Reported prevalence of the insect stings and rates of allergic reactions vary among studies. The aim of the present study was to carry out the first epidemiological study on the prevalence of Hymenoptera allergy among school children in Izmir, Turkey.
MethodsWe planned to reach 6100 children, assuming the frequency of allergic reactions to Hymenoptera stings as 20%. Thirty-seven and eight schools were chosen from rural and urban areas, respectively. Parents were asked to complete a questionnaire which included questions about history of insect stings and the presence of atopic disease. All cases with severe systemic reactions and a representative sample from the remaining population were surveyed by telephone afterwards.
ResultsA total of 8565 questionnaires were distributed and the response rate was 70.8%. Of the 5602 children, 61.6% were stung at least once in their lifetime. Of these, 24.3% had a LLR, 8.1% had a MSR, 0.8% had a SSR. Overall reliability of the questionnaire was calculated as 40.7% for SSR and 91.6% for other reactions after telephone survey. On logistic regression analysis, male sex and rural residence were associated with a higher risk of being stung (OR: 1.39; CI 1.25–1.56; OR: 4.37; CI 3.36–5.69, respectively). Male subjects and asthmatic children were more likely to experience a SSR (OR: 2.44; CI 1.06–5.65; OR: 3.3; CI 1.52–7.19, respectively).
ConclusionHymenoptera stings are common in our population and large local reactions are the most common type of reactions. Prevalence of severe reactions is low in our population compared to previous studies.
Stinging insects of the Hymenoptera order are one of the most common causes of anaphylaxis worldwide.1,2 The incidence of insect sting fatalities from anaphylaxis ranges from 0.03 to 0.48 fatalities per one million inhabitants per year, which account for nearly 20% of fatal anaphylaxis from any cause.3 However, it is the only successfully curable form of anaphylaxis with immunotherapy, which places Hymenoptera allergy in a unique place in the field of allergy.4
The prevalence of systemic reactions (SRs) to Hymenoptera stings has been studied in various studies revealing the prevalence of SRs between 0.5%–3.3% among adults in America and 0.3%–7.5% in Europe.5,6 Prevalence of systemic reactions is lower in children, ranging from 0.15% to 0.8%.3 The reported prevalence of insect sting and rates of allergic reactions differ among studies because of multiple variables including regional differences, exposure rates, differences in characteristics of the study population and also according to the different data collection methods of the different studies.
The present study was conducted in Izmir, which is the third largest city of Turkey situated in the west of the country with a population of 4 million and characterised by a warm climate all over the year. This study emerged from the observation of the low number of children receiving venom immunotherapy in three large referral allergy centres in Izmir and aimed to carry out the first epidemiological study on the prevalence of Hymenoptera allergy among school children in Izmir as well as to evaluate the factors associated with Hymenoptera venom allergy.
Materials and methodsPatient populationWe planned to reach 6100 children based on the study of Graiff et al.7 who reported the frequency of allergic reactions to Hymenoptera stings as 20% (1% precision, 95% CI). Rural and urban areas are defined as regions with a population of under and over 20,000, respectively. Thirty-seven and eight schools were chosen from rural and urban areas by simple random sampling reflecting the distribution of population in our city to reach an average 7220 children, with 20% excess of the target population. The participants were the parents of the school children aged 12–14 years attending the seventh and eighth classes of the elementary school. The parents of the children in selected schools received an explanatory letter requesting an informed consent for the study with a questionnaire. Parents willing to participate in the study were asked to complete the questionnaire which included the questions about history of insect stings, type of reaction, presence of hospital attendance and the presence of atopic disease. The questionnaires were collected 2 weeks after distribution. All cases with severe systemic reactions (SSR) and a representative sample from the remaining population which was calculated based on the error rate of SSR were surveyed with telephone afterwards.
