Allergy is determined by genetic and environmental factors. People immigrating from under-developed to industrialised countries are at higher risk of developing allergic diseases and immigration is as a good epidemiological model to quantify the influence of the environment.
We performed the allergological assessment of 32,555 recent immigrants from different areas of the world to a polluted metropolitan area of Northern Italy.
MethodsWe evaluated time of onset of allergic rhinitis and/or asthma, sensitisations and clinical characteristics of 395 subjects (3.74 ± 2.94 yrs, mean ± SD) from four macro-areas (Asia, Africa, East-Europe, South America) arriving to Milan, Italy from June 2005 to June 2009. Data were compared with immigrants having access to the same medical facility for any medical problem and with resident Italians living in the same area.
ResultsImmigrants with allergic rhinitis and/or asthma days since arrival in Italy correlated with number of sensitisations (p=0.0030). Moreover, personal (2.02%) or familial (2.78%) history of allergic diseases was lower in allergic immigrants as compared to allergic residents (37.77 and 29.39%, respectively; p<0.0001 for both comparisons). Finally, the frequency of allergic immigrants from South America (63.3%) was higher than expected from the overall proportion of individuals from this macro-area who sought medical help at the same facility (40.4%; p<0.0001, OR 2.289, CI 2.1670–3.255).
ConclusionsEnvironmental factors play a relevant role in the induction of allergies in immigrants to Northern Italy. Genetics appears as a further promoting factor in the case of immigrants from South America.
Allergy is determined by the effect of genetic and environmental factors1 and by their interaction. Recent advances in the genetic characterisation of the atopic phenotype are still missing the final goal, i.e., the prediction of the risk of allergy of single individuals with a defined genetic profile, when exposed to a given environmental challenge.2 Although maternal factors, feeding, infections and exposure to allergens are certainly involved in this complex interplay,3–5 a positive family history for atopy remains a strong predictor for the development of allergy.6
In the last two decades, the phenomenon of massive immigration to affluent European countries of people from non-industrialised areas of the world represents an experiment of nature to test the relative weight of environment versus genetics in the establishment of allergies in different populations.
One of us (AMV) is currently responsible for the medical facility of a Non-Governmental Organisation operating in Italy since 1959, which provides help at no cost to the poorest in the Milan metropolitan area (Opera San Francesco, (OSF)). The medical outpatient facility of OSF is organised in sections corresponding to the most relevant medical specialities, including Allergology and Clinical Immunology, and provided over 33,000 visits in calendar year 2008. The first visit of any applicant for medical care to OSF is made by one general practitioner, who subsequently re-directs patients to the competent specialist, if required. Each access is recorded in a database which is also used by medical personnel for the follow-up of the clinical interventions provided to patients. In Italy, the Public Health System (PHS) provides extensive medical assistance to residents, whereas immigrants can access it only for emergency problems, or for problems of special social impact (e.g., some infectious diseases at risk of spreading). Only when the requirements of the current legislation are accomplished, immigrants obtain access to the PHS, a process which may take several years. OSF is providing medical help exclusively to those immigrants who have yet to gain access to the Public Health System. This characteristic makes it possible for this Non-Governmental Organisation to sense the evolution of medical problems of the immigrated population in the very first years following arrival to Italy.
Here, we studied the demographic and clinical characteristics of individuals suffering from allergic rhinitis and/or asthma, who were referred to allergists by general practitioners volunteering at OSF. We found dramatic evidence for the effect of exposures to the environmental factors of the Milan metropolitan area in the induction of allergic rhinitis and asthma from the first years after arrival, and a population-based prevalence of allergies in immigrants from South America.
