Food allergy is a very frequent and increasingly common disease in children and adolescents. It affects quality of life and can even be life-threatening. Given that 10–18% of allergic/anaphylactic food reactions take place in schools, it is essential to provide school personnel with training on the management of reactions.
MethodsThe Allergy Unit of Hospital Universitario de Fuenlabrada, Spain, organized a conference entitled “Management of Food Allergy in Children and Adolescents in School Centers” during which teachers, cooks, cafeteria monitors, and summer-camp leaders underwent a training course. Attendees filled out a questionnaire with eight questions before and after the course to assess their self-efficacy in management of food allergy and anaphylaxis. The results were compared.
ResultsA total of 191 people participated (51% dining-room monitors, 24% teachers, 13% cooks, and 12% other professions). The areas in which the attendees presented the lowest confidence before receiving the course were recognition of symptoms and treatment of the reactions/anaphylaxis. The mean score for each of the eight concepts evaluated improved after the training course. This improvement was significant in the management of anaphylaxis.
ConclusionsOur study demonstrates the usefulness of a self-efficacy scale in school personnel as a tool to assess the ability to manage food allergy and anaphylaxis. It can help to identify problem areas in which more specific training programs can be implemented.
Food allergy is a common condition that affects 4–8% of European schoolchildren.1 It has a considerable impact on quality of life and can even be life-threatening. The incidence of anaphylaxis, especially food anaphylaxis and anaphylaxis affecting the pediatric population, has increased in recent years. Food allergy in Spain has doubled in just over a decade in patients referred to Allergy Departments, going from a prevalence of 3.6% in 1992, to 7.4% in 2005 and to 11.4% in 2015.2 A 1.89-fold increase in admissions due to anaphylaxis was recorded in Spanish hospitals during 1998–2011, particularly in patients aged 0–14 years (1.65- to 3.22-fold until 2009 and 4.09- to 12.59-fold until 2011). Admissions to hospital for food anaphylaxis increased in all age groups (2.78-fold until 2009 and 8.74-fold until 2011).3
During the school year 2016/2017, there were more than 8,000,000 students in Spain; of these, more than 6,500,000 were children aged between 3 and 16 years who were enrolled in infant, primary, and secondary education. Of the almost 28,000 education centers in Spain, some 18,000 have a school cafeteria, where two million children are fed daily. It is estimated that approximately 450,000 schoolchildren in Spain have food allergy.4 Considering that 10–18% of cases of food-induced allergic reaction and anaphylaxis occur in school,5 the school environment clearly presents very significant challenges in the management of potentially fatal food allergies.
The figure of the school nurse is well established in the United States and several European countries. In Spain, this is a recent development, and the presence of a nurse in schools is not equally distributed throughout the country. Therefore, in most cases, the responsibility for the management of schoolchildren with food allergy lies with the school staff. Several publications report deficiencies in the knowledge and management of allergic reactions by school staff, who are in daily contact with allergic children at risk of a reaction. The main limitations are in recognition of the symptoms of an allergic reaction and the delay in the administration of treatment, in particular adrenaline.6–9 Studies specifically designed to assess the self-efficacy of school staff have revealed serious deficiencies in the management of food allergy and in the treatment of allergic reactions in schoolchildren. They emphasize the need for specific educational interventions to ensure adequate management and treatment of these children.10–13 Supporting this recommendation, some studies show the importance and usefulness of training courses in improving the management of food allergy by school staff. A Japanese study on school nurses, teachers, and care workers involved with children who had been prescribed an adrenaline auto-injector showed that training with practical instruction resulted in a dramatic improvement in self-efficacy.14 In the United States, an educational intervention project based on a pretest–posttest control group design significantly increased teacher knowledge of the causes of food allergy, as well as of treatment.12 In a recent Italian study, a self-efficacy scale was proposed to identify specific weak areas in the management of food allergy by school staff. This questionnaire was based on clinical expertise previous research of the group and Bandura's guidelines for constructing self-efficacy scales. The results support the usefulness of such a scale for the identification of weak points and highlight the need to develop training programs designed specifically for the needs of school personnel. The authors suggested that the test could be used to assess the effectiveness of training and to measure changes in self-efficacy before and after the courses.15
The aim of the present study was to analyze the effectiveness of a program for training school staff in the management of food allergy and anaphylaxis, applying the test developed specifically for this purpose by Polloni.15
MethodsIn March 2017, the Allergy Unit of Hospital Universitario de Fuenlabrada, Fuenlabrada, Spain organized a Conference entitled “Management of Food Allergy in Children and Adolescents in School Centers”. The conference was aimed at teachers, cooks, dining-room monitors, and summer-camp leaders in the hospital's catchment area. The main objectives were to establish key areas in the prevention of allergic reactions to food in school, to learn to identify these reactions, and to know how and when to administer appropriate treatment.
