Hen's egg is responsible for one of the most frequent food allergies in childhood. About two-thirds of children will outgrow their egg allergy by early school age (1). The persistence of egg allergy or its late onset has usually a less favourable prognosis.
Hen's egg is composed by a non-allergic shell (10% of the egg), egg white (60%) and egg yolk (30%). Egg white is 10% protein and 88% water, being more allergenic than egg yolk. The former contains more than 20 proteins, four of them being major allergens. The most prevalent protein is ovalbumin (Gal d 2, 55%), which is thermolabile. On the other hand, ovomucoid (Gal d 1, 11%), ovotranferrin or conalbumin (Gal d 3, 12%) and lysozyme (Gal d 4, 3%) are heat-stable. Alpha-livetin or chicken serum albumin (Gal d 5) is the major allergen in egg yolk, being implicated in the bird-egg syndrome.1
Food tolerance mechanisms are not completely understood but there are several known factors that can affect it.2 It is postulated that a failure in oral tolerance induction or a breakdown in previously acquired tolerance results in food hypersensitivity. The latter is responsible for late onset food allergy cases but it is not always possible to explain why and how it happens.
We present a case of a female teenager who referred recurrent oral allergy syndrome (OAS) since she was eleven, within 2 months after Hodgkin's lymphoma (mixed cellularity type, stage 3B) diagnosis and chemotherapy beginning (with BEACOPP chemotherapy regimen: doxorubicin, bleomycin, vincristine, cyclophosphamide, etoposide and prednisone). After 6 months of chemotherapy, Hodgkin's lymphoma was in remission. She did not perform radiation therapy.
At the age of 14 she began recurrent eyelid angio-oedema, with no specific trigger. After an episode of glottis oedema related to croissant ingestion, she decided to avoid cakes and pastry. Besides that, she maintained recurrent angio-oedema and she was referred to our allergy department in November of 2007, at 17 years. She had always tolerated egg and egg containing foods until the age of 11 and she has never lost boiled egg tolerance. There was no personal history of food allergy. She had no recent or past history of birds or egg proteins exposition. Her personal history included pollinic rhinoconjuntivitis since she was 14. She denied a clinical history of atopic eczema, asthma, drug allergy or insect bite allergy. She also denied any regular medication (namely acid suppression treatment) besides chemotherapy until she was 17.
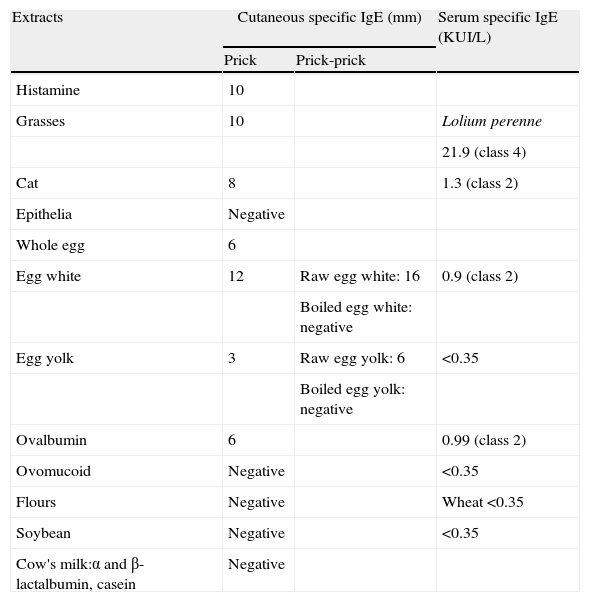
The immunoallergic study revealed normal cell counts, serum immunoglobulins, complement fractions, immunoelectrophoresis, lung function and chest X-ray. The study of autoimmunity, celiac disease and viral serologies were all negatives. The paranasal sinus X-ray showed maxillary sinusitis. Skin prick tests (prick method) were performed with a battery of common aeroallergens (ALK Abelló, Madrid, Spain), epithelia (ALK Abelló, Madrid, Spain), food commercial extracts (Leti, Madrid, Spain) and skin prick tests (prick-prick method) with fresh egg (raw and boiled), as well as serum level of total and specific IgE. Table 1 presents cutaneous and serum specific IgE reactivities.