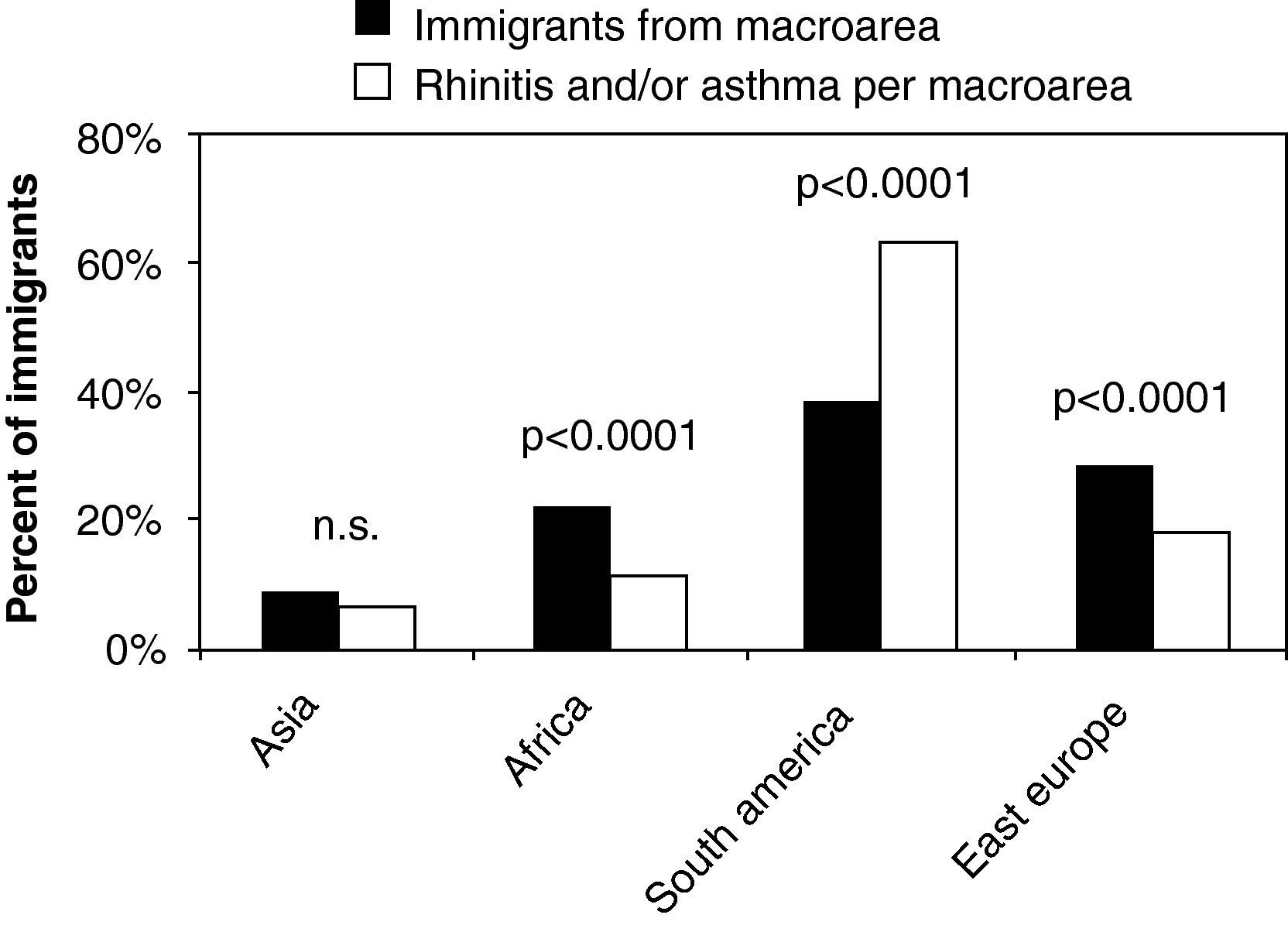
MethodsPatientsThis is an observational, retrospective study. Male and female subjects (age 15-71) were enrolled in the June 2005-June 2009 time interval; their demographic characteristics are listed in Table 1. General practitioners referred to allergists patients with diagnosis of allergic rhinitis and/or asthma. This applied both to immigrants recruited in the Opera San Francesco outpatients service, where general practitioners are in charge of the preliminary evaluation of any patient, and to resident Italians who sought the consultation of allergists at a public hospital (San Raffaele Hospital, Milan) following the advice of their family doctor.
