Asthma exacerbations attended in emergency departments show a marked seasonality in the paediatric age. This seasonal pattern can change from one population to another and the factors involved are poorly understood.
ObjectivesTo evaluate the association between meteorological factors and schooling with asthma exacerbations in children attended in the paediatric emergency department of a district hospital.
MethodsWe conducted a retrospective review of the medical records of children 5–14 years of age attended for asthma exacerbations during a 4-year period (2007–2011). Climatic data were obtained from a weather station located very close to the population studied. The number of asthma exacerbations was correlated to temperature, barometric pressure, relative humidity, rainfall, wind speed, wind distance, solar radiation, water vapour pressure and schooling, using regression analyses.
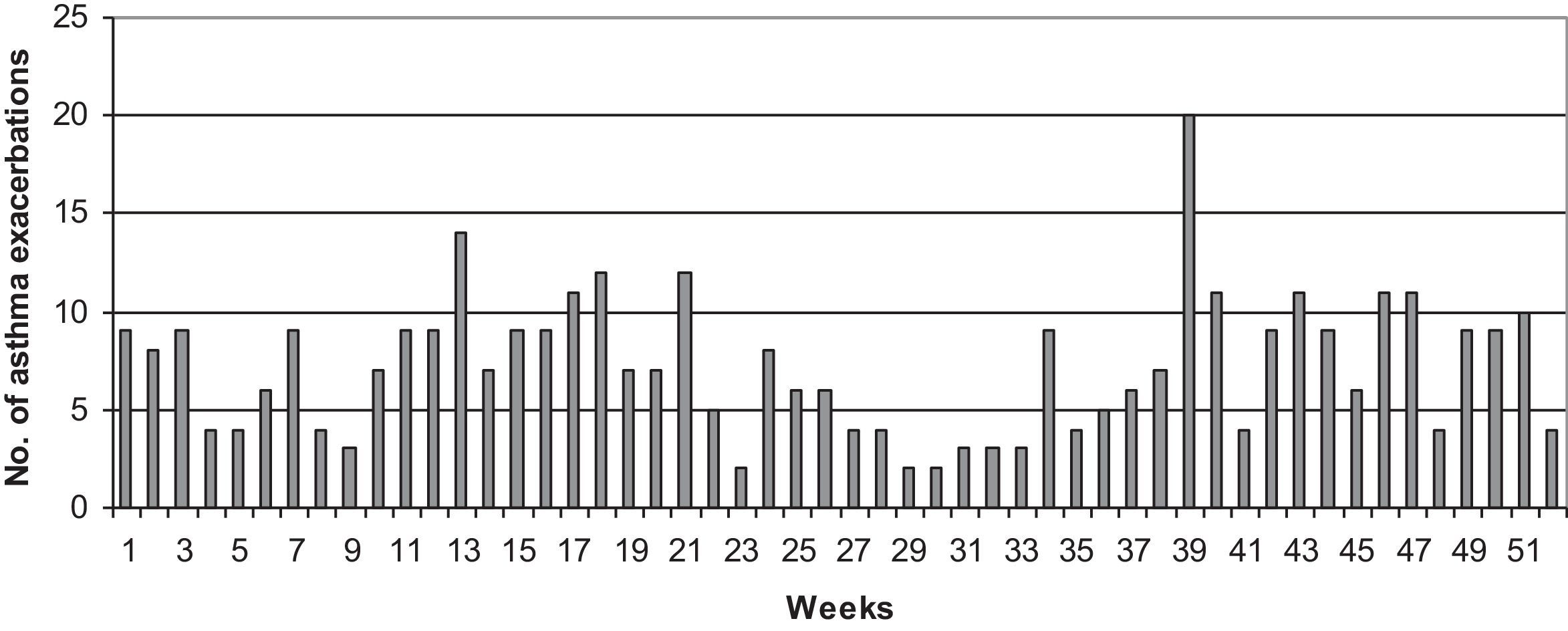
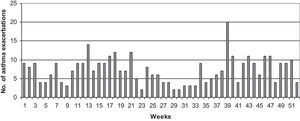
ResultsDuring the study period, 371 children were attended for asthma exacerbations; median age was eight years (IQR: 6–11), and 59% were males. Asthma exacerbations showed a bimodal pattern with peaks in spring and summer. Maximum annual peak occurred in week 39, within 15 days from school beginning after the summer holidays. A regression model with mean temperature, water vapour pressure, relative humidity, maximum wind speed and schooling could explain 98.4% (p<0.001) of monthly asthma exacerbations.
