Assess whether the Asthma, Sport and Health (ASAH) programme taught by teachers improves asthmatics’ quality of life, asthma knowledge, and reduces school absenteeism.
DesignRandomised cluster trial parallel group.
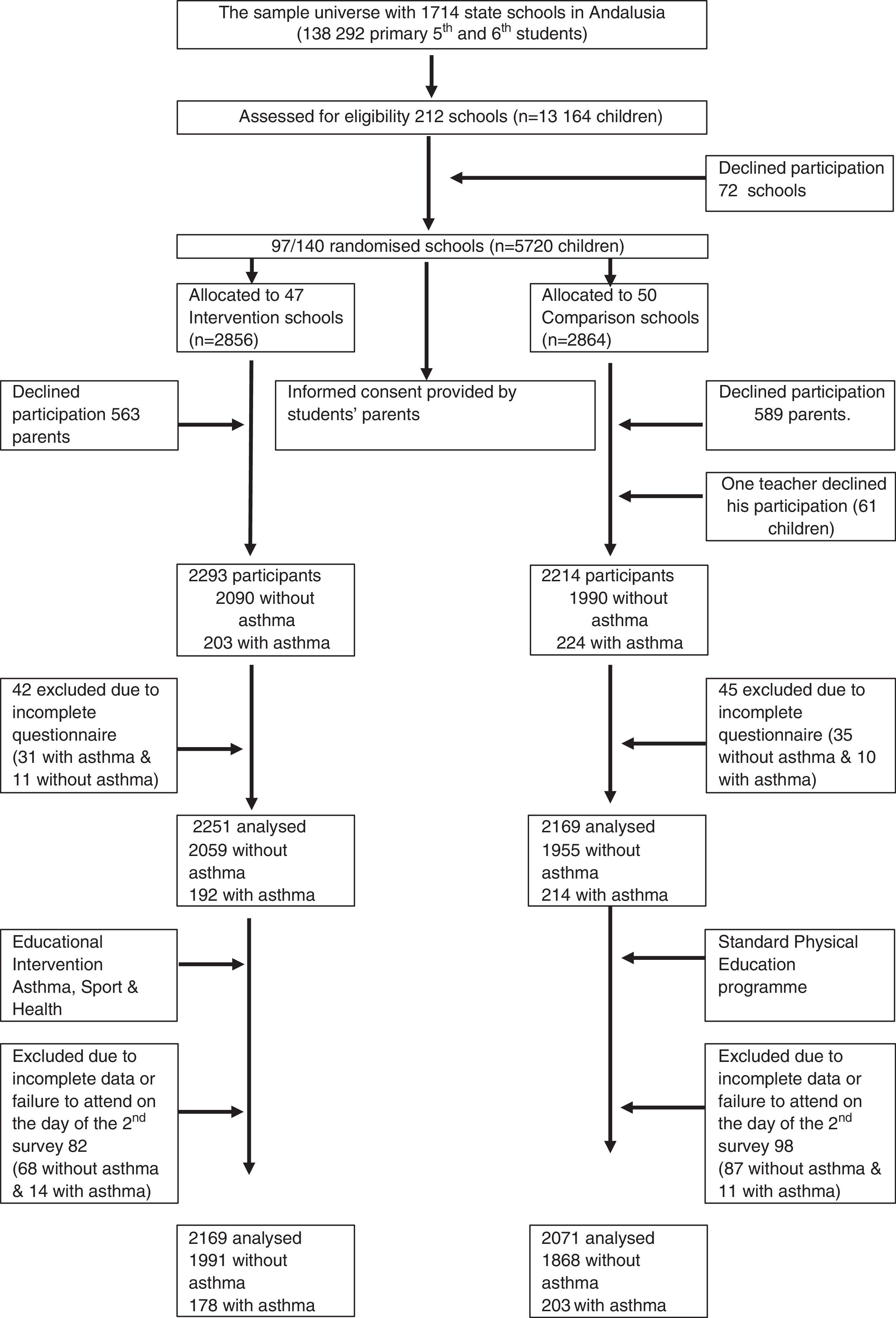
Participants2293 students (203 asthmatic) in the Intervention School group (IS) and 2214 in the Comparison School (CS) (224 asthmatic) belonging to primary school.
InterventionImplementation of the educational programme “Asthma, Sport and Health” at grade schools, taught by physical education teachers.
Main outcomeQuality of life according to the Pediatric Asthma Quality of Life Questionnaire (PAQLQ).
Secondary outcomesAsthma knowledge, asthma control, school absenteeism.
