Our aim was to assess the prevalence and associated risk factors of common hypersensitivity reactions to drugs in the adult population, for which limited data are available.
MethodsThe data consisted of 1052 questionnaires obtained from adults. The questionnaires consisted of questions on immediate-type hypersensitivity reactions induced by drugs (itching, skin rash/hives, angio-oedema, shortness of breath, hypotension, and loss of consciousness). The questionnaire added knowledge on pyhsician’s diagnosis of asthma, allergic rhinitis, eczema, and other chronic systemic diseases.
ResultsThe prevalence of self-reported drug hypersensitivity reactions was 11.8% for all reactions. Hypersensitivity reactions to analgesics were the most common (37.2%) followed by antibiotics (24.2%). Multivariate analysis showed that female gender (Odds Ratio (OR) 95% Confidence Interval (CI) (2.00 (1.25–3.21)), pyhsician-diagnosed allergic rhinitis (3.03 (1.64–5.59)), and eczema (3.22 (1.87–5.53)) were associated with any type of drug hypersensitivity reactions. Itching was associated with allergic rhinitis (4.50 (2.06–9.81)) and eczema diagnosis (4.24 (2.14–8.64)). Skin rash/hives were associated with female gender (2.67 (1.24–5.74)), allergic rhinitis (4.57 (1.99–10.05)), and eczema (5.36 (2.65–10.84)). Angio-oedema was higher in females (5.74 (1.69–18.5)). In addition, eczema (2.87 (1.12–7.32)) and systemic hypertension (2.60(1.03–6.10)) were associated with angio-oedema. Shortness of breath was only associated with ever asthma diagnosis (6.59 (2.09–20.83)). Factors associated with loss of consciousness were female gender (5.56 (1.27–24.30)), allergic rhinitis diagnosis (4.76 (1.73–13.14)), and systemic hypertension (2.74 (1.02–7.41)).
ConclusionThe study showed that females and subjects with allergic diseases and hypertension were more susceptible to drug hypersensitivity reactions.
Hypersensitivity reactions to drugs are one of the common problems in the general adult population. Despite developments in the area of allergy in recent decades, data on the prevalence and the related factors of hypersensitivity reactions to drugs in outpatient population remain sparse. Most of the reports on drug reactions focused on in-patient cases, whereas drug hypersensitivity reactions have been reported to affect more than 7% of the general population.1 Proposed risk factors for adverse drug reactions were age over 45, between 1 and 4 years, and female gender.2 In a previous study, drug allergy prevalence was found to be 7.8% in a general adult population.3 Among other conditions, atopy was reported as a risk factor for both non-steroidal anti-inflammatory drugs (NSAIDs) and antibiotic allergy.4,5 Data of 411,543 subjects from a medical record review showed a 22.4% prevalence rate of drug allergy.6 Penicillins and sulfa drugs among antibiotics were reported to have higher incidence of reactions.6,7 There are no data on drug hypersensitivity reactions in the outpatient adult population in our country. The present study aimed to assess the prevalence and related risk factors of immediate type hypersensitivity reactions to drugs in a general adult population.
MethodsThe study population consisted of 1052 people 18 years old or older, living in the urban area of Eskisehir, which is a city in the inner-western part of Anatolia, Turkey. The study was cross-sectional and the study subjects were randomly selected from family health centres. Such health centres have approximately 2000–3000 registered individuals in a given residential area of the city. We chose five distant family health centres serving different residential areas to obtain wide-scale information. Information was collected by family doctors with interviews using a structured questionnaire prepared prior to the study. The test-retest repeatability of the questionnaire was determined in a group of 30 patients and healthy subjects who filled out the questionnaire two to three weeks apart.
The questionnaire consisted of questions on immediate-type hypersensitivity reactions induced by drugs (itching on the skin, skin rash or hives (urticaria), swelling of the lips, tongue, eyes or face, angio-oedema, shortness of breath, hypotension, loss of consciousness or coma following drug intake without any other reason), the name of the culprit drug, and time of the reaction.
The questionnaire added additional knowledge on the pyhsician’s diagnosis of allergic diseases, asthma, allergic rhinitis, and eczema. Asthma, allergic rhinitis, and eczema information was based on self-report of having ever been diagnosed by a doctor. Current asthma was accepted as asthma diagnosis within the past 12 months. Questionnaires also added demographical data as well as additional data on the diagnosis of other frequent chronic systemic diseases (heart disease, diabetes mellitus, goitre, systemic hypertension, and others if any) The study was approved by the local ethics comitee and the subjects gave informed consent for the study.