The structure of the conference was as follows:
- •
Introduction, definition and epidemiology of food allergy. Problems of the child/adolescent with food allergy in educational centers.
- •
How to recognize an allergic reaction. How is the diagnosis of food allergy made?
- •
How to avoid an allergic reaction. Prevention measures. Coordination between the center, family, and doctor. Commitment of the educational center.
- •
Treatment of an allergic reaction to food. Treatment of anaphylaxis. Emergency action plan.
- •
Practical management workshop: medication, forms of administration, role-play.
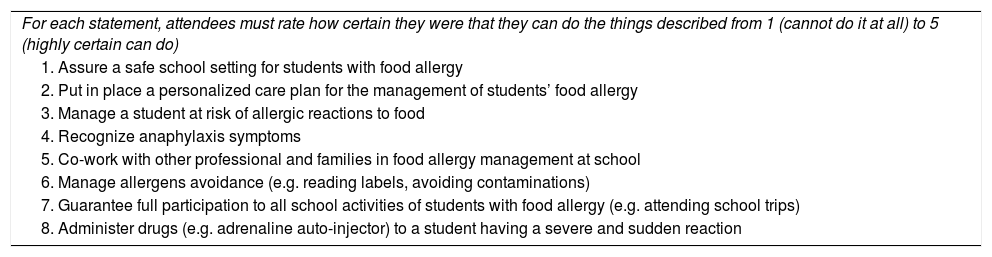
A total of 191 attendees answered eight questions (Table 1)15 before and after the conference to assess their self-efficacy in the management of food allergy and anaphylaxis. The results of both questionnaires were compared before and after the training session. In addition to these questions, data were also collected on profession, age, sex, and previous training in the management of food allergy. Data were collected anonymously. The attendees were informed of the objectives of the questionnaire and that the data could be analyzed for research purposes.
Questionnaire for school personnel's self-efficacy in managing food allergy and anaphylaxis at school.
| For each statement, attendees must rate how certain they were that they can do the things described from 1 (cannot do it at all) to 5 (highly certain can do) |
| 1. Assure a safe school setting for students with food allergy |
| 2. Put in place a personalized care plan for the management of students’ food allergy |
| 3. Manage a student at risk of allergic reactions to food |
| 4. Recognize anaphylaxis symptoms |
| 5. Co-work with other professional and families in food allergy management at school |
| 6. Manage allergens avoidance (e.g. reading labels, avoiding contaminations) |
| 7. Guarantee full participation to all school activities of students with food allergy (e.g. attending school trips) |
| 8. Administer drugs (e.g. adrenaline auto-injector) to a student having a severe and sudden reaction |
In addition, the attendees were presented with a clinical case involving a nut-allergic girl who experienced an anaphylactic reaction at school. Four possible options for action and treatment were proposed. The attendees were asked choosing the correct answer from the four options, before and after the course.
Statistical analysisQualitative variables are presented with their frequency distribution. Quantitative variables are expressed as mean and standard deviation (or median and interquartile range if the distribution is not normal). The association between qualitative variables was evaluated using the chi-square test or Fisher's exact test (if more than 25% of the expected values were less than 5). The behavior of the quantitative variables was analyzed for each of the independent variables using the Mann–Whitney test. These techniques enabled us to evaluate the differences in scores due to the main effect of the training action, both globally and by group (teachers and cafeteria monitors), as well as whether there were differences in previous training between these two groups. The distribution of the variable in the theoretical models was verified, as was the hypothesis of homogeneity of variances. The null hypothesis was rejected with a type I error or α error less than 0.05. The statistical analyzes were performed using IBM SPSS Statistics, Version 21®.