Demographic characteristics.
| Macro-area of origin | Immigrants | |||
| Women/men (ratio) | Mean age±SD (years) | |||
| Allergy | Unselected | Allergy | Unselected | |
| Asia | 14/12 (1.16) | 373/2594 (0.14) | 33.20±3.87 | 39.30±3.54 |
| Africa | 14/32 (0.44) | 859/6379 (0.13) | 35.67±5.29 | 37.08±4.14 |
| Central and South America | 172/78 (2.20) | 6546/3975 (1.65) | 37.63±8.75 | 35.08±1.08 |
| Eastern Europe | 55/18 (3.05) | 5241/5983 (0.88) | 39.61±3.17 | 32.98±5.57 |
| 255/140 (1.82) | 13019/18931(0.69) | 37.05±6.00 | 37.30±6.25 | |
| Residents | ||||
| Women/men (ratio) | Mean age±SD (years) | |||
| Allergy | Unselected | Allergy | Unselected | |
| 757/638 (1.19) | 8037/8230 (0.98) | 38.48±15.35 | 46.7±15.05 | |
| Allergic | Total | ||||||
| Female | Male | Female | male | P | Odds ratio | CI | |
| Immigrants (N=395) | 255 | 140 | 13755 | 18795 | <0.0001 | 2.649 | 2.152-3.259 |
| Residents (N=1395) | 757 | 638 | 8037 | 8231 | 0.0005 | 1.215 | 1.089-1.356 |
Odds ratio for female versus male in immigrants and residents with rhinitis and/or asthma.
In order to compare the characteristics of allergic subjects versus the whole cohort they belonged to, immigrants who sought medical help at OSF in the same time-period were considered. As for the resident population, a representative sample of the Italian population was evaluated, corresponding to persons who registered for having access to any medical intervention provided with a regimen not requiring admission to the San Raffaele Hospital in the January-March 2009 period.
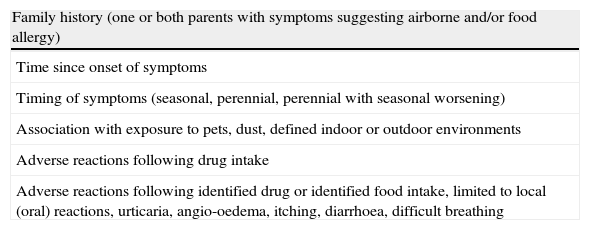
At Opera San Francesco, vital statistics, data about the country of origin, day of arrival to Italy, information on smoking habit, pregnancies, abortion, surgical interventions, allergies, and previous therapies were systematically collected at first visit by general practitioners, with the help of a standard electronic form which is part of a database running on a Filemaker Pro8® software platform (Filemaker Inc., Santa Clara, CA, USA). Because of the linguistic and culture problems, in order to properly fill in all the required parts of this form, the help of social mediators and translators was warranted whenever considered useful or necessary, as part of a routine activity of the OSF outpatient service. The consultation of an allergist was requested by the general practitioner when the diagnosis of allergic rhinitis and/or asthma was made. Other allergic problems were sometimes indicated (food allergy, drug hypersensitivity, urticaria), and these are not considered in the present analysis. The allergist who took over a patient's care extended the collection of the clinical history with a standard allergological questionnaire, which included detailed information on family history and time of first appearance of allergic symptoms (Table 2). Moreover, each patient underwent chest auscultation and prick testing (see below). Clinical diagnosis of rhinitis and asthma in immigrants and Italian patients were established according to current guidelines.7,8
Standard allergological questionnaire.
| Family history (one or both parents with symptoms suggesting airborne and/or food allergy) |
| Time since onset of symptoms |
| Timing of symptoms (seasonal, perennial, perennial with seasonal worsening) |
| Association with exposure to pets, dust, defined indoor or outdoor environments |
| Adverse reactions following drug intake |
| Adverse reactions following identified drug or identified food intake, limited to local (oral) reactions, urticaria, angio-oedema, itching, diarrhoea, difficult breathing |
Sensitisation to inhalant allergens was established in all patients, using a panel of commercial extracts for skin prick test (HAL Allergy, Milano, Italy) appropriate to the area where they patients were living. These included Dermatophagoides pteronyssinus and farinae (50% mix), Phleum pratense, Betula verrucosa, Alternaria alternata, Parietaria officinalis, Felis domesticus, Canis familiaris, Ambrosia artemisiifolia, and Artemisia absinthium. A 20-min skin prick test was performed with a standard skin pricker (Allergy pricker, Bayer DHS, Milan, Italy) by applying a drop of each extract to the volar surface of the forearm. Histamine chloride (10mg/ml) and saline (negative control) were included as positive and negative controls, respectively. A positive prick corresponded to a wheal whose diameter was > 3mm.9
Ethical issuesData from the database of the outpatient service of Opera San Francesco and San Raffaele Institute were treated anonymously and extrapolated as pooled data. This project was revised and approved by the Ethics Committee of OSF and San Raffaele Hospital (Protocol BBIA 10-10-05).