ConclusionsThe combination of meteorological factors and schooling could predict asthma exacerbations in children attended in a paediatric emergency department.
Asthma is the most prevalent chronic disease in childhood and an important cause of visits to the emergency department (ED).1 Seasonal exacerbation of asthma is a well-known phenomenon especially in children. Johnston and Sears2,3 studying hospitalisations and ED visits for asthma in Canada found that asthma exacerbations followed a cyclic pattern in school-age children 5–15 years. There was a minor increase through the first six months of the year, then declined during the summer and peaked in September about two weeks after school return from the summer holidays. The patterns in the distribution of asthma exacerbations may be explained by a combination of geographical differences in allergen sensitisation, pollution levels, viral exposure and/or weather conditions. In general, understanding the determinants of asthma exacerbation is poor because of the difficulty in determining exposure to causal factors and the complexity of the interactions between them.4
There are not many reports on the association between asthma attacks and specific weather conditions.5–19 Relative humidity, mean temperature, rainfall, wind speed, sunshine and barometric pressure have been evaluated as a cause of asthma exacerbations in children. However, it is not clear whether climatic factors affect asthma exacerbations directly or indirectly through their effect on other environmental agents. To date, no model based on climatic factors has been able to accurately predict exacerbations of asthma. The aim of this study was to determine the epidemiology of asthma exacerbations in the children attended in a paediatric ED. We evaluated the association of these exacerbations with some meteorological factors and school attendance.
Materials and methodsStudy populationThe study was conducted in the paediatric ED of a district hospital on the island of Mallorca, Spain. From July 1, 2007, to June 30, 2011, the medical records of children 5–14 years of age visited at the ED with a diagnosis of asthma exacerbation were retrospectively reviewed. Diagnosis, age, sex, and date of admission of all children attended were codified prior to their discharge and these data were automatically stored in a computerised database. Subjects were selected from this database after revision of the hospital discharge codes with a primary or secondary diagnosis of asthma exacerbation. The episodes of asthma exacerbation were identified via the International Classification of Diseases, 9th revision, with 493.0-9 discharge codes.
Meteorological dataDuring the study period, data on barometric pressure, humidity, wind speed, wind distance, rainfall, global solar radiation and temperature were obtained from the Spanish Meteorology Agency. This agency collects daily information from a weather station located close by at latitude 39.55°N, longitude 2.73°E and 4m height. Water vapour pressure was obtained using an equation described elsewhere.20
Data analysisDescriptive analysis was performed using frequency distributions or rates. All continuous variables were confirmed to be normally distributed, or to have skewness not significantly different from zero. Results are presented as mean±standard deviation (SD) or median and interquartile (IQR) as required. Co-linearity was studied performing tolerance testing. For analyses, variables were paired throughout the 12 months of the year; the meteorological data were the mean of the different monthly means, and asthma exacerbations was the sum of admissions in the ED for this reason during the months of the year. The association between asthma exacerbations and the meteorological variables was determined after multivariate linear regression. Backward elimination method was used for variable selection. The effect of two lag months period was also evaluated. The effect of a unit increase for each independent variable was calculated transforming the ¿i coefficients into percentages ([¿i/N° asthma exacerbations]×100). To determine the effect of school attendance we considered that one or more weeks of school holidays during a month period could be considered a relevant decrease in schooling. In consequence, a dummy variable that defined schooling as the absence of this holiday period was introduced in the multivariate analyses. Statistical significance was set at p<0.05. Data were analysed with the statistical software package IBM SPSS 20.0 (New York, USA).
