IgE-mediated systemic reactions to local anaesthetics may be seen- although rarely- by dentists. However, it is not known whether dentists are familiar with symptoms, signs and management of anaphylaxis.
MethodsIn this study we aimed to evaluate knowledge of dentists of the symptoms and signs and current treatment of anaphylaxis. For this, some dentists working in their private offices in Istanbul were asked to complete an anonymous questionnaire with 15 questions related to anaphylaxis.
ResultsA total of 86 dentists agreed to participate in the study. None of the attendants were completely aware of the symptoms and signs of anaphylaxis. About half of the attendants (48.8%) knew epinephrine as the first drug in the treatment of anaphylaxis and keep it in their offices (55.6%), but only one third of the dentists (31.5%) preferred intramuscular route as the most effective route for epinephrine injection.
ConclusionOur data show that the level of dentists’ knowledge of local anaesthetics allergy and anaphylaxis is inadequate. This may endanger patients’ lives. An educational programme that may improve general dentists’ knowledge about local anaesthetics allergy and anaphylaxis is urgently necessary.
Anaphylaxis is one of the most urgent of clinical allergic events in every field of medicine, affecting between 1% and 2% of the general population.1 Although drugs are responsible for most of the anaphylactic reactions in addition to foods, local anaesthetics (LAs) also rarely lead to severe systemic reactions.2,3 Nevertheless, dentists often refer their patients with suspected drug allergy to allergy clinics to be tested with LAs. On the other hand, drug allergies and anaphylaxis may occur without any previous symptoms. For this reason, symptoms, signs, and treatment of anaphylaxis should be known by dentists just like all other health care professionals.4 But we do not know whether the dentists, especially those working in their private offices, are familiar with LAs allergy and anaphylaxis. This study was performed to learn if office-working dentists who may see cases with anaphylaxis in their daily practice have adequate information about symptoms, signs, and management of anaphylaxis.
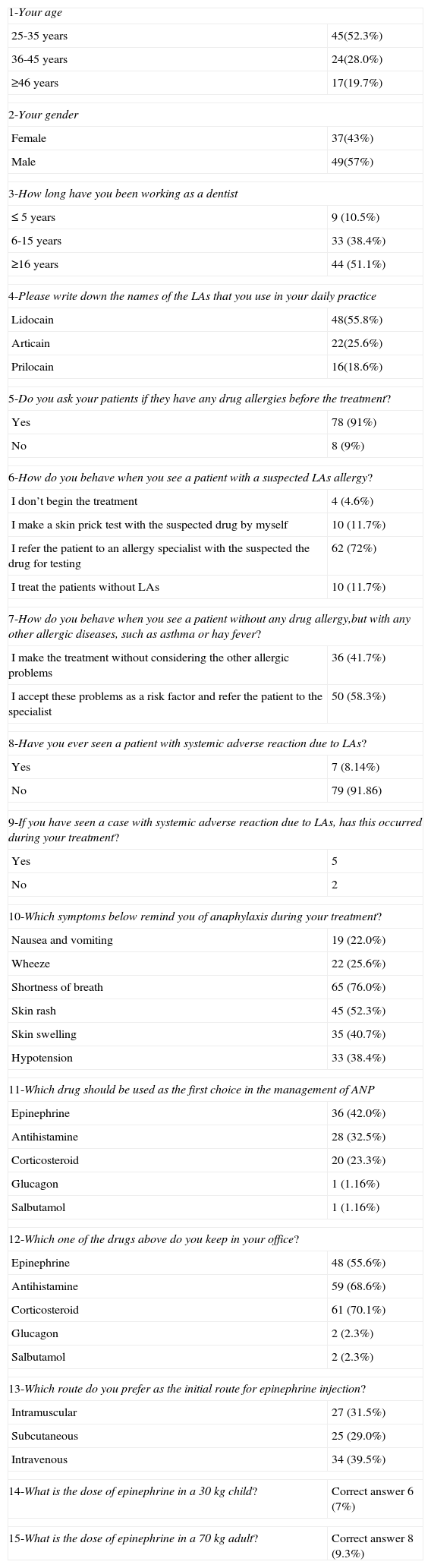
Material and methodsThe study was performed among dentists working in their private offices in Anatolian part of Istanbul in 2010. The dentists were randomly selected from a list and they were asked by telephone if they wanted to join the study. Those who accepted to join the study were visited in their offices and a questionnaire (Table 1) designed to document the general knowledge of the dentists on the signs, symptoms and management of anaphylaxis was distributed and they were asked to answer the questions without explaining their identifications. The survey consisted of 15 questions, three of which contained demographic data and 12 questions asking about the LAs and anaphylaxis (Table 1).