Statistical analysisDifferences between groups were examined for statistical significance using the two-tailed Fisher's test with Yates correction. P values of less than 0.05 were considered statistically significant.
ResultsPatients’ characteristicsImmigrants selected at OSF who were included in this study were 395 subjects referred to the allergist by the general practitioner with a diagnosis of rhinitis and/or asthma in the June 2005-June 2009 time frame and 31,950 subjects who sought medical help for any reason in the same time frame. As control groups, 1395 residents were included in this study, who were referred by the general practitioner with a diagnosis of rhinitis and/or asthma to one allergist of a public hospital serving the same area (San Raffaele, Milan), and 16267 subjects who sought medical help at the outpatients facilities of the same hospital for any reason in the same time period (Table 1). The proportions of subjects with a diagnosis of allergy and/or asthma who were sent to the allergist by general practitioners were therefore 1.24 and 8.58% in immigrants and residents, respectively (p<0.0001)
Females with allergy were more numerous than males both in immigrant and in residents (p<0.001 for both comparisons, with odds ratio of female versus male equal to 2.649 and 1.215 for immigrants and non-immigrants, respectively) (Table 1).
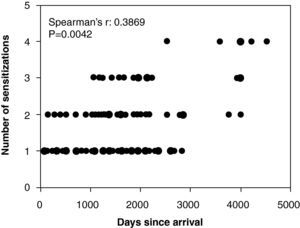
Permanence in Italy and appearance of allergic symptomsFirst onset of allergic symptoms in immigrants ranged from 178 days to 12.38 yrs from arrival. Average values of times from first onset of symptoms did not differ in patients from different macro-areas (not shown). Notably, a significant correlation was found between number of sensitisations and the time of permanence in the Milan metropolitan area (non-parametric correlation analysis yielded Spearman r value equal to 0.3869, with a 95% confidence interval ranging from 0.2258 to 0.5274 and a 2-tailed p value of 0.0042) (Fig. 1).
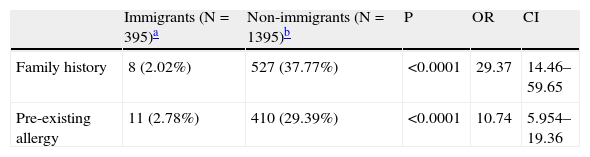
Personal and familial history for allergic diseases in immigrants and in residents at first allergological visitAmong patients with allergic rhinitis and/or asthma resident in the Milan metropolitan area, those who described at their first allergological visit a previous personal and/or a familial history of allergic diseases were 37.77 and 29.39%, respectively. In contrast, only 2.02% and 2.27% of immigrants with allergic rhinitis and/or asthma reported a positive anamnesis for these problems (p<0.0001 vs. residents for both comparisons) (Tables 3a–3d). Evidence of previous allergic symptoms in immigrants referred in all cases to problems they suffered of in the country of origin. This observation suggests per se a strong environmental influence in the generation of allergic symptoms in newly immigrated people.
Proportion of patients with rhinitis and/or asthma with positive familial and/or known pre-existing allergies at study entry.
| Immigrants (N=395)a | Non-immigrants (N=1395)b | P | OR | CI | |
| Family history | 8 (2.02%) | 527 (37.77%) | <0.0001 | 29.37 | 14.46–59.65 |
| Pre-existing allergy | 11 (2.78%) | 410 (29.39%) | <0.0001 | 10.74 | 5.954–19.36 |
Distribution of skin sensitisations in immigrants and residents of the Milan metropolitan area.