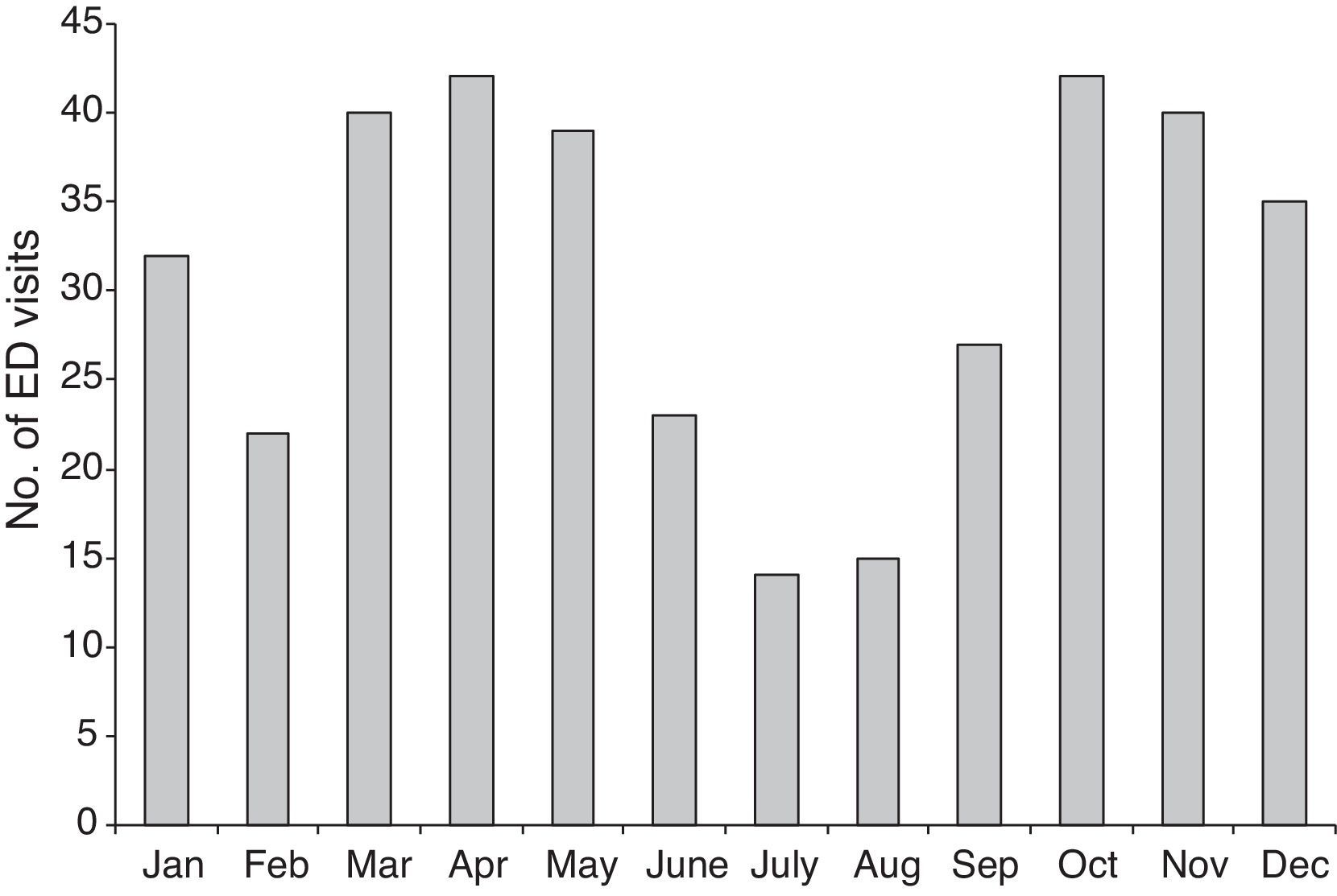
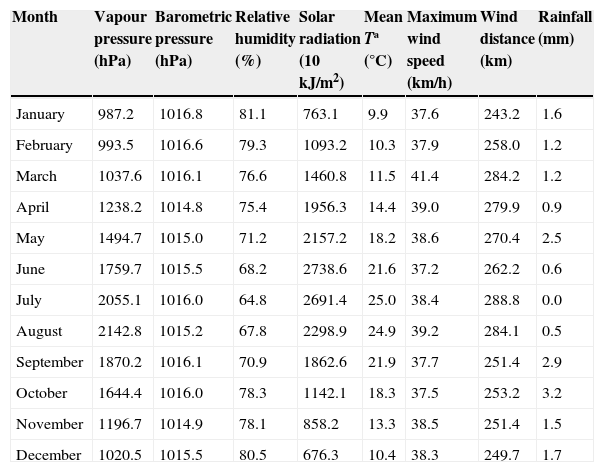
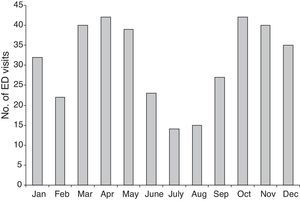
ResultsGeneral characteristics and seasonalityFrom July 1, 2007, through June 30, 2011, 371 children aged 5–14 years were attended at the ED for asthma exacerbation. This accounted for 7.9% of the attended children of this age group in the paediatric ED. The median age was eight years (IQR: 6–11), and 59% were males. The monthly distribution of the children attended for asthma is shown in Fig. 1. Monthly asthma exacerbations showed a bimodal distribution with two annual peaks, one in spring and the other in autumn. Table 1 shows the monthly variation of the meteorological variables.