QuestionnaireThe questionnaire was comprised six questions regarding Hymenoptera stings which were used in previous study by Graif et al.7 and three questions regarding atopic diseases based on the International Study of Asthma and Allergies in Childhood Standard core questionnaire. Questions included whether the child had ever been stung, how many times the child had been stung, whether or not they had experienced the following reactions: a large local reaction (LLR), defined as a swelling on the sting site which was larger than 5cm and lasted for more than 2 days; a mild systemic reaction (MSR) defined as a skin reaction like rash or swelling except for the sting site within one hour of the sting; severe systemic reaction (SSR), defined as difficulty in breathing, an asthma attack, abdominal pain or loss of consciousness within one hour of the sting. The last question regarding stings was about hospital attendance after insect sting. Finally parents answered yes or no to the questions related to the presence of asthma, allergic rhinitis and eczema in their children.
Institutional ethical board approval was obtained for the study.
Statistical analysisStatistical analysis was done with SPSS package 15.0 (SPSS Inc., Chicago, IL, USA). A multiple logistic regression model was used to evaluate the association between the allergic reactions and the risk factors. Odds ratios were presented with 95% confidence intervals. A p value less than 0.05 was considered as significant.
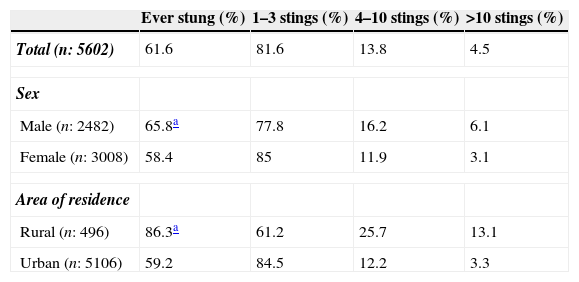
ResultsA total of 8565 questionnaires were distributed to 45 schools, 5602 completed (regarding critical questions about being stung) and 465 incomplete questionnaires were returned with a response rate of 70.8%. Of the 5602 children, 3449 (61.6%) were stung at least once in their lifetime. The prevelance of being stung was 86.3% in rural areas while it was 59.2% in the urban areas. Male subjects and living in rural areas were found to have a high risk of being stung on logistic regression analysis (OR of 1.39 and 95% CI 1.25–1.56 for male children; OR of 4.37 and 95% CI 3.36–5.69 for children living in rural areas. Characteristics of the study population being stung are given in Table 1.
Characteristics of the study population being stung.
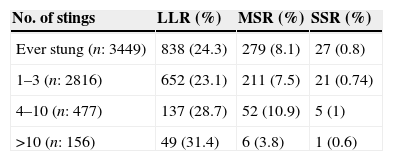
In the subset of children being stung, 24.3% had a large local reaction (LLR), 8.1% had a mild systemic reaction (MSR), 0.8% had a severe systemic reaction (SSR) representing 15%, 5% and 0.5% of the whole population, respectively. Hospital attendance was 10.7% in the subjects being stung (6.6% in the whole group) while it was 17.2%, 18.6%, and 40.7% in the LLR, MSR and SSR groups.
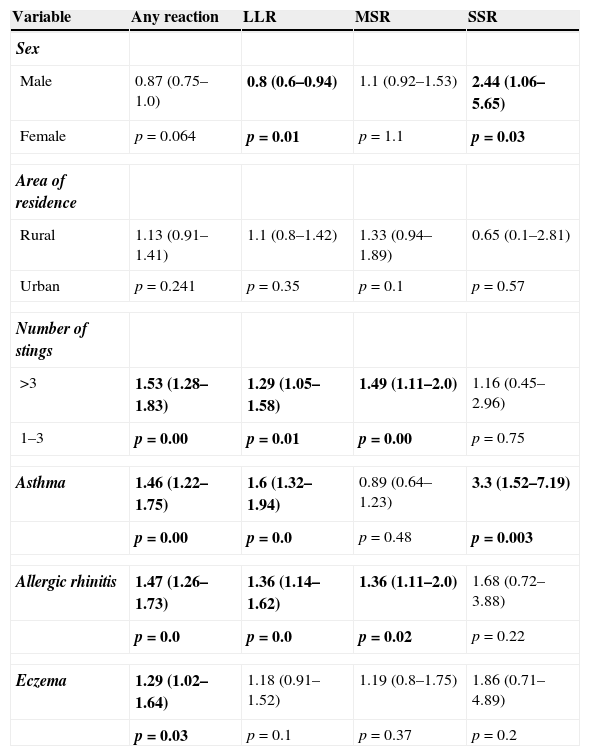
Having a reaction after being stung was found out to be associated with three or more number of stings (OR: 1.53, 95% CI: 1.28–1.83). No significant difference was noted in the rates of LLR and MSR between subjects living in rural and urban areas. Having a reaction after being stung was more common in children having asthma, allergic rhinitis and eczema (Table 2). Local large reaction was more common in female subjects (p=0.01) while there was not any difference between male and female subjects in the rate of MSR. Number of stings more than three was associated with the risk of LLR and MSR (OR: 1.29 95% CI: 1.05–1.58, OR: 1.49% 95 CI: 1.11–2.0, respectively). Males were two times more likely to experience SSR (OR: 2.44 95% CI 1.06–5.65) than female subjects while there was not any difference between urban and rural residence.