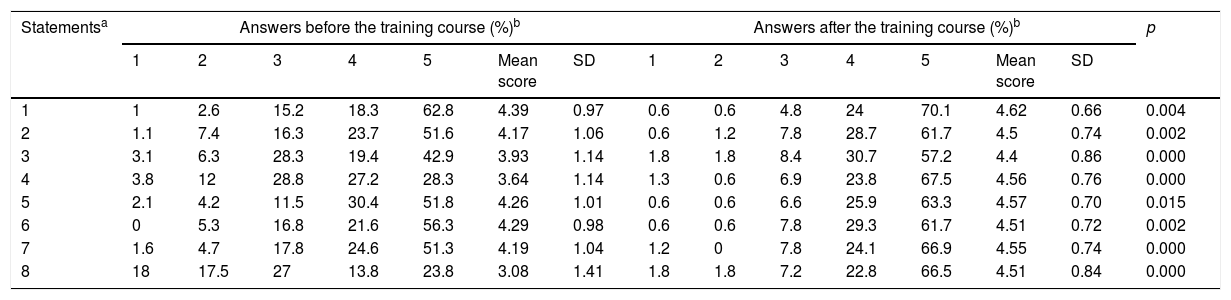
ResultsWomen accounted for 92% of the participants, and the mean age was 45.6 years (SD 10.8) (min, 20; max, 63); 51% were cafeteria monitors, 24% teachers, 13% cooks, and 12% other professions. A total of 43% reported having never received food allergy training, and 37% had received some type of training. When the jobs with the largest number of attendees were analyzed separately, 44% of the dining-room monitors and 39% of the teachers reported having received training. The aspects in which the attendees showed less confidence before receiving the course were in recognition of symptoms of food allergy and treatment of allergic reactions and anaphylaxis (questions 3 and 8) (p<0.05) (Table 2). When the whole sample was taken into consideration, the mean score for all eight concepts evaluated improved after the training received, with a much more significant improvement in the issues related to symptom recognition and management of anaphylaxis (p<0.05) (Table 2). By jobs, there were significant differences before and after the training in teachers for questions 2, 3, 4, 5, and 8 (p<0.05) and among cafeteria monitors for questions 2, 3, 4, 6, and 8 (p<0.05). No significant differences were detected for the remaining items. As for the case study, 25.5% of attendees obtained correct answers before the training, compared with 96.90% afterwards.
Comparison of participants’ answers before and after the training.
| Statementsa | Answers before the training course (%)b | Answers after the training course (%)b | p | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | Mean score | SD | 1 | 2 | 3 | 4 | 5 | Mean score | SD | ||
| 1 | 1 | 2.6 | 15.2 | 18.3 | 62.8 | 4.39 | 0.97 | 0.6 | 0.6 | 4.8 | 24 | 70.1 | 4.62 | 0.66 | 0.004 |
| 2 | 1.1 | 7.4 | 16.3 | 23.7 | 51.6 | 4.17 | 1.06 | 0.6 | 1.2 | 7.8 | 28.7 | 61.7 | 4.5 | 0.74 | 0.002 |
| 3 | 3.1 | 6.3 | 28.3 | 19.4 | 42.9 | 3.93 | 1.14 | 1.8 | 1.8 | 8.4 | 30.7 | 57.2 | 4.4 | 0.86 | 0.000 |
| 4 | 3.8 | 12 | 28.8 | 27.2 | 28.3 | 3.64 | 1.14 | 1.3 | 0.6 | 6.9 | 23.8 | 67.5 | 4.56 | 0.76 | 0.000 |
| 5 | 2.1 | 4.2 | 11.5 | 30.4 | 51.8 | 4.26 | 1.01 | 0.6 | 0.6 | 6.6 | 25.9 | 63.3 | 4.57 | 0.70 | 0.015 |
| 6 | 0 | 5.3 | 16.8 | 21.6 | 56.3 | 4.29 | 0.98 | 0.6 | 0.6 | 7.8 | 29.3 | 61.7 | 4.51 | 0.72 | 0.002 |
| 7 | 1.6 | 4.7 | 17.8 | 24.6 | 51.3 | 4.19 | 1.04 | 1.2 | 0 | 7.8 | 24.1 | 66.9 | 4.55 | 0.74 | 0.000 |
| 8 | 18 | 17.5 | 27 | 13.8 | 23.8 | 3.08 | 1.41 | 1.8 | 1.8 | 7.2 | 22.8 | 66.5 | 4.51 | 0.84 | 0.000 |
Food allergy is a major health problem in industrialized countries. It affects the entire population, although it is especially prevalent in children and adolescents. Since this age group spends a large part of the day at school, where they also eat meals, many of the food-induced allergic reactions occur in the school environment. The people who take care of these children should know how to manage reactions. It is very important to establish preventive measures in classrooms, playgrounds, cooking areas, food storage areas, and workshops, as well as during extracurricular activities, to ensure an appropriate balance between avoidance of reactions and safe participation of allergic children in activities with their classmates, thus ensuring integration and non-discrimination. Broad planning of the processes involved will ensure that fewer mistakes are made and that the student is better integrated. Improvisation should always be avoided, since small amounts of an allergen are enough to trigger an allergic reaction.