Mean monthly levels of studied meteorological factors.
| Month | Vapour pressure (hPa) | Barometric pressure (hPa) | Relative humidity (%) | Solar radiation (10kJ/m2) | Mean Tª (°C) | Maximum wind speed (km/h) | Wind distance (km) | Rainfall (mm) |
|---|---|---|---|---|---|---|---|---|
| January | 987.2 | 1016.8 | 81.1 | 763.1 | 9.9 | 37.6 | 243.2 | 1.6 |
| February | 993.5 | 1016.6 | 79.3 | 1093.2 | 10.3 | 37.9 | 258.0 | 1.2 |
| March | 1037.6 | 1016.1 | 76.6 | 1460.8 | 11.5 | 41.4 | 284.2 | 1.2 |
| April | 1238.2 | 1014.8 | 75.4 | 1956.3 | 14.4 | 39.0 | 279.9 | 0.9 |
| May | 1494.7 | 1015.0 | 71.2 | 2157.2 | 18.2 | 38.6 | 270.4 | 2.5 |
| June | 1759.7 | 1015.5 | 68.2 | 2738.6 | 21.6 | 37.2 | 262.2 | 0.6 |
| July | 2055.1 | 1016.0 | 64.8 | 2691.4 | 25.0 | 38.4 | 288.8 | 0.0 |
| August | 2142.8 | 1015.2 | 67.8 | 2298.9 | 24.9 | 39.2 | 284.1 | 0.5 |
| September | 1870.2 | 1016.1 | 70.9 | 1862.6 | 21.9 | 37.7 | 251.4 | 2.9 |
| October | 1644.4 | 1016.0 | 78.3 | 1142.1 | 18.3 | 37.5 | 253.2 | 3.2 |
| November | 1196.7 | 1014.9 | 78.1 | 858.2 | 13.3 | 38.5 | 251.4 | 1.5 |
| December | 1020.5 | 1015.5 | 80.5 | 676.3 | 10.4 | 38.3 | 249.7 | 1.7 |
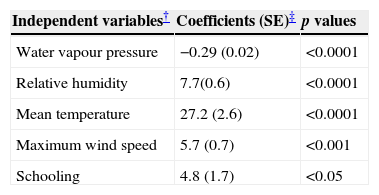
After multivariate analyses asthma exacerbation was independently associated to several meteorological variables: mean temperature, water vapour pressure, relative humidity and maximum wind speed (see Table 2). The resulting model (including schooling) was able to explain 98.4% of the variability of monthly asthma exacerbations during the study period. The regression equation showed a 7.3% increase in the number of monthly asthma exacerbations for each degree decrease in temperature; and 1.5% and 2.1% increase for each unit rise in wind speed and relative humidity, respectively. A 100hPa increase in water vapour pressure decreased the number of asthma exacerbations by 7.8%. The use of one and two lag months did not provide better models.
Association with school attendancePeak asthma exacerbations occurred 15 days after school return from the summer holidays (week 39 of the year). The number of attended asthma exacerbations decreased the following week but maintained at a high rate for several months with scarce variations (see Fig. 2). Multivariate analysis showed that school attendance was also an independent variable associated to asthma exacerbations.
DiscussionAsthma exacerbations show a seasonal variability in adults and children in both hemispheres, with grade school children being the most vulnerable to seasonal changes.21,22 In our study, we observed a bimodal seasonal pattern of asthma exacerbations with peaks in April and October, similar to those described in Tokyo (Japan) and Ontario (Canada).14,15 Studies that have evaluated the association between meteorological factors and asthma exacerbations in the ED are limited and have obtained disparate results. They differ in the meteorological variables associated, their positive or negative correlation and/or the strength of the association. The resulting models of the reported studies on meteorological factors and exacerbation of asthma have shown low predictive power (R2<0.4).7–9,17 In our study, we observed an association between asthma exacerbation, measured by the rates of ED visits for asthma, and several meteorological variables such as mean temperature, water vapour pressure, relative humidity and maximum wind speed. This model has given a very high predictive power (R2=0.98), making it very useful for forecasting.