The questions in the questionnaire and the dentists’ answers.
| 1-Your age | |
| 25-35 years | 45(52.3%) |
| 36-45 years | 24(28.0%) |
| ≥46 years | 17(19.7%) |
| 2-Your gender | |
| Female | 37(43%) |
| Male | 49(57%) |
| 3-How long have you been working as a dentist | |
| ≤ 5 years | 9 (10.5%) |
| 6-15 years | 33 (38.4%) |
| ≥16 years | 44 (51.1%) |
| 4-Please write down the names of the LAs that you use in your daily practice | |
| Lidocain | 48(55.8%) |
| Articain | 22(25.6%) |
| Prilocain | 16(18.6%) |
| 5-Do you ask your patients if they have any drug allergies before the treatment? | |
| Yes | 78 (91%) |
| No | 8 (9%) |
| 6-How do you behave when you see a patient with a suspected LAs allergy? | |
| I don’t begin the treatment | 4 (4.6%) |
| I make a skin prick test with the suspected drug by myself | 10 (11.7%) |
| I refer the patient to an allergy specialist with the suspected the drug for testing | 62 (72%) |
| I treat the patients without LAs | 10 (11.7%) |
| 7-How do you behave when you see a patient without any drug allergy,but with any other allergic diseases, such as asthma or hay fever? | |
| I make the treatment without considering the other allergic problems | 36 (41.7%) |
| I accept these problems as a risk factor and refer the patient to the specialist | 50 (58.3%) |
| 8-Have you ever seen a patient with systemic adverse reaction due to LAs? | |
| Yes | 7 (8.14%) |
| No | 79 (91.86) |
| 9-If you have seen a case with systemic adverse reaction due to LAs, has this occurred during your treatment? | |
| Yes | 5 |
| No | 2 |
| 10-Which symptoms below remind you of anaphylaxis during your treatment? | |
| Nausea and vomiting | 19 (22.0%) |
| Wheeze | 22 (25.6%) |
| Shortness of breath | 65 (76.0%) |
| Skin rash | 45 (52.3%) |
| Skin swelling | 35 (40.7%) |
| Hypotension | 33 (38.4%) |
| 11-Which drug should be used as the first choice in the management of ANP | |
| Epinephrine | 36 (42.0%) |
| Antihistamine | 28 (32.5%) |
| Corticosteroid | 20 (23.3%) |
| Glucagon | 1 (1.16%) |
| Salbutamol | 1 (1.16%) |
| 12-Which one of the drugs above do you keep in your office? | |
| Epinephrine | 48 (55.6%) |
| Antihistamine | 59 (68.6%) |
| Corticosteroid | 61 (70.1%) |
| Glucagon | 2 (2.3%) |
| Salbutamol | 2 (2.3%) |
| 13-Which route do you prefer as the initial route for epinephrine injection? | |
| Intramuscular | 27 (31.5%) |
| Subcutaneous | 25 (29.0%) |
| Intravenous | 34 (39.5%) |
| 14-What is the dose of epinephrine in a 30kg child? | Correct answer 6 (7%) |
| 15-What is the dose of epinephrine in a 70kg adult? | Correct answer 8 (9.3%) |
ANP: Anaphylaxis LAs: Local anaesthetics
The questionnaire was answered by 86 of 100 dentists (86%). 37 of the dentists were female and the mean age of attendants was 36±3.5 years. The mean professional period they spent in practice was 8.4 years. According to the results of the questionnaire, every attendant knew one or more symptoms and signs of anaphylaxis but none of them marked all options related to anaphylaxis. Answers to the questions related to symptoms and signs of anaphylaxis were similar in all age groups. On the other hand, only half of the dentists (55.6%) knew epinephrine as the first drug of choice in the treatment of anaphylaxis, but only 27 (31.5%) of them were aware of the fact that epinephrine should be used intramuscular (IM) route when required (Table 1). 18 of 27 (67%) dentists who preferred IM route were younger than 35 years of age. About 30% of the dentists considered antihistamines and 45.4% corticosteroids to be the first-line therapy in anaphylaxis. Seven dentists had seen patients with systemic adverse reactions due to LAs and five of them had used antihistamines and corticosteroids for the treatment of cases with emergency reactions in their own practice.
