98.4% of whom (CI: 97.7 %-98.9 %) were sensitized to one of the 5 main allergens (olive, Salsola, mites, Alternaria and cat).
- –
3 to 5years: 56 % were atopic, 93.9% of whom (CI: 90.8 %-96.1 %) were sensitized to one of the 5 mentioned allergens. When peach was included, the percentage rose to 95.9 % (CI: 93.1 %-97.6 %). Adding dog or egg, it rose to 97.2 % (CI: 94.8 %-98.6 %) and adding both dog and egg, to 98.3 % (CI: 96.2 %-99.3 %).
- –
0 to 2years: 16 % were atopic. With the 5 main aeroallergens between the ages of 3 and 14, only 47.5 % of atopic patients under the age of 3 were detected, whereas with egg alone 59 % of these atopic infants were detected. At this age, the best combination to detect atopy is: egg, milk, mites, Alternaria, dog and olive. This combination detected 95.1% of the atopic patients (CI: 86.3 %-99.0 %). In order to detect 100 % of these 61 children (CI: 94.1%-100%) at least three more allergens (cat, peach and peanut) would need to be included.
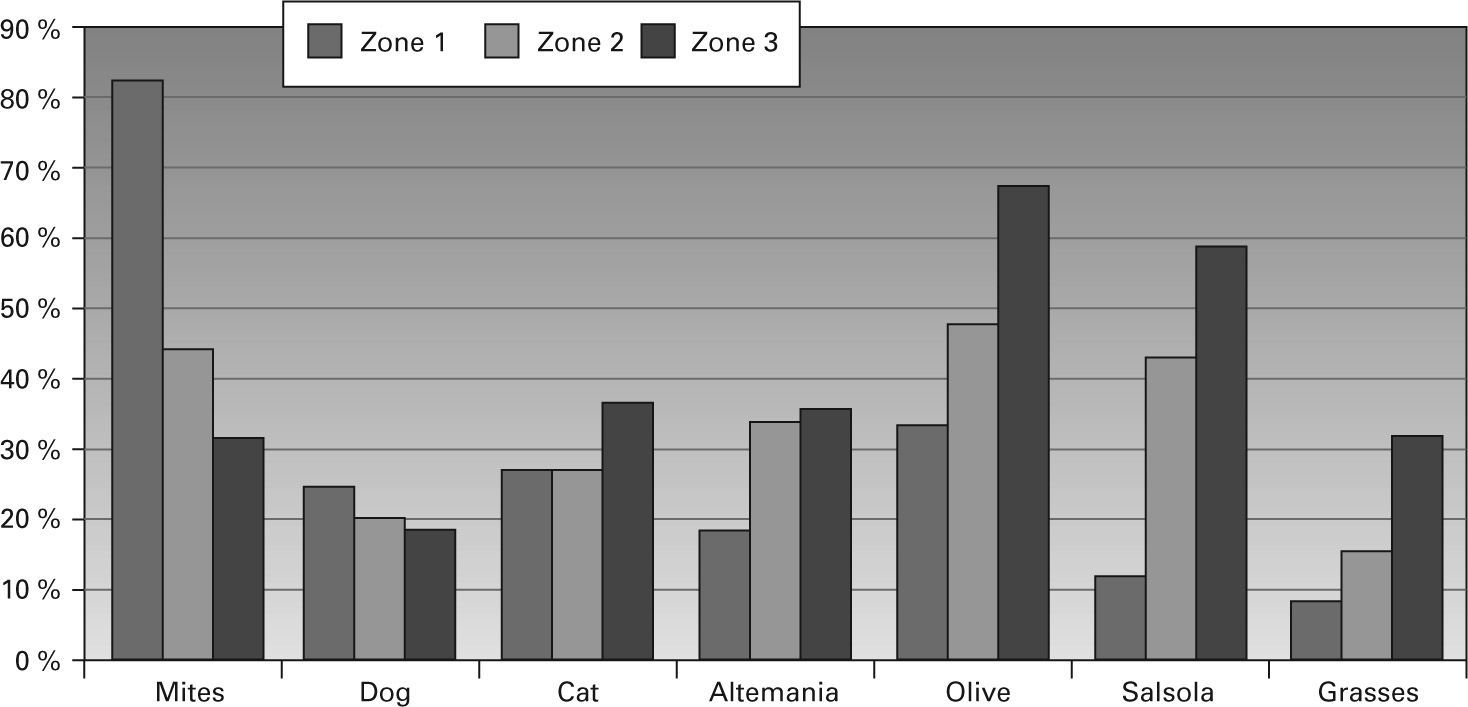
Three hundred and forty-six patients were living in zone 1 of whom 74.9 % were atopic, 1807 in zone 2 (69.7 % atopic) and 913 in zone 3 (74.9 % atopic) (p = 0.007). The relative importance of the aeroallergens varied markedly in the different zones of study, as can be seen in figure 4, with a predominance of mites on the coast and pollens inland.
