To the Editor:
The most frequent cause of ischemic heart disease is reduced blood flow due to atherosclerotic lesions of the coronary arteries. Less frequently, reduced blood flow is due to vasospasm, localised in the atherosclerotic plaque or in healthy arteries.
Other less common causes of myocardial ischemia are anaphylactic shock, allergic angina syndrome (Kounis syndrome), embolism, spontaneous dissection, arteritis and other vasculitis. These causes mainly affect young individuals without coronary risk factors or patients with generalised arterial illnesses. There are also a small percentage of cases in which increased oxygen demand (severe arterial hypertension, tachycardia, anemia) can trigger ischemia in individuals with or without obstructive lesions.
We present the case of a patient with a MI after suffering anaphylactic shock.
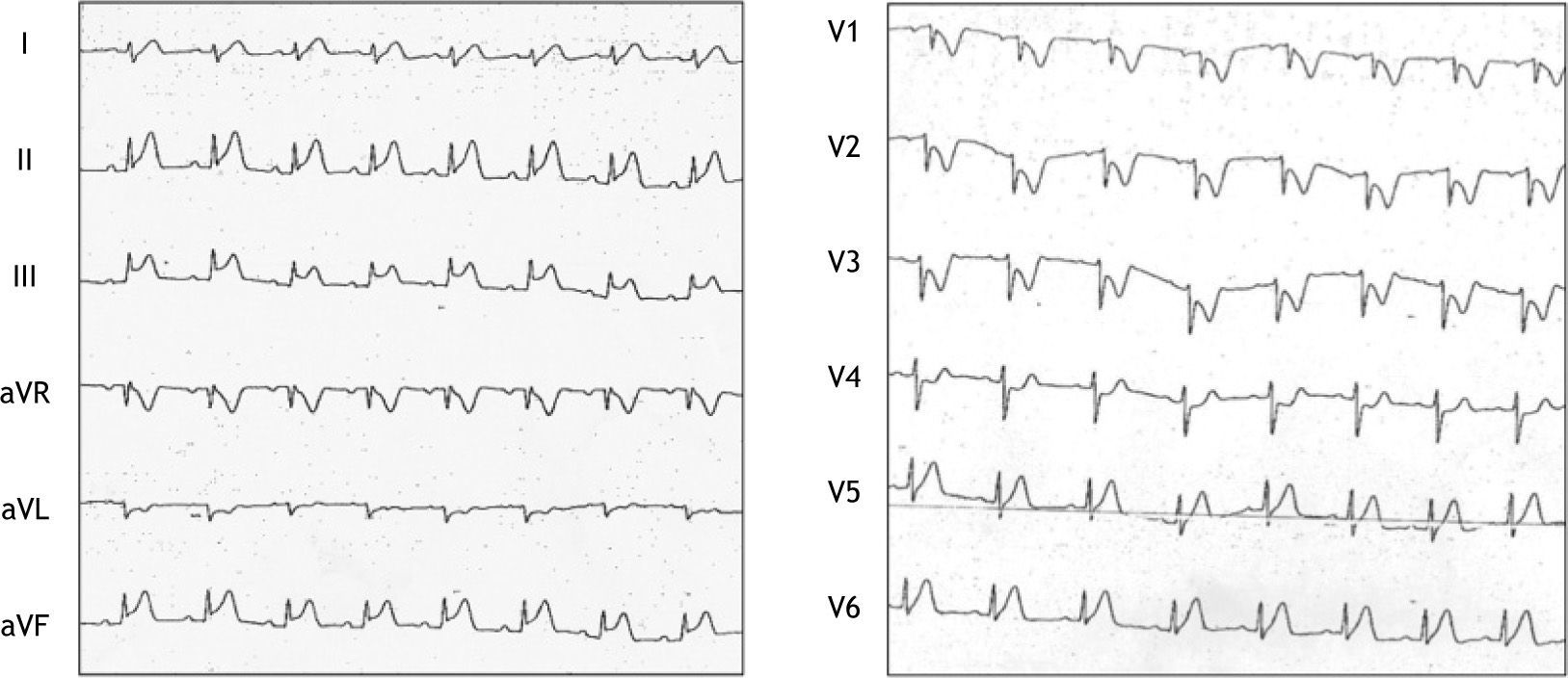
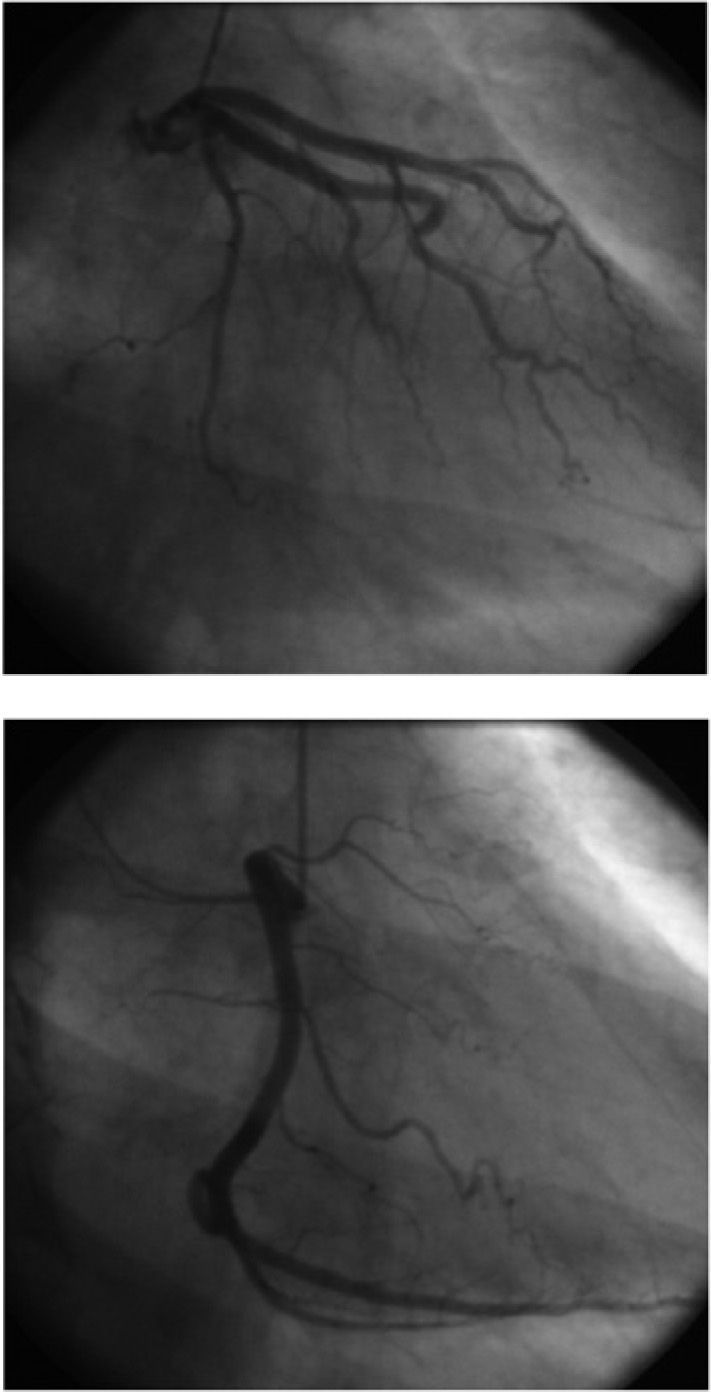
A fifty-year-old woman, without cardiovascular risk factors, allergic to acetylsalicylic acid, diagnosed of bronchial asthma treated with salmeterol and fluticasone. She visited her Health Centre (HC) complaining of cephalea, rhinorrhea and nasal congestion, suggesting sinusitis. She was administered intramuscular metamizol and prescribed clavulanic amoxicillin and ibuprofen, which she took 45 minutes later. After 10 minutes she presented sudden dyspnea, dizziness and palpitations without chest pain, and returned to the HC, where severe hypotension (69/39mmHg) and hypoxemia (O2 saturation: 65 %) were detected. Anaphylactic shock was suspected and she was treated with 1mg of subcutaneous adrenaline. Self-limited episodes of ventricular tachycardia were observed. After fluid and bronchodilators administration, her blood pressure and her dyspnea improved, although she still complained of chest pain. The ECG showed sinus bradycardia, 2mm ST segment elevation in DII and aVF and ST depression in V1-V4 (fig. 1). Posteroinferior MI was suspected, and she was brought into our hospital's Emergency Department. On arrival she presented systolic blood pressure of 80mmHg, without response to volume loads and, despite treatment with intravenous nitroglycerin, residual chest pain, but her ECG had normalised. She was transferred to ICU. She again presented severe chest pain and 2mm ST elevation in inferior segment leads. Thrombolysis with TNK was performed and two hours later the ECG was normal. Doppler-echocardiography revealed no alterations. Twenty-four hours after admission, her serum tryptase level was 14.1μg/L (5.5-13.5μg/L) and two weeks