| Immigrants (N=395) | Residents (N=1395) | ||||||
| Allergen | N | % | N | % | p | OR | CI |
| House dust mites | 145 | 43.8 | 405 | 33.4 | 0.0044 | 1.084 | 1.024–1.148 |
| Blattella germanica | 70 | 17.7 | 35 | 2.5 | <0.0001 | 8.369 | 5.480–12.780 |
| Felis domesticus | 65 | 19.6 | 198 | 16.3 | 0.2606 | ||
| Canis familiaris | 35 | 10.6 | 124 | 10.2 | 1.0000 | ||
| Alternaria alternata | 13 | 3.9 | 98 | 8.1 | 0.0062 | 2.220 | 1.231–4.005 |
| Phleum pratense | 221 | 66.8 | 774 | 63.8 | 0.9087 | ||
| Betula verrucosa | 121 | 36.6 | 541 | 44.6 | 0.0031 | 1.435 | 1.129–1.823 |
| Parietaria officinalis | 124 | 37.5 | 554 | 45.7 | 0.0027 | 1.440 | 1.135–1.827 |
| Ambrosia artemisiifolia | 55 | 16.6 | 254 | 20.9 | 0.0498 | ||
| Monosensitised | 56 | 16.9 | 245 | 20.2 | 0.1273 | ||
| Sensitisations per patienta | 1.97 | 2.11 | |||||
aNumber of sensitisations per patient was calculated considering only patients with at least one positive prick test. Nine immigrants and 96 residents who were sent with a diagnosis of rhinitis and/or asthma by the general practitioner did not display any sensitisation to the allergens included in the panel.
Diagnosis at onset.
| Immigrants (N=395)a | Non immigrants (N=1395)a | P | OR | CI | |||
| Asthma only | 20 | 5.1% | 90 | 6.4% | 0.3441 | ||
| Rhinitis only | 114 | 28.9% | 364 | 26.1% | 0.2741 | ||
| Rhinitis and asthma | 261 | 66.0% | 941 | 67.4% | 0.6275 | ||
| Asthma total | 281 | 71.1% | 1031 | 73.9% | 0.2741 | ||
| Rhinitis total | 375 | 94.9% | 1305 | 93.5% | 0.3441 | ||
| Adverse drug reactions | 54 | 13.7% | 265 | 19.0% | 0.0140 | 1.481 | 1.079–2.033 |
| Food allergy | 84 | 21.3% | 305 | 21.9% | 0.8359 | ||
aNumber of sensitisations per patient was calculated considering only patients with at least one positive prick test. Nine immigrants and 96 residents who were sent with a diagnosis of rhinitis and/or asthma by the general practitioner did not display any sensitisation to the allergens included in the panel.
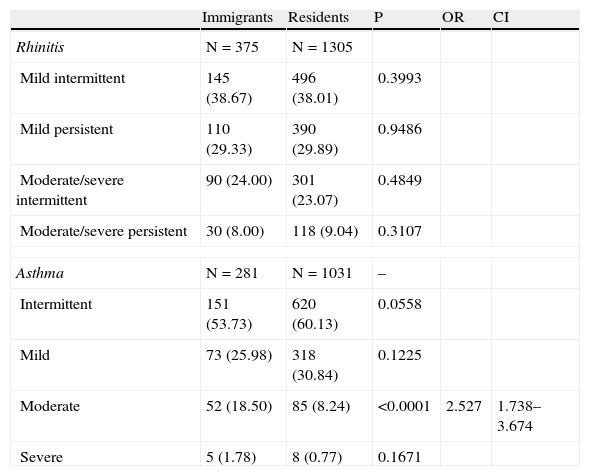
Clinical characteristics of rhinitis and asthma in immigrants and residents.
| Immigrants | Residents | P | OR | CI | |
| Rhinitis | N=375 | N=1305 | |||
| Mild intermittent | 145 (38.67) | 496 (38.01) | 0.3993 | ||
| Mild persistent | 110 (29.33) | 390 (29.89) | 0.9486 | ||
| Moderate/severe intermittent | 90 (24.00) | 301 (23.07) | 0.4849 | ||
| Moderate/severe persistent | 30 (8.00) | 118 (9.04) | 0.3107 | ||
| Asthma | N=281 | N=1031 | – | ||
| Intermittent | 151 (53.73) | 620 (60.13) | 0.0558 | ||
| Mild | 73 (25.98) | 318 (30.84) | 0.1225 | ||
| Moderate | 52 (18.50) | 85 (8.24) | <0.0001 | 2.527 | 1.738–3.674 |
| Severe | 5 (1.78) | 8 (0.77) | 0.1671 | ||
The proportion of individuals with only one sensitisation to airborne allergens, within the panel of considered allergen extracts (“monosensitised” subjects) did not differ in immigrants (16.9%) versus resident patients (20.2%) with allergic rhinitis and/or asthma. When the frequency of sensitisation to each single allergen was considered, individuals sensitised to house dust mites were more numerous among immigrants as compared to residents (43.8% vs. 33.4%9, p=0.0044). Individuals sensitised to Alternaria, Fagales tree pollen and Parietaria pollen were more frequent among residents (8.1%, 44.6% and 45.7%, respectively) as compared to immigrants (3.9%, 36.6% and 37.5%, respectively) (p=0.0062, 0.0031 and 0.0027, respectively). No differences were found in the proportions of subjects allergic to animal epithelia, grass pollen and ragweed (Tables 3a–3d).