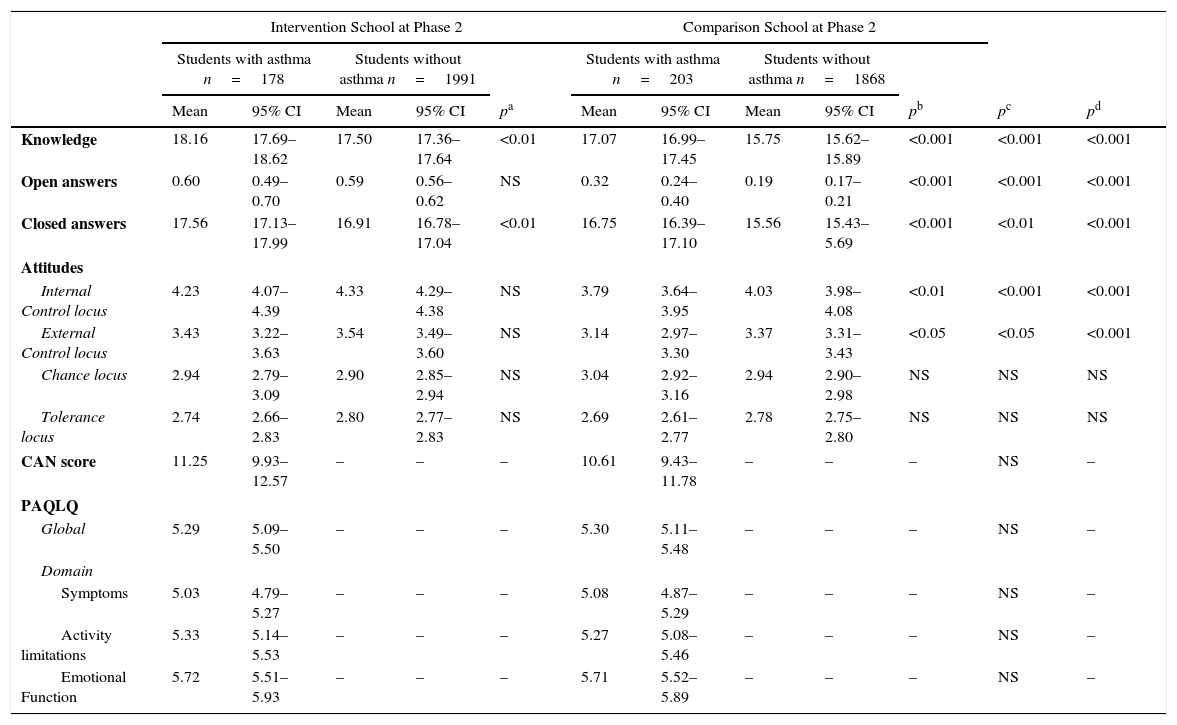
ResultsAfter implementing the programme in the IS group, global quality of life improved significantly (p<0.001) as did their domains, symptoms (p<0.001), emotional function (p<0.001) and activity limitations (p<0.01), while in the CS group improvement was seen in global life quality (p<0.01) without any significant changes in the domains for emotional function and activity limitations. Asthma knowledge only increased in IS, among asthmatic students from 16.51 (CI 95% 16.04–16.98) to 18.16 (CI 95% 17.69–18.62) (p<0.001) and students without asthma from 15.49 (CI95% 15.36–15.63) to 17.50 (CI95% 17.36–17.64) (p<0.001). The multiple regression analysis showed that quality of life and its domains depend on asthma knowledge and above all, having well-controlled asthma. We found no decrease in school absenteeism.
ConclusionsThe ASAH programme improved certain quality of life aspects regarding asthma (emotional function and limitation of activities) and asthma knowledge, but it failed to reduce school absenteeism NCT01607749.
In Spain, asthma has a prevalence of approximately 10%, although there are geographic variations between coastal and inland populations.1 In recent years, asthma has increased among 6–7-year-old children.1,2 Asthma affects children's physical activities, resulting in negative repercussions for their quality of life and school performance.3 Asthmatic adolescents are at a greater risk of suffering anxiety,4 feeling ashamed or worried about being taunted by classmates when they have to take medication, in addition to feeling a lack of support from their teachers and avoiding physical exercise.5
Therapeutic education is an essential component in asthma patient management; it includes understanding the disease, correct use of medication, avoiding triggers, symptom-based decision-making and participation in self-management.6 Educational outcomes vary greatly depending on the scenario (primary care, hospital, schools), the professionals involved (doctors, nurses, pharmacists, teachers), the methodology used (single or multifaceted intervention) and tested outcomes7 (inhalation therapy skills, pulmonary function, school absenteeism, symptoms, asthma control or quality of life). Education for self-management achieves greater results for most outcomes; this is especially true when individualised teaching is provided for decisions based on daily symptoms or peak-flow meter.8 The best scenario for education in asthma is when patients are diagnosed, treated and monitored. However, educating asthma patients at school offers a number of potential advantages: it reaches children and adolescents with difficulties in accessing health care courses and could help classroom integration.9–11 The results are not consistent when researching quality of life, school absenteeism and symptoms, but are for asthma knowledge and improving self-management.7 In Spain, most schools have no nurses and when an asthmatic child has symptoms, it is the teacher who is faced with the situation. However, school teachers have limited asthma knowledge12–14 and are inadequately prepared for such situations. Training Spanish school teachers has improved their knowledge about asthma, but whether it improves the quality of life of their students with asthma has not been studied. The same holds true for knowledge about asthma, school absenteeism and students’ attitudes towards asthma.12
Following the Global Initiative for Asthma (GINA),15 Spain developed plans that consider education a key tool for asthma management. Nevertheless, asthma training courses at primary health care centres16 and hospitals face several difficulties.17 Schools are another resource to be explored. Specific teacher training to recognise the asthma symptoms in their students and help them, should medication be needed, could contribute to improving asthma care in the classroom. If teachers educate their pupils regarding asthma, even those without the disease, it is probable that these same students will better understand their classmates, thus improving integration. This, in turn, could influence quality of life and decrease school absenteeism, but a pilot programme must be launched to verify this point. We hypothesised that an asthma training programme, taught by grade school teachers, could improve the quality of life and knowledge about asthma, and modify attitudes towards the disease while at the same time decreasing school absenteeism among asthmatic students.
MethodsDesignRandomised cluster trial with parallel school-based groups. The intervention was “asthma education in asthmatic students and their classmates.” The study was approved by the Primary Care Health Care District Ethics and Research Committee in Seville, Spain.
ParticipantsThe sample universe included 138,292 students who were in 5th and 6th grade (approximately 10–12 years old), registered for the 2011–2012 course (1714 public schools) in the region of Andalusia, Spain. Inclusion criteria: Grade school students, either gender with sufficient reading and writing skills to fill out the questionnaire, with their parents providing a signed consent form.