later 3.23μg/L. Her histaminuria level was 74.3nmol/24h (75–450nmol/24h). The patient was treated with antihistamines, corticoids, bronchodilators and aspirin. Her condition stabilised 48 hours after admission. She was then transferred to the Internal Medicine department, where she remained asymptomatic. Coronary angiography was normal (fig. 2). Consultation was undertaken with the Allergy Unit, which requested specific IgE antibodies for penicillin G, V and amoxicillin. IgE was positive for penicillin V (0.40 UI/ml) and negative for the others. Because of the characteristics of the reaction, no provocation test was given for Non Steroidal Anti Inflammatory Drugs (NSAID), and intolerance was diagnosed. A CT scan of the paranasal sinuses revealed massive occupation of these, in the context of probably ASA triad.
This patient presented MI after suffering an anaphylactic shock on taking NSAID and clavulanic amoxicillin, and was treated with adrenaline. Few medical studies discuss the involvement of this antibiotic in these processes1–5.
The mechanisms that trigger an acute coronary syndrome (ACS) from an anaphylactic reaction are diverse and not fully understood, being less frequent in patients with normal coronary arteries6–8, like our case. It is accepted that mediators of anaphylaxis7,9, massively released during the reaction, cause vasospasm. The Kounis syndrome is caused by release of inflammatory mediators during mast cell degranulation, and sometimes, also caused by progresses to myocardial infarction10. In patients with atherosclerotic coronary disease, hypotension compromises distal flow, while local action of histamine11 in the atheroma plaque, could rupture it and cause platelet aggregation.
Moreover, adrenaline administered to treat the shock, potentiates coronary vasospasm12,13, thus slowing down the blood flow and favouring the formation of blood clots and, therefore, arterial occlusion. In this patient, fibrinolysis minimised this effect, the patient's condition returned to normal and, as the coronary angiography revealed, she suffered no sequel, which is not always the case14.
In this case study, anaphylactic shock appears to be the main cause of acute MI, so our patient probably suffered Kounis syndrome, though we cannot rule out the role of adrenaline as an etiological agent. However, the fact that, some hours after administration of the vasoconstrictor, the patient's coronary symptoms and ECG changes returned, suggests a role for biphasic anaphylactic reaction15 and indicates that this was responsible for the patient's ACS.