Cutaneous and serum specific IgE results.
| Extracts | Cutaneous specific IgE (mm) | Serum specific IgE (KUI/L) | |
| Prick | Prick-prick | ||
| Histamine | 10 | ||
| Grasses | 10 | Lolium perenne | |
| 21.9 (class 4) | |||
| Cat | 8 | 1.3 (class 2) | |
| Epithelia | Negative | ||
| Whole egg | 6 | ||
| Egg white | 12 | Raw egg white: 16 | 0.9 (class 2) |
| Boiled egg white: negative | |||
| Egg yolk | 3 | Raw egg yolk: 6 | <0.35 |
| Boiled egg yolk: negative | |||
| Ovalbumin | 6 | 0.99 (class 2) | |
| Ovomucoid | Negative | <0.35 | |
| Flours | Negative | Wheat <0.35 | |
| Soybean | Negative | <0.35 | |
| Cow's milk:α and β-lactalbumin, casein | Negative | ||
Battery of common aeroallergens (ALK Abelló, Madrid, Spain), epithelia (ALK Abelló, Madrid, Spain), food commercial extracts (Leti, Madrid, Spain) and fresh egg.
Both clinical history and presented results are suggestive of a late onset egg allergy, soon after Hodgkin's lymphoma diagnosis and chemotherapy began. We have recommended eviction of foods containing raw egg; precaution in the administration of egg-containing vaccines and she was prescribed with a written treatment plan for reactions to unintentional exposure, including self-injectable epinephrine.
Since then, she has had no more angio-oedema episodes. She has grass pollen induced rhinoconjunctivitis and sinusitis controlled under nasal corticosteroids and oral antihistamines on demand. Periodically, clinical and laboratorial assessment has been made in order to look for an eventual egg tolerance development.
We document a raw egg allergy case, namely to ovalbumin, a thermolabile protein responsible by the absence of symptoms with boiled egg. This can be found as an occult allergen in foods, namely in those incompletely cooked, which justifies recurrent angio-oedema besides eviction of products in which egg presence was undoubted.
Asero et al.3 also described an OAS in a 47-year-old woman, after ingestion of egg-containing foods, besides boiled egg tolerance.
Why did this patient, without previous food allergy, lose egg tolerance at the age of 11? It has been suggested that the prevalence of food allergy is higher in patients with gastrointestinal diseases,4 which can occur as a cause or a result of intestinal inflammation. Given the closer temporal relationship between egg allergy symptoms and the diagnosis of Hodgkin's lymphoma, this disease and/or its treatment could have predisposed this patient to egg sensitisation. This could happen by a mechanism similar to that of Crohn's disease, in which one of the pathologic steps is the loss of oral tolerance to gut flora.5 Inflammation and infection can lead to intestinal epithelia tight-junctions disruption and, therefore, increase of intestinal mucosa permeability with decrease of sensitisation threshold and loss of oral tolerance.6 This process could also be induced by chemotherapy, since these drugs can affect either the normal cells with high multiplication rates, as is the case of bowel's mucous membrane (enterotoxicity) or the gut flora, an immunomodulator of the immune system. Constant microbial stimuli from the gut flora seem to be required to keep a successful maturation of the gut mucosal immune system. It has been reported that the lack or inadequacy of such stimuli has resulted in a decreased intestinal area, altered mucosal enzymes, defects in the intestinal barrier function, reduced inflammatory responses, a defective mucosal IgA system, and a deficient oral tolerance.7
There is evidence that psychological stress, on its own, can induce disruption of biological systems related to inflammation through mechanisms potentially overlapping with those altered by physical pollutants and toxicants. It seems that stress influences neuroimmunoregulation and oxidative stress pathways, which could modulate hypersensitivity response. Some studies in mice models proved that physical and psychological stress can induce intestinal sensitisation to luminal antigens and oral tolerance disruption by inducing alterations in colonocyte differentiation and decreased expression of RNAm encoding tight junction proteins, with a consequent increase in paracellular permeability and excessive uptake of luminal material.8,9 Stress is also associated to gut flora changes, with the possible consequences already discussed above.
Unsel et al.10 had reported a clinical case of egg allergy onset at the age of 53, in a previous healthy woman, after her 21-year-old daughter had died from a brain tumour.
Thus, bowel mucous membrane can have two opposite roles in food allergy: a protecting role as an efficient first-line protection against food allergy, conducing to oral tolerance under physiological conditions; on the other hand, it can be responsible either by the absence of tolerance gain or by the lost of previously acquired tolerance, as probably happened in this case.
This case report has some particularities, namely the late onset egg allergy coincident with Hodgkin's lymphoma diagnosis and its persistence. We hypothesise that, in this patient, the initial sensitisation to egg occurred through gut mucosa as a consequence of Hodgkin's lymphoma and/or chemotherapy used in its treatment.