Exfoliative skin diseases of the neonate are relatively rare but when present require rapid diagnosis and treatment to decrease morbidity and mortality associated with these entities. Toxic epidermal necrolysis (TEN) is an acute, rare life-threatening drug reaction associated with 30% mortality. 1 This disorder is characterised by extensive full- thickness necrosis of epidermis and mucous membrane involvement. TEN could be considered an extreme form of Stevens-Johnson syndrome, when an epidermal detachment > 30% of the body surface occurs coupled with widespread purpuric macules or flat atypical targets.2 This entity is considered extremely rare in the neonatal period.
We report a case of male term newborn infant, Apgar 8/9, weight 2860g, with characteristics of Down syndrome (47XY+21). He had bilateral cephalhaematoma and physiologic jaundice, besides respiratory distress and needing supplemental oxygen. On the third day of life an abscess in right knee was noted, and blood count with low platelets (78,000) and elevated C-reactive protein. An antibiotic combined regimen was started of crystalline penicillin plus gentamicin for 7 days that was substituted by oxacillin because of elevated ratios of immature neutrophils. One day after starting oxacillin, the blood culture revealed growth of Staphylococcus haemolyticus oxacillin resistant and the antibiotic was changed to vancomycin. Infection was controlled clinically and by laboratory findings.
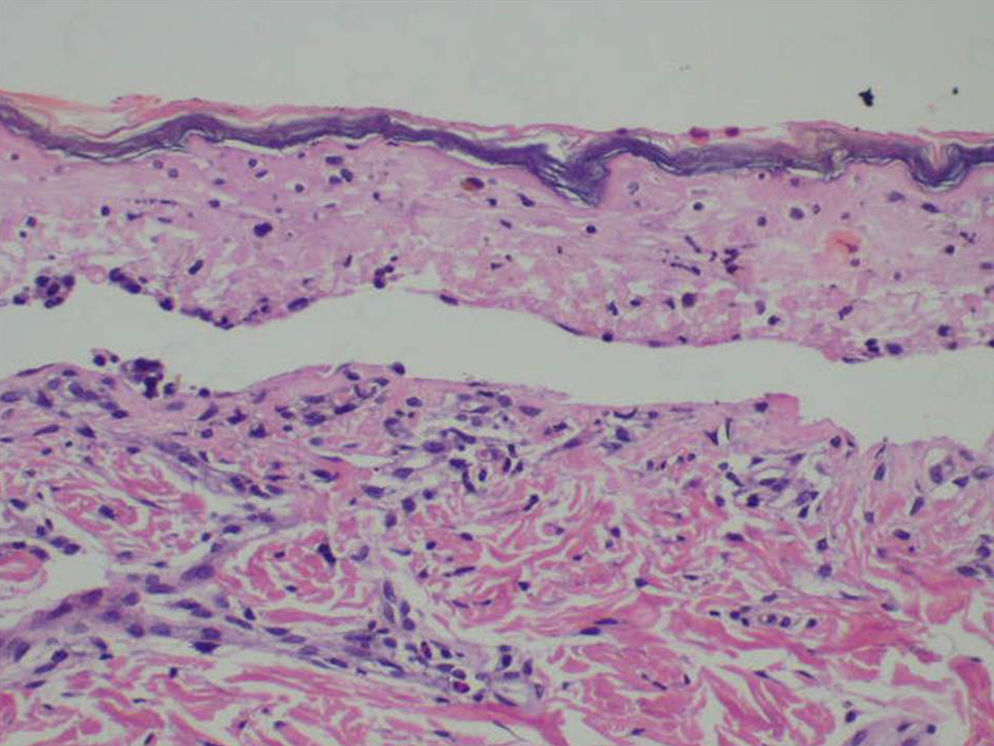
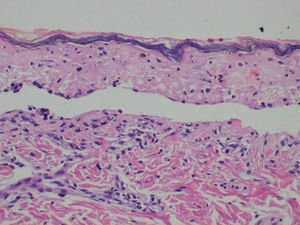
After the use of vancomycin for 10 days, on the 20th day of life, he developed erythematous target lesions on trunk, abdomen, and next day developed bullous lesions with separation of epidermis in more than 30% of the corporal surface, besides labial and ocular damage. His mother received antibiotic (penicillin) for treatment of skin infections and she was breast feeding. The results of serological tests were negative for toxoplasmosis, rubella, syphilis, cytomegalovirus, mononucleosis and herpes virus. Skin biopsy revealed keratinocyte necrosis with subepidermal bullous lesions, indicating TEN. He presented serious ocular lesions with cornea ulceration. He received systemic corticosteroid, dexamethasone (0.4mg/kg/day for 5 days) and care in the lesions, remaining in the Intensive Care Unit. He was accompanied by teams of allergy, dermatology and ophthalmology with diagnostic agreement of TEN. In vitro tests (lymphocyte transformation test) for evaluation of delayed immune reaction to drug were not available in our hospital.The cutaneous lesions improved with progressive reepithelialisation. However, on the third day of corticosteroids he relapsed with fever, leucopoenia (4,500 leukocytes/mm3) and thrombocytopenia (49,000 platelets/mm3) and amikacin and clindamycin were introduced. He evolved with septicaemia (positive blood culture for negative-coagulase Staphylococcus and Klebsiella) and antibiotics were changed to teicoplanin and fluconazole, and received gammaglobulin (400mg/kg/day for 5 days). There was worsening of the disease with abdominal distension. Laparotomy showed extensive necrotising enterocolitis in all the intestine which suggested mesenteric thrombosis. It was associated to Ciprofloxacin+Metronidazole. He developed septic shock, vasculitis with necrosis of extremities and death occurred on the 49th day of life.
The pathophysiology of TEN remains unknown. The condition is usually caused by drugs.3 TEN seems to be extremely rare in newborns, with few cases reported.4,5 Cases of TEN in the neonatal period are associated with sepsis and use of various medications. (Figs. 1–3)
Other diseases should be considered in the differential diagnosis of TEN, such as staphylococcal scalded skin syndrome4 (mainly in the neonatal period), linear IgA dermatosis, paraneoplastic pemphigus, acute graft-versus-host disease, drug-induced pemphigoid and pemphigus and acute generalised exanthematous pustulosis.2 Features of TEN which reinforces the diagnosis of the disease include keratinocyte necrosis and cleavage at the basal layer with loss of the entire epidermis.3 The skin biopsy of our patient showed keratinocyte necrosis with subepidermal bullous lesions, which allows to distinguish it from the usual characteristics of pathological study of scalded skin syndrome. Another point to consider here is the onset of TEN over a period of stability of the infection and associated with the use of an antimicrobial drug, the possible aetiology of TEN.
The majority of patients with TEN die from complications of infections. The major causes of sepsis in TEN patients are Staphylococcus aureus and Pseudomonas aeruginosa.3 Our patient had positive blood culture for negative-coagulase Staphylococcus and Klebsiella. The corticosteroids, when indicated, should be early and have short duration to avoid complications, especially infections and increased catabolism. Our patient received 5 days of dexamethasone and developed signs of infection on the third day of corticosteroid. Intravenous immunoglobulin has recently been shown to result in rapid improvement in both adults and children, when used early.1,2 Our patient received 0.4g/kg/day for 5 days, but this therapy with gammaglobulin was used late with a focus on recovery from sepsis. We reported a case of newborn infant that presented TEN associated of drugs (ß-lactam antibiotic x vancomycin) administered to septic infant with fatal evolution.