The prevalences of LLR, MSR and SSR and ORs are presented in Tables 2 and 3.
Odds ratios (95% CIs) for allergic reactions.
| Variable | Any reaction | LLR | MSR | SSR |
|---|---|---|---|---|
| Sex | ||||
| Male | 0.87 (0.75–1.0) | 0.8 (0.6–0.94) | 1.1 (0.92–1.53) | 2.44 (1.06–5.65) |
| Female | p=0.064 | p=0.01 | p=1.1 | p=0.03 |
| Area of residence | ||||
| Rural | 1.13 (0.91–1.41) | 1.1 (0.8–1.42) | 1.33 (0.94–1.89) | 0.65 (0.1–2.81) |
| Urban | p=0.241 | p=0.35 | p=0.1 | p=0.57 |
| Number of stings | ||||
| >3 | 1.53 (1.28–1.83) | 1.29 (1.05–1.58) | 1.49 (1.11–2.0) | 1.16 (0.45–2.96) |
| 1–3 | p=0.00 | p=0.01 | p=0.00 | p=0.75 |
| Asthma | 1.46 (1.22–1.75) | 1.6 (1.32–1.94) | 0.89 (0.64–1.23) | 3.3 (1.52–7.19) |
| p=0.00 | p=0.0 | p=0.48 | p=0.003 | |
| Allergic rhinitis | 1.47 (1.26–1.73) | 1.36 (1.14–1.62) | 1.36 (1.11–2.0) | 1.68 (0.72–3.88) |
| p=0.0 | p=0.0 | p=0.02 | p=0.22 | |
| Eczema | 1.29 (1.02–1.64) | 1.18 (0.91–1.52) | 1.19 (0.8–1.75) | 1.86 (0.71–4.89) |
| p=0.03 | p=0.1 | p=0.37 | p=0.2 | |
The relationship of a history of asthma, allergic rhinitis and eczema to the allergic reaction to sting was also investigated. There was a statistically significant relationship between having a LLR after being stung and having asthma and allergic rhinitis (OR: 1.60 95% CI 1.32–1.94 for asthma, OR: 1.36 95% CI 1.14–1.62 for allergic rhinitis). Children having an allergic rhinitis diagnosis were more likely to experience MSR (OR: 1.36 95% CI 1.11–2.0) while children having asthma were more likely to experience SSR (OR: 3.3 95% CI 1.52–7.19). Eczema was not found to be associated with LLR, MSR and SSR.
All the children who reported having SSR were surveyed again by telephone after the study. Of the 27 children, 11 children were found to have a severe reaction. Six of the remaining population were wrong in terms of filling and understanding the statements about SSR. A further 10 of the questionnaires were found to be filled out by children themselves who exaggerated the findings. According to this information, we calculated the reliability of the SSR as 40.7% and telephoned parents of 120 children with reactions other than SSR. Of the 106 parents available, information of 10 children (9.43%) was inconsistent with that in the questionnaire. Most of the inconsistency was about being stung or not and 20% was about the type of reaction. Reliability of the study in terms of other reactions was calculated as 91.6% after telephone survey.