Statistical analysisValues are expressed as mean±SD (standard deviation). Student’s t-test for continuous variables and chi-square test were used to compare variables in the study group. Logistic regression analysis was used to assess the independent association between possible risk factors and drug hypersensitivity reactions for all and each hypersensitivity reaction seperately. The strength of the relationship between risk factors and the reactions was evaluated by calculating adjusted odds ratios (OR) and their 95% CI for all the factors tested. Variables included in the multivariate logistic regression model were selected from those results which had a significance of less than 0.05 in univariate analysis. Age was analysed as continuous covariate. All other variables were coded as categorical covariates which were taken to the model dichotomously. Differences were considered as statistically significant if p<0.05. The data were analysed with SPSS computer program for Windows version 13.0.
ResultsThe mean age of the patients was 41.6±14.6 years. Six-hundred and nineteen subjects (58.8%) were female. The test-retest repeatability of questionnaire was found to be excellent in a group of 30 patients and healthy subjects who filled the questionnaire two to three weeks apart. For the questions related to prevalence of asthma, allergic diseases and drug hypersensitivity reactions, accuracy and Cohen’s Kappa ranged from 86.7% to 100% and 0.65 to 1.0 (for most items it was 1.0), respectively.
The prevalence of self-reported immediate-type drug hypersensitivity reactions was 11.8% (124 subjects) for all type of reactions. Of all patients who reported drug hypersensitivity, 5.2% had itching on the skin (55 subjects), 5.0% had hives or urticarial complaints (53 subjects), 3.5% had angio-oedema (37 subjects), 3.0% had shortness of breath (32 subjects), and 2.0% had hypotension or loss of consciousness (21 subjects). Three-hundred and ninety-three subjects (37.4%) were current smokers. The prevalences of ever physician-diagnosed asthma, current asthma, ever allergic rhinitis, ever eczema, and diagnosis of any chronic-systemic disease were as follows, respectively; 10.2% (107 subjects), 6.6% (71 subjects), 10.2% (107 subjects), 7.8% (82 subjects), and 28.9% (304 subjects). Of the chronic systemic diseases, current prevalence of systemic hypertension was 16.5% (174 subjects), diabetes mellitus was 8.5% (89 subjects), any heart disease was 6.5% (69 subjects), hyperipidemia was 1.7% (18 subjects), and current prevalence of goitre was 1.4% (15 subjects). Other diseases had lower prevalence rates. Ten subjects reported rheumatological and collagen tissue disorders, nine subjects reported neuropsychiatric disease, and two reported other chronic skin disorders. One-hundred and twenty-six subjects (%11.9) had atopic family history.
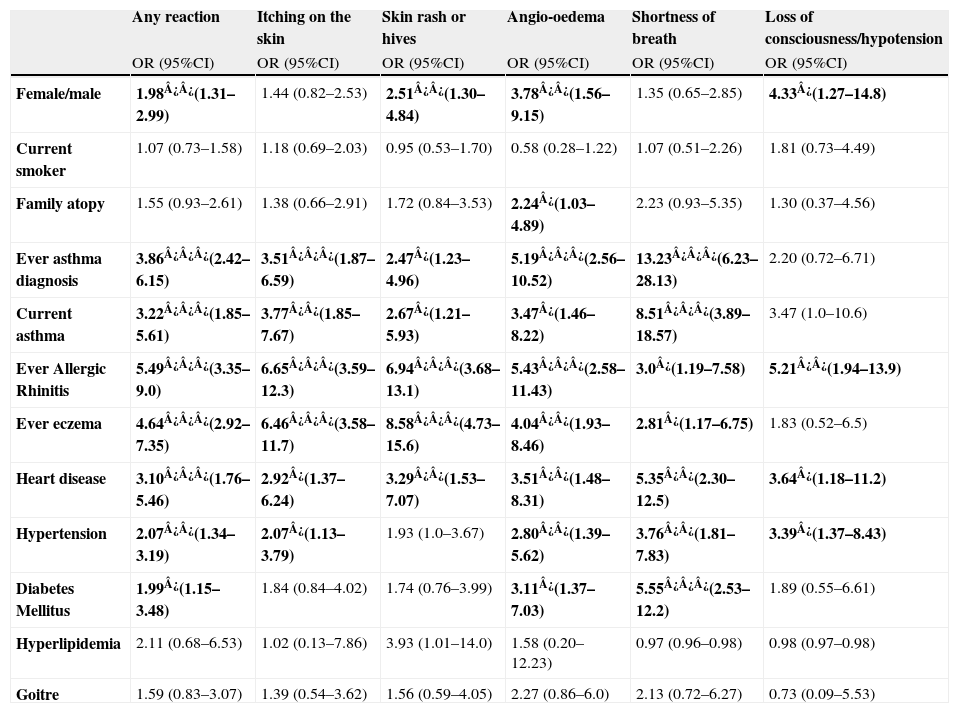
Table 1 shows the associations between immediate-type drug hypersensitivity reactions and possible risk factors in univariate analysis. As shown in Table 1, female gender and diagnosis of asthma, allergic rhinitis, eczema, heart disease, hypertension, and diabetes mellitus were associated with drug hypersensitivity reactions in univariate analysis.