Sample sizeWe calculated optimal size for the design of the randomised cluster trial without considering the groups. It was later adjusted for the effect of the cluster design using the formula 1+(m−1)*ρ, where m is the average size of the cluster and ρ the intra-class correlation coefficient. We established a power of test at 90% with a significance level of 5%, considering a difference of means for quality of life (PAQLQ) between Intervention Schools (IS) and Comparison Schools (CS) students with asthma of 0.5 points, with a standard deviation of 1.25, based on a previous study by our research group,13 with which an optimal sample size of 133 students was obtained for both the IS and the CS group. Given that the prevalence of childhood asthma in our population is 10%, the optimal sample size is 2660 students. We then applied the correction factor, bearing in mind the effect of the cluster design, considering the mean cluster size of 40 students (m=40) and an intra-class correlation coefficient of ICC=0.03, to obtain a final sample size in the randomised cluster design of 5773 students.
RandomisationSchool children were the analytical units; the randomised units were the schools (to avoid contamination of the programme at school).
Eighteen doctors who cover 212 schools (n=13,164 5th and 6th grade students) offered the Asthma, Sport and Health (ASAH) Programme at their schools, of which 140 agreed to participate (June-2011). We randomly selected 97 schools until the sample size was obtained (n=5720 students). Schools were designated as IS and CS; they were stratified as Coast, Mountain or Inland, by author NAL, using a randomised number generation process, seeking a similar number of elements in both groups. Forty-seven schools were assigned (2856 students) to IS and fifty (2864 students) to CS.
Study proceduresTogether with the parents’ written consent, we were informed whether the child had asthma or if the child had taken asthma medication in the past year. This information was used to deliver the corresponding questionnaire. Questionnaires were coded to identify each student while guaranteeing anonymity. School teachers knew the name and code for each student.
The 18 school doctors were trained to teach the ASAH Programme in a five-hour interactive seminar and they received an ASAH Programme kit for each school. Between October and November, school doctors prepared PE teacher seminars for the ASAH Programme at the Intervention Schools (IS). Teacher implication was followed-up and support was provided when difficulties arose. Prior to the student educational programme, teacher knowledge and attitudes were analysed. Upon completing the course, PE teachers were re-analysed and asked to fill out an assessment questionnaire about the educational package. Upon conclusion, each PE teacher received an ASAH Programme kit for his/her school. In November, the students at all schools filled out the initial questionnaire (Phase 1). The ASAH Programme was taught at all IS in less than six weeks between November and December, while at the Comparison Schools (CS), the standard subject syllabus was followed. After five to six months (April-May 2012), students filled out a new questionnaire (Phase 2) and PE teachers at CS were trained and given the ASAH Programme kit. This allowed comparisons to be made between the two groups, and comply with the study's ethics requirements.
Asthma, Sport and Health Educational ProgrammeThe ASAH Programme is comprised of three, 45-min sessions to be included in Physical Education classes as part of standard class subject matter. This package was developed jointly between school teachers and health care professionals. The programme teaches the symptoms of asthma, its triggers and how to avoid them, how to respond to an asthma crisis and ways to prevent asthma symptoms. Several teaching-learning methods including videos and slide presentations were integrated into the ASAH Programme to facilitate student interaction, as well as practical material such as straws to experiment how a person breathes when having an asthma attack, peak flow metres, spacer chamber and a canister of beta-2 adrenergic for use when a crisis arises. The programme promotes solidarity and awareness that caring for asthma is the patient's responsibility. The content and its validation had already been published.18,19
VariablesThe primary outcome was quality of life. Secondary outcomes included asthma knowledge, asthma control, school absenteeism, and attitudes towards asthma.
Data obtained from students:
- 1.
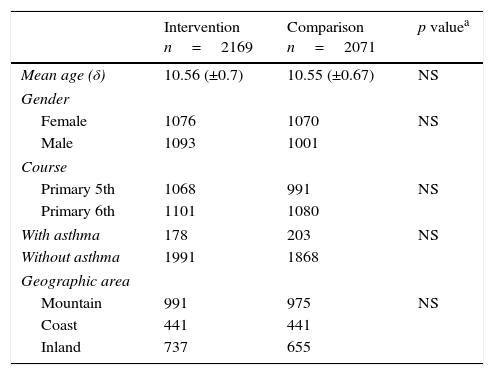
Participants’ socio-demographic data, according to Table 1.
Table 1.Characteristics of the 4240 students analysed in the study.
Intervention
n=2169Comparison
n=2071p valuea Mean age (δ) 10.56 (±0.7) 10.55 (±0.67) NS Gender Female 1076 1070 NS Male 1093 1001 Course Primary 5th 1068 991 NS Primary 6th 1101 1080 With asthma 178 203 NS Without asthma 1991 1868 Geographic area Mountain 991 975 NS Coast 441 441 Inland 737 655 Asthma information provided by parents and doctors from 272, a total of 381 asthmatic students Intervention Comparison p valuea Number of sheets answered n=128/178 n=144/203 NS Symptoms Cough 97 111 NS Wheezing 68 88 NS Dyspnoea 67 89 NS Chest pain 20 28 NS Others 9 10 NS Triggers Common cold 68 78 NS Chalk dust 13 10 NS Strong odours 23 19 NS Weather changes 54 75 NS Exercise 38 36 NS Allergy (global) 98 113 NS Cat dander 31 37 NS Dog 24 30 NS Bird 0 0 Dust mites 56 62 NS Mould/Alternaria/humidity 28 35 NS Olive pollen 57 76 NS Grass pollen 45 62 NS Other pollen 7.4 16 NS Medication at school Need inhaler at school 114 124 NS Salbutamol 96 102 NS Terbutaline 18 22 NS Carries own inhaler 102 108 NS Teacher keeps inhaler 12 16 NS Self-administered inhaler 102 114 NS Needs help with inhaler 12 10 NS - 2.
Absenteeism rates were provided by the Regional Ministry of Education.