DiscussionIn this study, we studied the prevalence of allergic reactions to Hymenoptera stings in our city, Izmir. We found that 61.6% of the school children aged 12–14 had been stung at least once in their lifetime. This study is the second prevalence study about Hymenoptera stings in children in Turkey after the first study conducted in Ankara in 1998. In this previous study, lifetime cumulative sting prevalence was 60.8%, which was similar to our study.8 Lifetime sting prevalence was found to be similar in countries sharing the same climate. In the study of Graif et al.7 which was conducted in Israel, the prevalence rate was 56.3%, whereas it was low as 37.5% in Irish children.9 Izmir has a mild climate and sunny days all year long and children spend more time outside, which may explain this high rate of being stung. Males and children living in the rural areas were also more commonly stung in our study as indicated in previous studies.7,9–11 This is also understandable because boys and children living in rural areas tend to spend much more time outdoors than girls and children in cities.
In this study, we found that 15% of the study population had LLR, 5% had MSR, and 0.5% had SSR. This prevalence of LLR seems to be higher from pediatrics studies from Ireland and Israel, which are 5.8% and 11.5%, respectively. Only one pediatric study from Italy reported a prevalence of LLR as high as 19.4%.12 However, the definiton of LLR was broader in that study without giving the specific size and duration. This high rate of LLR seems to be similar to previous adult studies conducted in smaller number of patients in Turkey and Spain, which may speculate the importance of genetic determinants of the type of reaction and atopy.13,14 Despite this rate of LLR, 27 children (0.5%) were reported to have SSR in our study. Previous studies from the 1970s reported that up to 0.4% of girl and boy scouts in United States had a history of systemic reactions to stings.15,16 Moreover, the rate of SSR was 0.8% in Ireland and 2.5% in Israel studies. Differences in studies may be due to the selected population, data collection methods (questions and definitions) and personal risk factors. However, we used the same questionnaire as the recent published studies from Ireland and Israel to uniform the definitions and compare the specific characteristics of our study population.
Hospital attendance was 10.7% in the subjects being stung (6.6% in the whole group) in our study group. It was found out to be 17.2%, 18.6%, and 40.7% in the children having LLR, MSR and SSRs, respectively. This ratio is generally higher than other countries because people can attend easily and directly to emergency services in our country. However, hospital attendance of children having SSRs should be increased with appropriate national education programmes.
Atopy and the risk of allergic reactions after being stung were studied in previous pediatrics studies. Graif et al.7 and Jennings et al.9 reported that having an asthma diagnosis resulted in an increased risk of severe reaction after being stung. We also found that if the child had a diagnosis of asthma, they are three times more likely to have SSR. Allergic rhinitis was also regarded as a risk factor for three types of allergic reactions in previous studies.7,17 We found that children with allergic rhinitis have an increased risk of only LLR and MSR. Having a diagnosis of eczema did not increase the risk of allergic reaction after being stung in our study.
Questionnaire-based data collection is useful and widely used in population-based prevalence studies. In this study, we used a questionnaire targeted to parents of the relevant children and we telephoned parents of these children to have secondary checks about the responses of questionnaires. However, we discovered errors in the group reporting SSRs especially. One of the major drawbacks was the tendency of the children to fill out the questionairre themselves and exaggerate their history about the reaction. This made the reliability of the SSR as low as 40.7%. But, this was not true for other types of reactions. We think that one should be cautious when interpreting results from questionnaire-based studies if the study is conducted through the adolescent group. Although we have tried to make a secondary survey by phoning a representative sample of the study group, our study could have overestimated the prevalence of allergic reactions. It is also recognised that the history is not perfectly correlated with the diagnosis made after diagnostic tests, and there are examples of inconsistency between history and diagnostic tests in wasp allergy in Turkey.18
In conclusion, we found that Hymenoptera stings are common in Turkish school children and the rates of allergic reactions resemble those of adults. Large local reactions are the most common type of allergic reactions although severe systemic reactions are rare. Male sex and asthma diagnosis were found to increase the risk of SSR after being stung in our study population.
Although hospital attendance is higher in each type of allergic reactions in our country compared to other countries, accurate education programmes for emergency physicians and public are needed to direct the right person to appropriate emergency care.
FundingNone.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in the study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Conflict of interestThe authors have no conflict of interest to declare.