Clinical characteristics of allergic immigrants versus residentsThe diagnostic conclusions given by allergists in the study groups were analysed as follows: isolated or combined allergic asthma and allergic rhinitis, food allergy, and adverse drug reactions. Diagnosis at onset for immigrants and residents are shown in Tables 3a–3d. No differences in frequency of the various considered pathological conditions or combination thereof were observed between the study groups, with the exception of drug allergies, which were more frequent in residents (Tables 3a–3d).
Severity of rhinitis (7) and asthma (8) were scored with the corresponding 4-score scales provided by international guidelines, respectively. A prevalence of moderate asthma (18.50% vs. 8.24%) was found in immigrants vs. residents (p<0.0001, respectively). Patients with the other considered levels of severity were equally represented in the study groups (Tables 3a–3d).
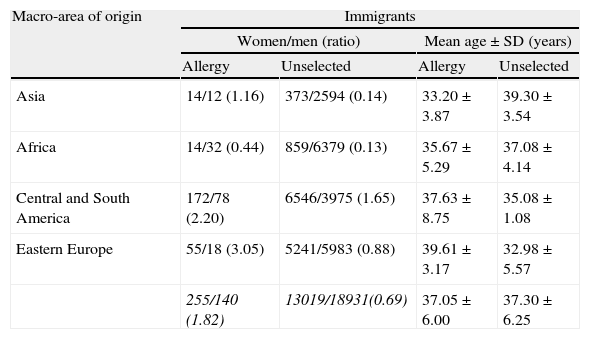
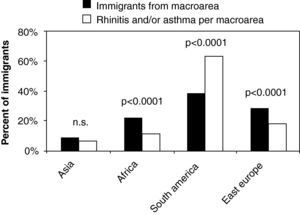
Geographic origin and frequency of rhinitis and/or asthmaWhen divided according to the macro-area of origin, the proportion of Asian patients with rhinitis and/or asthma mirrored the proportion of overall Asian patients visited for any medical problem at OSF (p=0.0787) (Fig. 2). In contrast, the proportions of allergic individuals from Africa and East Europe were significantly lower than expected from the corresponding proportions of overall subjects from these areas visited by general practitioners at OSF (p<0.0001 for both comparisons). More interestingly, the proportion of South American immigrants with rhinitis and/or asthma was almost double that expected from the proportion of patients from this macro-area visited by general practitioners at OSF (p<0.0001) (Fig. 2).
Frequency of allergic individuals (in percent values) among immigrants visited at the OSF.
Significance data are shown with actual p values of comparisons between percentage of individuals who were enrolled to the study, and percentage of allergic individuals, after grouping per macro-area of origin (on the x-axis).
Allergy is determined by genetic and environmental factors. The evaluation of asthma and allergy in persons migrating from developing to industrialised countries provide a unique opportunity to investigate the role of environmental factors in the development of these diseases.10–17
Here, we report that newly immigrants from widely different areas of the world to a highly polluted metropolitan area in Northern Italy18 display a time-dependent increase in the number of sensitisations to inhalant allergens and more severe asthmatic symptoms as compared to the resident population. Moreover, we show that immigrants from South America are significantly more prone to develop allergic rhinitis and/or asthma, as compared to immigrants from other areas of the word, suggesting the influence of genetic factors, which deserve further investigation.