- 3.
Asthma Knowledge. We used the Newcastle asthma knowledge questionnaire (NAKQ)20 translated and validated in Spanish,21 self-administered by the students.
- 4.
Attitudes towards asthma. We used a self-administered questionnaire about attitudes concerning asthma with 15 items developed by Gibson et al.22 It includes four loci: “Tolerance towards asthma”, “Internal locus control” (degree to which a person believes that their own decisions and actions influence their illness), “external locus control” (degree to which an individual believes that their scope for action concerning asthma and its management is under the control of important external parties such as a doctor or teacher) and “Chance”, (belief that asthma and its effects are a result of chance.22 These were listed using a Likert scale. The highest score represents the strongest attitudes for the locus assessed.
Data from students with asthma:
- a.
Asthma-related quality of life. We used the Pediatric Asthma Quality of Life Questionnaire (PAQLQ)23 version with standardised activities, translated and validated in Spanish.24
- b.
Asthma Control in Children (in Spanish “Control Asma en Niños” or CAN). This includes nine items, with values from 0 to 4 (the higher the score, the worse the control). A score below 8 indicates well-controlled asthma; between 8 and 36 indicates uncontrolled asthma. We used the self-administered version.25
- c.
Asthma information. The child's parents and doctor indicated asthma symptoms, triggers and treatment to inform the teacher, with a coded copy for the study.
We performed an analysis by intention to treat, considering all those included in the intervention group, whether or not the children had attended educational programme.
To analyse the results and verify the research hypothesis, univariant and bivariate descriptive statistics were calculated, both quantitative (frequency tables, contingency tables, means, medians, typical deviations and percentages) as well as graphics (bars, box and whisker, sectors, histograms and dispersion).
For the inferential study, the corresponding confidence interval was calculated, as was the test for independent samples when the objective of the study was to research the equality of means or the distribution. T-student and ANOVA tests were performed in the case of assumed normality in the distribution of variables while non-parametric Mann–Whitney U or Kruskal–Wallis tests were applied in other cases. The Shapiro–Wilk test was used as well as graphic study, histograms, box-and-whisker plot to decide the most appropriate contrasts. In addition to providing the p-value obtained in the contrasts of means, we calculated the non-standardised measure of effect size. The corresponding log transformations for the variables were performed when necessary.
To compare the data obtained in the two phases of the study, we carried out parametric tests to study the equality of means for the related samples. In those cases in which a hypothesis of normality could not be assumed, a Wilcoxon signed-rank test or Friedman test was performed. To study possible associations between qualitative variables, Pearson's Chi-squared test and Fisher's exact test for 2×2 tables were performed.
To study the relationship between quantitative variables, regression, lineal, and non-lineal statistical techniques were applied to calculate and compare the corresponding goodness-of-fit coefficients (square R). For the more complex analysis of data, multiple lineal regression models were used, as were multi-level lineal models and multi-level logistic regression models when the dependent variables so demanded. Contrasts were made with an alpha significance level of=0.05. Intervals were calculated considering a 95% confidence level. We used SPPS Statistics V20 and STATA 13.
ResultsDuring the two phases of the study, we obtained paired data for each child from the 2169 students at the IS (94.6% of the initial number), of which 178 had asthma, and 2071 at the CS (93.5% of the initial number), of which 203 had asthma (Fig. 1). In general, the initial characteristics of the students were similar for IS and CS, both in terms of children with and without asthma (Table 1).
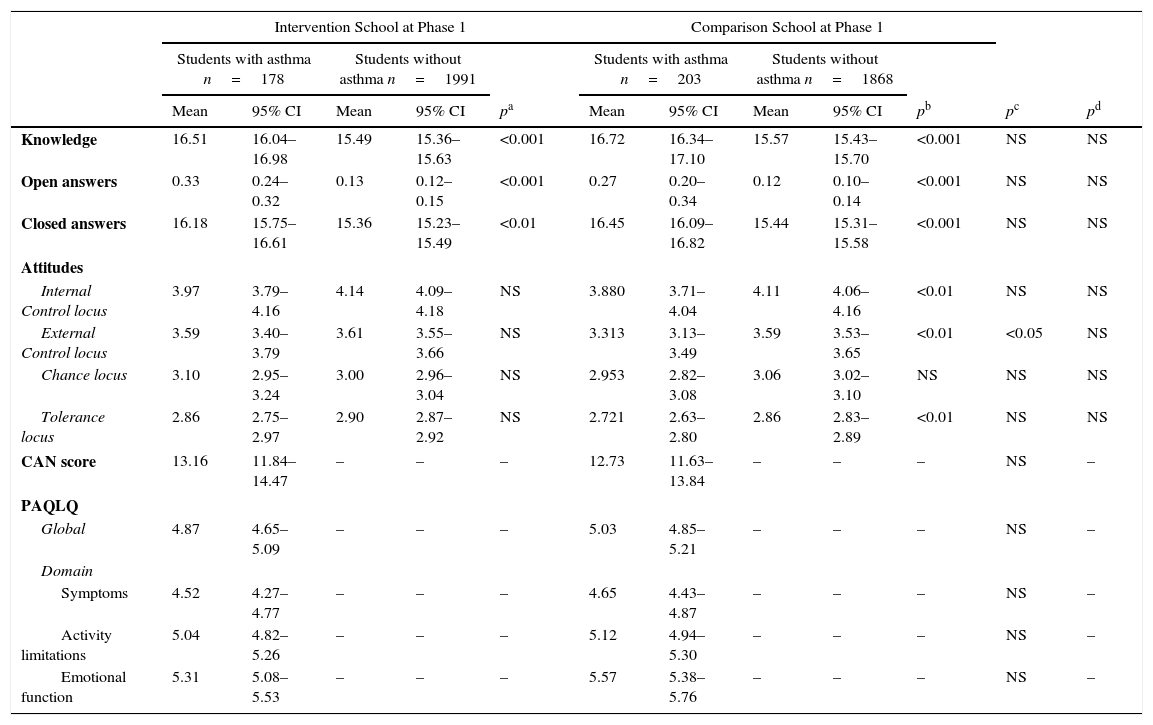
Asthma quality of lifePAQLQ scores and its domains prior to (Phase 1) and after the programme (Phase 2) are shown in Tables 2 and 3, respectively. There are no differences between IS and CS in both phases. The analysis of the matched samples for both phases of the study appears in Table 4. The score for global quality of life and the domain of symptoms increases significantly, in both IS and in CS. The scores in the domains for emotional function and activity limitations only increased in IS schools.