DiscussionLocal anaesthetics are generally considered safe with respect to allergy. Although various clinical reactions may occur, most adverse drug reactions are not truly allergic, i.e. IgE-mediated, in nature. Only 6 to 10% of all adverse drug reactions are IgE-mediated.2 Actually, reactions are seldom related to the local anaesthetic itself and most general reactions are not allergic (i.e. IgE mediated), but are the result of vasovagal, psychogenic, toxic, or predictable side effects of the epinephrine that is often used in combination with local anaesthetics.2,5 Another possible but rare cause of immediate-type reactions is preservatives, such as methylparaben, that are present in multidose vials.6
To practice dentistry in Turkey graduation from a dental school in a university is required and to be admitted to a dental school, graduation from a high school and passing a very competitive examination is mandatory. Education programmes in Turkish dentistry schools are the same as in American and European ones.
Anaphylaxis is one of the most urgent clinical pictures in daily medical practice and should be diagnosed and treated as soon as possible.1,7 Since anaphylaxis may also be encountered by dentists –although not common-in their routine practice, they should also be aware of the symptoms and signs of anaphylaxis, and treat the severe reactions in the light of recent advances.8
Epinephrine is the drug of choice and the mainstay of therapy of anaphylaxis and subsequent therapeutic intervention depends on the clinical response to this drug.1,7,9 Until 10-15 years ago it had been accepted that subcutaneous route was the preferred route for epinephrine.10 Simons et al.11 have shown that epinephrine is more effective when given IM route rather than SC in the management of anaphylaxis. Unfortunately, this very important change has not taken place soon in general textbooks and academic programmes in dentistry schools and scientific meetings. As a result of this delay, many dentists working in their private offices are unaware of the fact that epinephrine is the first medication of choice in the management of anaphylaxis and intramuscular route of epinephrine is the route of choice. Unfortunately, in our study group most dentists did not know the priority, administration route and dose of epinephrine. Fortunately, the proportion of the younger dentists who preferred IV route was higher than older ones. On the other hand, about 40% of dentists preferred IV route for epinephrine which may be fatal.
Ampoule forms of epinephrine, antihistamines and corticosteroids are not so expensive and should be kept in every medical setting, including private offices. In spite of this fact, only 56% of the private working dentists keep epinephrine ready in their offices.
Corticosteroids have a delayed onset of action and do not reverse the cardiovascular effects of anaphylaxis and should not be used instead of epinephrine and H1 antihistamines.1,8 But, corticosteroids have been accepted as the first-line choice drug in the management of anaphylaxis by some of the responders from our study group.
Atopic diseases, such as asthma and allergic rhinitis are not a risk factor for local anaesthetic sensitivity.12 In spite of this fact, many patients with asthma and other atopic diseases are referred to allergy clinics by the dentists for evaluation for LAs allergy.
In conclusion: Most dentists who may encounter, although rarely, patients with anaphylaxis in their daily practice do not seem to be aware of this emergency situation and the developments in this field in recent years. Therefore, diagnosis and treatment of anaphylaxis should take place more commonly in the courses and congresses of dentists.
Conflict of interestThe authors have no conflict of interest to declare.