In our case history, female prevailed over men for allergic disorders both among immigrants and among residents. This observation is in line with previous knowledge on sex differences in health. In fact, females have been long known to show higher incidence of acute and minor chronic conditions, more short-term restricted activity, and more use of outpatient services as compared to males.19 Moreover, it was recently reported that women demonstrated worse asthma control compared with men with regard to several short-term and long-term measures, despite reporting higher rates of inhaled corticosteroid use and routine asthma care visits.20 Finally, in a recent survey of 16,408 unselected individuals who underwent allergen microarray-based determination of specific IgE to inhalant and food allergens, female prevalence was confirmed considering the whole population and the whole allergen set.21
In our knowledge, we report here for the first time the correlation between the time of stay of subjects to a Westernised Country and the number of sensitisations to locally relevant airborne allergens. These data, taken together with the dramatic differences in the proportion of individuals with familial history of allergies among immigrants as compared to residents, support the speculation that environmental factors may play a relevant role in the triggering of these diseases. Notably, the observed positive family history for allergic diseases is very low also in comparison with that reported by other studies in the general population,6,22 even when they were performed in the same geographic area.23 This is also in agreement with the observation of Tedeschi et al., who reported a positive clinical history in only 16% of immigrants.12
Data about the lack of respiratory allergies before immigrations may be affected by information biases related to under-reporting family and/or familiar histories. However, at OSF, linguistic help is provided for all the most representative ethnic groups by dedicated personnel, which makes data collection accurate and reliable, in particular concerning the administration of standard questionnaires such as the one which was used for allergic diseases.
A relatively higher number of individuals sensitised to mite allergens and cockroaches was observed among immigrants, as compared to residents, a result that may depend on the typical job assignments of the former, which mostly imply home care duties, or in poorer hygienic conditions,24 respectively. However, the partial cross-reactivity between the major allergens of cockroaches and dust mites25 may act as a confounding factor here.
Positive skin tests for local allergens in a proportion similar to the resident population also represent a very intriguing aspect, since they clearly demonstrate that the observed sensitisations were acquired locally, since mugwort is not a relevant allergen in any of the geographical areas considered, and this also applies to Fagales, with the exception of East-European populations.
Overall, diagnosis at onset was similar in immigrants and residents, with the exception of hypersensitivity reactions to drugs, which were more frequent in the latter. We speculate that this may depend on the different ease in the access to medical care between the compared groups of patients.
The comparison of the proportion of allergic individuals from different areas of the world clearly indicated that the proportion of patients from South America was significantly higher than the proportion of immigrants from that macro-area. Over-representation of this subset persisted when data were analysed separately for males and females (not shown). Allergic diseases are caused by a complex interaction between host genetics and environmental exposures. In the interpretation of this phenomenon, it has to be considered that rural residence is consistently identified as the strongest protective factor against asthma in epidemiological studies26–28 and is likely to be associated with such diverse environmental and cultural occurrences as life style, diet, and hygiene.29,30 All these variables are difficult to account for and properly balance in the study populations. Despite this watchfulness, we suggest that genetic factors specific to South America populations may also play a specific role in this context.
Our data encourage the application of genome-wide association studies on populations of widely different ethnic origin who are subjected to the same environmental exposure and have different outcomes in terms of development of allergies, such as those described in the present study. The crucial environmental factors still await clear identification. In this context, platinum group elements are candidate pro-allergic components31,32 in emissions dependent on urban transportation. The differential effect of the same environmental triggers on different genetic backgrounds appears a favourable experimental set up to unveil those genes associated to asthma and allergy which control biological functions related to the response to environmental insults, such as oxidative stress (e.g., GSTM1).33–35 In this context, the application of admixture mapping appears as a promising opportunity. Admixture mapping studies have defined single-nucleotide polymorphism panels that can distinguish between chromosomal segments of Amerindian or European Ancestry,36,37 just posing the basis for whole genome association studies exploiting relatively limited sets of markers (in the range of few thousands, rather than the 300,000–1,000,000 required for a whole-genome haplotype scan).38 Similar approaches provided promising results in studies of African Americans susceptibility regions for multiple sclerosis39 and prostate cancer.40
Clarification of the dynamics behind the causation of allergy and asthma in urban migrant populations will further improve our understanding of what is behind the increase of frequency of these diseases with urbanisation and westernisation. The identification of modifiable risk factors could lead to new public health initiatives to reduce the burden of allergic disease among urbanising populations.
Conflict of interestThe authors have no conflict of interest to declare.
The professional work of medical doctors, nurses and administration personnel volunteering at the Opera San Francesco Non-Governmental Organization is gratefully acknowledged.