Results of knowledge questionnaires, attitudes about asthma of all students and Paediatric Asthma Quality of Life Questionnaire (PAQLQ), with detail of dimensions and Asthma Control (CAN) for students with asthma in Phase 1 of the study (prior to educational course).
| Intervention School at Phase 1 | Comparison School at Phase 1 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Students with asthma n=178 | Students without asthma n=1991 | Students with asthma n=203 | Students without asthma n=1868 | |||||||||
| Mean | 95% CI | Mean | 95% CI | pa | Mean | 95% CI | Mean | 95% CI | pb | pc | pd | |
| Knowledge | 16.51 | 16.04–16.98 | 15.49 | 15.36–15.63 | <0.001 | 16.72 | 16.34–17.10 | 15.57 | 15.43–15.70 | <0.001 | NS | NS |
| Open answers | 0.33 | 0.24–0.32 | 0.13 | 0.12–0.15 | <0.001 | 0.27 | 0.20–0.34 | 0.12 | 0.10–0.14 | <0.001 | NS | NS |
| Closed answers | 16.18 | 15.75–16.61 | 15.36 | 15.23–15.49 | <0.01 | 16.45 | 16.09–16.82 | 15.44 | 15.31–15.58 | <0.001 | NS | NS |
| Attitudes | ||||||||||||
| Internal Control locus | 3.97 | 3.79–4.16 | 4.14 | 4.09–4.18 | NS | 3.880 | 3.71–4.04 | 4.11 | 4.06–4.16 | <0.01 | NS | NS |
| External Control locus | 3.59 | 3.40–3.79 | 3.61 | 3.55–3.66 | NS | 3.313 | 3.13–3.49 | 3.59 | 3.53–3.65 | <0.01 | <0.05 | NS |
| Chance locus | 3.10 | 2.95–3.24 | 3.00 | 2.96–3.04 | NS | 2.953 | 2.82–3.08 | 3.06 | 3.02–3.10 | NS | NS | NS |
| Tolerance locus | 2.86 | 2.75–2.97 | 2.90 | 2.87–2.92 | NS | 2.721 | 2.63–2.80 | 2.86 | 2.83–2.89 | <0.01 | NS | NS |
| CAN score | 13.16 | 11.84–14.47 | – | – | – | 12.73 | 11.63–13.84 | – | – | – | NS | – |
| PAQLQ | ||||||||||||
| Global | 4.87 | 4.65–5.09 | – | – | – | 5.03 | 4.85–5.21 | – | – | – | NS | – |
| Domain | ||||||||||||
| Symptoms | 4.52 | 4.27–4.77 | – | – | – | 4.65 | 4.43–4.87 | – | – | – | NS | – |
| Activity limitations | 5.04 | 4.82–5.26 | – | – | – | 5.12 | 4.94–5.30 | – | – | – | NS | – |
| Emotional function | 5.31 | 5.08–5.53 | – | – | – | 5.57 | 5.38–5.76 | – | – | – | NS | – |
NS: p≥0.05.
pa Comparison for students with asthma and without asthma in the Intervention School.
pb Comparison for students with asthma and without asthma in the Comparison School.
pc Comparison for students with asthma between Intervention and Comparison Schools.
pd Comparison for students without asthma between Intervention and Comparison Schools.
Results of knowledge questionnaires, attitudes about asthma of all students and quality of life questionnaire (with detail of dimensions) and control of asthma (CAN) for students with asthma in Phase 2 of the study (after to educational course).
| Intervention School at Phase 2 | Comparison School at Phase 2 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Students with asthma n=178 | Students without asthma n=1991 | Students with asthma n=203 | Students without asthma n=1868 | |||||||||
| Mean | 95% CI | Mean | 95% CI | pa | Mean | 95% CI | Mean | 95% CI | pb | pc | pd | |
| Knowledge | 18.16 | 17.69–18.62 | 17.50 | 17.36–17.64 | <0.01 | 17.07 | 16.99–17.45 | 15.75 | 15.62–15.89 | <0.001 | <0.001 | <0.001 |
| Open answers | 0.60 | 0.49–0.70 | 0.59 | 0.56–0.62 | NS | 0.32 | 0.24–0.40 | 0.19 | 0.17–0.21 | <0.001 | <0.001 | <0.001 |
| Closed answers | 17.56 | 17.13–17.99 | 16.91 | 16.78–17.04 | <0.01 | 16.75 | 16.39–17.10 | 15.56 | 15.43–5.69 | <0.001 | <0.01 | <0.001 |
| Attitudes | ||||||||||||
| Internal Control locus | 4.23 | 4.07–4.39 | 4.33 | 4.29–4.38 | NS | 3.79 | 3.64–3.95 | 4.03 | 3.98–4.08 | <0.01 | <0.001 | <0.001 |
| External Control locus | 3.43 | 3.22–3.63 | 3.54 | 3.49–3.60 | NS | 3.14 | 2.97–3.30 | 3.37 | 3.31–3.43 | <0.05 | <0.05 | <0.001 |
| Chance locus | 2.94 | 2.79–3.09 | 2.90 | 2.85–2.94 | NS | 3.04 | 2.92–3.16 | 2.94 | 2.90–2.98 | NS | NS | NS |
| Tolerance locus | 2.74 | 2.66–2.83 | 2.80 | 2.77–2.83 | NS | 2.69 | 2.61–2.77 | 2.78 | 2.75–2.80 | NS | NS | NS |
| CAN score | 11.25 | 9.93–12.57 | – | – | – | 10.61 | 9.43–11.78 | – | – | – | NS | – |
| PAQLQ | ||||||||||||
| Global | 5.29 | 5.09–5.50 | – | – | – | 5.30 | 5.11–5.48 | – | – | – | NS | – |
| Domain | ||||||||||||
| Symptoms | 5.03 | 4.79–5.27 | – | – | – | 5.08 | 4.87–5.29 | – | – | – | NS | – |
| Activity limitations | 5.33 | 5.14–5.53 | – | – | – | 5.27 | 5.08–5.46 | – | – | – | NS | – |
| Emotional Function | 5.72 | 5.51–5.93 | – | – | – | 5.71 | 5.52–5.89 | – | – | – | NS | – |
NS: p≥0.05.