DISCUSSIONOur findings reflect the main allergologic characteristics of chronic rhinitis and asthma in the paediatric population in our region. Although ours is a cross-sectional retrospective study of a selected population, the large sample size representing patients with predominantly non-mild disease from different hospitals with a high degree of homogeneity, both from the point of view of the population treated as well as from that of the healthcare provided, makes it more robust. In addition to the typical limitations of retrospective studies, two specific ones should be mentioned. On the one hand, throughout the study we refer to “mites” since it was not possible for us to separate the results for D. pteronyssinus from those for D. farinae, although we know that the first is more common in our setting and that there is intense cross-reactivity. Likewise we refer to Salsola pollen since we do not have the individual results for Chenopodium and Salsola, although Salsola pollen predominates in our region and the cross-reactivity is also intense.
The 7 main aeroallergens allow 97 % of atopic patients of paediatric age to be detected; and this percentage rises to 99 % if we include 4 food allergens. However, these data are not homogeneous for all ages. Almost all the very young children treated were suffering from asthma and usually not sensitized to allergens. They represent the children with transitory and non-atopic wheezing in Tucson's study, to whom we diagnose as having non-allergic childhood asthma.3 Among atopic patients in the first years of life sensitization to food allergens (egg and milk) predominated over that to aeroallergens. This situation is reversed as the child gets older and the percentage of sensitized children increases sharply. The initial importance of food allergens and the early increasing importance of aeroallergens after the first years of life are findings supported by other studies.4–6 Rhinitis becomes more and more frequent and is a more accurate marker of atopy than is asthma, whose frequency diminishes with age. From the age of 9years on, the frequency of aeroallergen sensitization stabilizes and appears to reach a maximum of over 90 %. It is especially intense in the case of concomitant asthma and rhinitis, and this may be seen from an early age. Food allergens appear to lose their importance in school age children with exclusively respiratory disease.
With only 5 aeroallergens we were able to detect sensitization in over 98 % of atopic patients over 6years of age. The ECRHS-I study recommends a battery of 7 aeroallergens to detect the majority of atopic subjects in Western countries.7 If we had followed these recommendations in our population, we would have detected only 94 % of our atopic patients. In this respect, the local importance of Salsola should be mentioned. This allergen is not usually recognised in Europe,8 but it is in North America.9
The relative importance of each of the aeroallergens becomes evident very early on in childhood and tends to remain stable. However, the behaviour of Alternaria appears to differ from that of the other allergens, since it increases sharply in early childhood and is the main allergen in 3year old and 5year old children. It reaches a maximum in 7year olds and then stabilizes or even decreases in older children. The especial importance of mould as a cause of early onset allergy in childhood and adolescence and its stabilization or decrease at later ages has been described in other studies.6,9–12
The frequency of polysensitization is notable (74 % of all atopic patients) even though we are dealing with a paediatric population. The frequency of monosensitization is noteworthy in the case of egg (in very young children), mites and Alternaria and to a lesser extent Salsola pollen; whereas it is very rare in the case of the other allergens.
Our study shows differences in the allergens predominant in the different areas of a reduced geographical region, and the strong influence of the proximity of the sea on the aeroallergenicity. The climatic conditions of the coast (humidity, salinity, thermal stability, breezes, etc) may favour sensitization to mites, while protecting against sensitization to pollens and Alternaria. Differences are clearly seen as we move just a few kilometres away from the coast, between the coastline (zone 1) and the coastal plain (zone 2). Sensitization to pollens increases as we move away from the coast to the mountainous valleys inland (zone 3), whereas sensitization to animal epitheliums does not appear to be influenced by the geographical region to the same extent. The predominance of sensitization to mites along the coast and to pollens or Alternaria inland is well-known in Spain and in other countries.13,14 However, we found no other studies reporting the exact distance from the coast at which this effect becomes apparent. We can not exclude other social non-climatic factors for these differences, such as agricultural practices.
In conclusion, we have described the allergologic characteristics of a large population of children suffering from rhinitis and asthma in a relatively homogeneous geographical area. Despite this homogeneity we found differences related to age and bioclimatic conditions. We have described the predominant allergens in our region, underlining the local importance of Salsola and the early sensitization to Alternaria. The effect of the proximity of the coast, which favours sensitization to mites and protects against sensitization to pollens and Alternaria, has a surprisingly small radius of action in our region.