As this study has shown, training in the management of food allergy is infrequent in professionals who work daily with children in schools. According to the results of previous studies, we found that only 37% had received training.13 Since the presence of nurses in Spanish schools is not common, other jobs such as teachers and dining-room monitors are responsible for managing possible allergic reactions and should receive greater coaching in the recognition thereof. Previous studies have already shown that teachers’ knowledge of how to address emergency situations in food allergy is poor, although they have expressed a wish to receive training.13 Since it is necessary to know the training needs of the target group before developing specific intervention plans, we decided to carry out this training action in our area.
As published elsewhere,6,13 the areas where the participants showed the lowest self-efficacy were in recognition of symptoms and treatment of allergic reactions, especially in the administration of adrenaline. A significant improvement was observed in all areas after the training course, especially in the recognition of reactions and the administration of adrenaline. Consequently, training actions carried out by allergists with broad experience in the management of food allergy are highly useful. Analysis of the best-represented jobs among the attendees (teachers and dining-room monitors) revealed significant improvements in the same questions in both groups (questions 2–4 and 8), although the difference between before and after the training course in question 5 (“Work with other professionals and families on the management of food allergy at school”) was significant for teachers. In contrast, the difference in question 6 (“Manage allergen avoidance [e.g. reading labels, avoiding contamination]”) was significant for dining-room monitors. Therefore, an interesting and logical observation can be made: all the participants improved their general knowledge of the problem and improved specific knowledge on the management of anaphylaxis. However, depending on the jobs, training led to improvement for situations more directly related to their work, although this was not as clear-cut in areas not directly related to their daily work.
In conclusion, the present study highlights the interest and need for training in the management of food allergy by school and canteen staff. It also shows the usefulness of a self-efficacy scale that can be used by school staff, as a tool to evaluate the ability to manage food allergy and anaphylaxis. This tool can identify areas in which professionals have more difficulties in addressing the disease and thus help them to implement more specific training programs.
Conflict of interestThe authors have no conflict of interest to declare.
We would like to thank Tomas Sebastian Viana, Supervisor of Innovation and Development in Hospital Universitario Fuenlabrada, for his help in carrying out the statistical analysis.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
This work has been presented as a poster in the International Symposium on Aerobiology, Pollution and Climate Change of the SEAIC held in Murcia from October 26 to 28, 2017.
Pediatric Allergy and Immunology permission has been requested and obtained to reproduce Table 2 of the paper: Polloni L, et al. School personnel's self-efficacy in managing food allergy and anaphylaxis. Pediatr Allergy Immunol 2016;27:356–60.