pa Comparison for students with asthma and without asthma in the Intervention School.
pb Comparison for students with asthma and without asthma in the Comparison School.
pc Comparison for students with asthma between Intervention and Comparison Schools.
pd Comparison for students without asthma between Intervention and Comparison Schools.
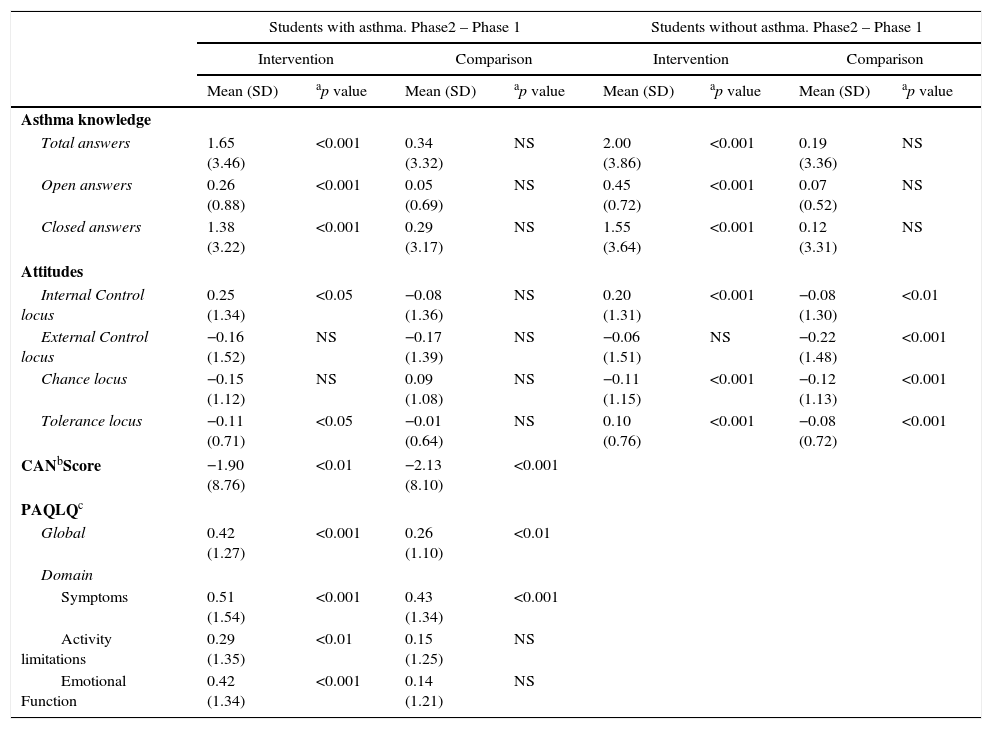
Study of related samples. Differences of the changes for each child in the variables studied, between Intervention and Comparison Schools in two phases of the study.
| Students with asthma. Phase2 – Phase 1 | Students without asthma. Phase2 – Phase 1 | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Comparison | Intervention | Comparison | |||||
| Mean (SD) | ap value | Mean (SD) | ap value | Mean (SD) | ap value | Mean (SD) | ap value | |
| Asthma knowledge | ||||||||
| Total answers | 1.65 (3.46) | <0.001 | 0.34 (3.32) | NS | 2.00 (3.86) | <0.001 | 0.19 (3.36) | NS |
| Open answers | 0.26 (0.88) | <0.001 | 0.05 (0.69) | NS | 0.45 (0.72) | <0.001 | 0.07 (0.52) | NS |
| Closed answers | 1.38 (3.22) | <0.001 | 0.29 (3.17) | NS | 1.55 (3.64) | <0.001 | 0.12 (3.31) | NS |
| Attitudes | ||||||||
| Internal Control locus | 0.25 (1.34) | <0.05 | −0.08 (1.36) | NS | 0.20 (1.31) | <0.001 | −0.08 (1.30) | <0.01 |
| External Control locus | −0.16 (1.52) | NS | −0.17 (1.39) | NS | −0.06 (1.51) | NS | −0.22 (1.48) | <0.001 |
| Chance locus | −0.15 (1.12) | NS | 0.09 (1.08) | NS | −0.11 (1.15) | <0.001 | −0.12 (1.13) | <0.001 |
| Tolerance locus | −0.11 (0.71) | <0.05 | −0.01 (0.64) | NS | 0.10 (0.76) | <0.001 | −0.08 (0.72) | <0.001 |
| CANbScore | −1.90 (8.76) | <0.01 | −2.13 (8.10) | <0.001 | ||||
| PAQLQc | ||||||||
| Global | 0.42 (1.27) | <0.001 | 0.26 (1.10) | <0.01 | ||||
| Domain | ||||||||
| Symptoms | 0.51 (1.54) | <0.001 | 0.43 (1.34) | <0.001 | ||||
| Activity limitations | 0.29 (1.35) | <0.01 | 0.15 (1.25) | NS | ||||
| Emotional Function | 0.42 (1.34) | <0.001 | 0.14 (1.21) | NS | ||||
SD=standard deviation.