We observed that mean temperature was inversely correlated with ED visits for asthma, which is consistent with other studies that showed a weaker correlation.7,17 However, this variable has given contradictory results in some reports. Mohr et al.23 reported a positive association with ED visits for asthma in summer and negative during the winter time. Hashimoto et al.14 observed a positive association for mean temperature but inverse for maximum average temperature. In addition, other studies have found a weak positive correlation.18 It is likely that these results are not mutually exclusive, and that the association between temperature and asthma exacerbations in the ED depends on the aetiological trigger; probably negative with respiratory viruses,24 and positive in the case of air pollutants and pollens.18,25,26
In our study, asthma exacerbations in the ED were associated to a decrease in the water vapour pressure and to an increase in relative humidity. The association between vapour pressure and asthma exacerbations has not been previously studied, but several studies have reported a relationship between this variable and respiratory viruses (respiratory syncytial virus and influenza), which are believed to trigger asthma exacerbations.20,24 Similarly, increased relative humidity has been correlated in some studies to an increase in viral activity and mite concentration.27,28 In our study, for each one percent increase in relative humidity there was a 1.8% increase in asthma attacks, as also described by others.17
Overall, the association of asthma attacks with temperature, vapour pressure and humidity is in agreement with the increasing evidence of the role of viral respiratory infections as important triggers of asthma exacerbations, especially serotype C human rhinovirus.29 A recent study performed in Madrid (Spain) evaluated the seasonal distribution of rhinovirus C infections in children.30 We compared their data with our monthly incidence of asthma attacks, observing a good correlation (r=0.61, p<0.05; data not shown). Despite the limitations of comparing populations with environmental and weather differences, this correlation suggests that the asthma exacerbations in our study could also be caused by rhinovirus infections in certain periods of the year.
The maximum wind speed was another independent factor that we found associated to asthma exacerbations. Until now, reports correlating this meteorological factor to viral infections and/or asthma exacerbations have been anecdotal.15,28 In our study, the correlation was more marked during the spring time. An increase in wind speed during this season could favour a higher concentration, transport and/or exposure to pollen grains. In a similar way, wind speed favours higher concentrations of asthma-related air pollutants such as low weight particle matter (e.g. PM10).31 However, we did not observe an association with rainfall or barometric pressure, which have been related to the concentration of air pollutants.15,16 The absence of association between these two variables and asthma exacerbations in our study points to a scarce influence of pollutants as asthma triggers in our population.
Meteorological factors could also play a direct role as triggers of asthma exacerbations, as occurs with bronchoconstriction due to low air temperature or exercise-induced asthma in low humidity conditions. However, the real impact of the direct effect of climatic factors on asthma exacerbations requiring an ED visit remains unknown.32 A study performed in Ottawa (Canada), evaluating the association with asthma ED visits in an hourly time scale, suggested that the direct role of meteorological factors was scarce.15
Finally, we evaluated the effect of schooling to see if this variable acted as a confounding factor due to seasonal overlapping with meteorological factors. Schooling was an independent variable that increased the monthly risk of asthma attacks. Previous studies have analysed the effect of schooling especially after the summer holidays. We observed that the highest asthma exacerbation peak occurred 15 days after the beginning of school in September. This is in accordance with the 10–18 days lag from school opening previously described.22,33,34 As has been suggested, the “September epidemic” coinciding with school opening is probably due to various factors such as a favourable weather, increase of viral proliferation and exposure (especially rhinovirus), stress, and low compliance of inhaled corticosteroid therapy during the summer.3,35
The present report is an ecological retrospective study with the limitations of this type of study. We are aware that our results cannot be extrapolated to other populations with different sociodemographic, environmental, and climatic characteristics. Despite these limitations, we have shown that meteorological factors and schooling can efficiently forecast the asthma exacerbations that need to visit the ED. This could have potential implications for the organisation of health resources, prevention and etiological study of asthma.
Ethical disclosuresProtection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
Patients’ data protectionThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no funding or conflicts of interest to disclose.