Table 2 shows the scores obtained for CAN in Phase 1; Table 3 shows the data for Phase 2. No differences in the score for CAN were seen between IS and CS in both phases. The study of matched samples is provided in Table 4. The scores for CAN improved significantly both in IS as in CS.
School absenteeismThe intervention programme decreases absenteeism in IS in comparison with CS, without reaching significance.
Asthma knowledgeTable 2 shows asthma knowledge in Phase 1 and Table 3 for Phase 2. The asthmatic children had a significantly higher score than non-asthmatic children in both IS and CS. The study of matched samples for the variable “differences” is shown in Table 4. Knowledge improved significantly only for IS.
Attitudes towards asthmaAttitudes towards asthma, in its four loci, are shown for Phase 1 in Table 2 and for Phase 2 in Table 3. Table 4 shows the matched samples analysis.
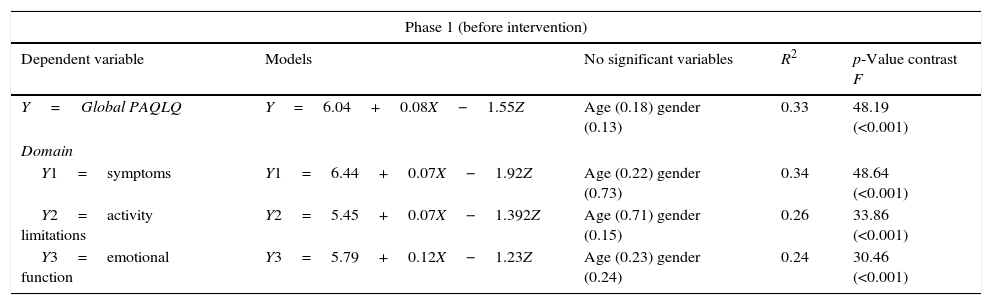
Relationship among variablesIn the multi-level lineal regression analysis, quality of life and its domains were considered the dependent variable, as first level variables, the score for knowledge, age, gender and control of asthma. Second level variables were the groups based on geographical location. No null model obtained significant results, with the resulting values for the interclass correlation (ICC) being insufficient (ICC for mountain/coast/inland=0.005, ICC for rural/urban=2.91e−10, ICC for provinces=5.76e−13, ICC for municipality 0.025), and for the second level variable to be explicative for a significant part of the quality of life variability. Better results were not obtained for other dependent domain symptoms variables, the activity limitation domain and emotional function domain.
We performed a multiple regression analysis, with the dependent variables being quality of life and their three domains symptoms, activity limitation and emotional function. Gender, age, score for asthma knowledge and the variable factor indicating whether or not the child had controlled asthma (CAN<7 points) were used as independent variables. Children without controlled asthma (CAN>7 points) were considered the reference category (Table 5).
Multiple regression models.
| Phase 1 (before intervention) | ||||
|---|---|---|---|---|
| Dependent variable | Models | No significant variables | R2 | p-Value contrast F |
| Y=Global PAQLQ | Y=6.04+0.08X−1.55Z | Age (0.18) gender (0.13) | 0.33 | 48.19 (<0.001) |
| Domain | ||||
| Y1=symptoms | Y1=6.44+0.07X−1.92Z | Age (0.22) gender (0.73) | 0.34 | 48.64 (<0.001) |
| Y2=activity limitations | Y2=5.45+0.07X−1.392Z | Age (0.71) gender (0.15) | 0.26 | 33.86 (<0.001) |
| Y3=emotional function | Y3=5.79+0.12X−1.23Z | Age (0.23) gender (0.24) | 0.24 | 30.46 (<0.001) |
| Phase 2 (after intervention) | ||||
|---|---|---|---|---|
| Dependent variable | Models | No significant variables | R2 | p-Value contrast F |
| Y=Global PAQLQ | Y=5.12+0.09X−1.56Z | Age (0.526) gender (0.79) | 0.37 | 56.15 (<0.001) |
| Domain | ||||
| Y1=symptoms | Y1=5.59+0.07X−1.89Z | Age (0.605) gender (0.35) | 0.37 | 57.21 (<0.001) |
| Y2=activity limitations | Y2=5.32+0.09X−1.34Z | Age (0.389) gender (0.66) | 0.28 | 37.34 (<0.001) |
| Y3=emotional function | Y3=4.30+0.12X−1.29Z | Age (0.950) gender (0.52) | 0.29 | 38.70 (<0.001) |
The variable Z indicates controlled-asthma (Z=0) or uncontrolled-asthma (Z=1). CAN>7=uncontrolled-asthma.
In the multiple lineal regression models, the quality of life for children with asthma that was not controlled lowered 1.5 points over the quality of life for children with controlled asthma. Upon seeing these results for the two phases, high stability was seen in the models calculated. A higher score for quality of life and its domains is linked to the score for knowledge about asthma and controlled asthma. The score for the emotional function domain depends, to a greater extent, on knowledge about asthma.
Additionally, we found a high lineal relationship (R2=0.559) between CAN and PAQLQ and its domains: “symptoms” R2=0.59, “limited activities” R2=0.375 and “emotional function” R2=0.408. This relationship was greater in girls R2=0.586 than in boys R2=0.534. Pearson's lineal correlation coefficient between CAN and PAQLQ for boys was r=−0.73 and r=−0.77 for girls. We found no relationship for knowledge, attitudes towards asthma and school absenteeism with regards to Quality of Life.
DiscussionWe conducted an educational programme about asthma among grade school students, applying a train-the-trainer strategy, using school doctors without specific asthma preparation to train PE teachers in the ASAH Programme. This is the first study about quality of life regarding asthma in a grade school population in Spain, followed longitudinally throughout the school year. The programme improved the quality of life, both globally as well as the domains making it up, while at the same time improving asthma knowledge in all students, especially those with asthma.
Asthma-related quality of life measured with PAQLQ is lower than that of a group of uncontrolled asthma patients found in Spain's hospitals and used to validate the Spanish-language version of the PAQLQ24 but similar to a study carried out in high school education in Australia.10 In a recent study with older students, PAQLQ was significantly greater than this current study, which is in keeping with the ISAAC study, where, in recent years, asthma is worse among younger children.2,26
We found a significant improvement between the two phases of the study in terms of the scores for CAN (asthma control) and global PAQLQ for IS and CS; no significant differences were found between IS and CS. Probably, this is due to seasonal environmental changes when the questionnaires were fill out.27,28 There are other aspects such as learning self-management of asthma, psycho-social factors such as quality of life of the parents,29 and avoidance of triggers that have a greater influence on asthma control and the children's quality of life.11,30
Although quality of life is related to controlling asthma, there are other psycho-social factors that influence this relationship.31,32 Such factors are not dependent solely upon pulmonary function and symptoms, especially in the case of mild-moderate asthma.33 In our study, the domains “activity limitations” and “emotional function” for quality of life changed significantly in the analysis for matched samples, but only in IS. The education received by children with asthma and their classmates could have influenced to improve “emotional function” and “activity limitation” domains which are more related to feelings and the life experiences of asthmatic children.
Henry10 detected significant changes in the PAQLQ, only for IS; this was not clinically relevant as 0.5 improvement points were not obtained. In our study, the percentage of students with improvements on the PAQLQ translated into relevant clinical changes being greater among IS, but these were not statistically significant when compared with CS.
The programme did not alter the number of absentees at IS when compared to CS. It is possible that this may be due to the limited intervention with students. Other authors included the students’ parents in their programme and encountered improvement in school absenteeism.34
Students’ knowledge increased significantly in the IS in comparison with the CS. The knowledge differences between children with and without asthma were maintained; this indicated the effectiveness of the programme for all those involved. Specific education at school significantly improves the knowledge of students with9–11 and without asthma,10 but we do not know whether it influenced asthma management in students with asthma, given that this was not the objective of this study. Nevertheless, the programme significantly increased the score for the “internal control” locus in children with asthma; this attributes greater responsibility in controlling one's own asthma. Likewise, it decreased the “external control” locus, which attributes the responsibility of caring for the person with asthma to others (i.e. doctors, parents or teachers). These beliefs are essential for asthma patients to accept their own care.10 Children with asthma in the CS did not vary their response between the two phases of the study. The differences found in attitudes towards asthma among children without asthma in both groups were interpreted as random responses.
The strength of our study lies in the large sample size, the limited losses between the two phases of the study, and maintaining a blind study by using a coding system. The information that parents provided about their child's asthma could have a positive influence on students with asthma, but this aspect was not assessed. Communication is essential to optimise asthma management at school, especially in high risk districts.35
Our study has used a train-the-trainer strategy, successfully tested by certified trainer programmes36 using professional resources from our own educational field. Thanks to school doctors, we reached a greater number of students, while empowering the teachers participating in the experience. Changes in asthma knowledge, attitudes about and management of asthma among the participating teachers have yet to be assessed.
Limitations of the studyOur study has several limitations. These include its generalisation—it was for the last two years of grade school—and training included no self-management based on daily symptoms or peak-flow metre. Although 72 schools refused to participate, this need not be considered a limitation for generalisation, since randomisation was carried out after the invitation was presented and there were no differences in the school size or their geographical location. Another possible limitation is that the ASAH Programme was for all children, with or without asthma, which could mitigate the intensity of the education in children with asthma. Other health results linked to quality of life and asthma control have not been tested, including the quantification of daytime and night-time symptoms, use of beta-2-adrenergic for relief, pulmonary function and the use of preventive medication.24
ConclusionsThe ASAH Programme has improved knowledge and attitudes towards asthma in students. It has improved quality of life, especially certain aspects such as “emotional function” and “limitation of activities” but without reducing their school absenteeism. Our educational programme could be taught by PE teachers to obtain positive asthma results at school.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the subjects’ parents mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
FundingGrant PI10/01244 from Healthcare Research Project: Instituto de Salud Carlos III; Ministry of Education and Competitiveness, Government of Spain, and ERFD (European Regional Development Fund), European Union.
Grant PI-0177-2010 from Andalusian Regional Government Ministry of Health and ERFD (European Regional Development Fund), European Union.
Potential Conflict of interestThe authors have indicated they have no potential conflicts of interest to disclose.
We greatly appreciate the help provided by the school doctors listed below. They willingly volunteered to participate in this project. Without their help, this work would have been impossible.
Antonia Acosta-Delgado, Mariano Andújar-Mejías, Susana de la Guerra-Irazu, Antonio Miguel Fernández-Rivas, Rafael Gamero-García, Rafael Hernández-Izquierdo, Teodoro Izquierdo, Antonio Ladrero-Madrid, Dolores Martínez-Travé, Marcial Medina-Ceballos, Ana María Montes-Domínguez, Ana María Morilla-García, Antonio Abad Olmedo-Fernández, Rafael Pineda-Lucena, Mario Rodríguez-Burgos, José Santos-Luna, Antonio Sotomayor and Fernando Vega-Toro.