Association between drug hypersensitivity reactions and possible risk factors in univariate analysis
| Any reaction | Itching on the skin | Skin rash or hives | Angio-oedema | Shortness of breath | Loss of consciousness/hypotension | |
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Female/male | 1.98¿¿(1.31–2.99) | 1.44 (0.82–2.53) | 2.51¿¿(1.30–4.84) | 3.78¿¿(1.56–9.15) | 1.35 (0.65–2.85) | 4.33¿(1.27–14.8) |
| Current smoker | 1.07 (0.73–1.58) | 1.18 (0.69–2.03) | 0.95 (0.53–1.70) | 0.58 (0.28–1.22) | 1.07 (0.51–2.26) | 1.81 (0.73–4.49) |
| Family atopy | 1.55 (0.93–2.61) | 1.38 (0.66–2.91) | 1.72 (0.84–3.53) | 2.24¿(1.03–4.89) | 2.23 (0.93–5.35) | 1.30 (0.37–4.56) |
| Ever asthma diagnosis | 3.86¿¿¿(2.42–6.15) | 3.51¿¿¿(1.87–6.59) | 2.47¿(1.23–4.96) | 5.19¿¿¿(2.56–10.52) | 13.23¿¿¿(6.23–28.13) | 2.20 (0.72–6.71) |
| Current asthma | 3.22¿¿¿(1.85–5.61) | 3.77¿¿(1.85–7.67) | 2.67¿(1.21–5.93) | 3.47¿(1.46–8.22) | 8.51¿¿¿(3.89–18.57) | 3.47 (1.0–10.6) |
| Ever Allergic Rhinitis | 5.49¿¿¿(3.35–9.0) | 6.65¿¿¿(3.59–12.3) | 6.94¿¿¿(3.68–13.1) | 5.43¿¿¿(2.58–11.43) | 3.0¿(1.19–7.58) | 5.21¿¿(1.94–13.9) |
| Ever eczema | 4.64¿¿¿(2.92–7.35) | 6.46¿¿¿(3.58–11.7) | 8.58¿¿¿(4.73–15.6) | 4.04¿¿(1.93–8.46) | 2.81¿(1.17–6.75) | 1.83 (0.52–6.5) |
| Heart disease | 3.10¿¿¿(1.76–5.46) | 2.92¿(1.37–6.24) | 3.29¿¿(1.53–7.07) | 3.51¿¿(1.48–8.31) | 5.35¿¿(2.30–12.5) | 3.64¿(1.18–11.2) |
| Hypertension | 2.07¿¿(1.34–3.19) | 2.07¿(1.13–3.79) | 1.93 (1.0–3.67) | 2.80¿¿(1.39–5.62) | 3.76¿¿(1.81–7.83) | 3.39¿(1.37–8.43) |
| Diabetes Mellitus | 1.99¿(1.15–3.48) | 1.84 (0.84–4.02) | 1.74 (0.76–3.99) | 3.11¿(1.37–7.03) | 5.55¿¿¿(2.53–12.2) | 1.89 (0.55–6.61) |
| Hyperlipidemia | 2.11 (0.68–6.53) | 1.02 (0.13–7.86) | 3.93 (1.01–14.0) | 1.58 (0.20–12.23) | 0.97 (0.96–0.98) | 0.98 (0.97–0.98) |
| Goitre | 1.59 (0.83–3.07) | 1.39 (0.54–3.62) | 1.56 (0.59–4.05) | 2.27 (0.86–6.0) | 2.13 (0.72–6.27) | 0.73 (0.09–5.53) |
¿: p<0.05, ¿¿: p<0.01, ¿¿¿: p<0.001, Significant findings are marked in bold.
OR: Odds ratio, CI: Confidence interval.
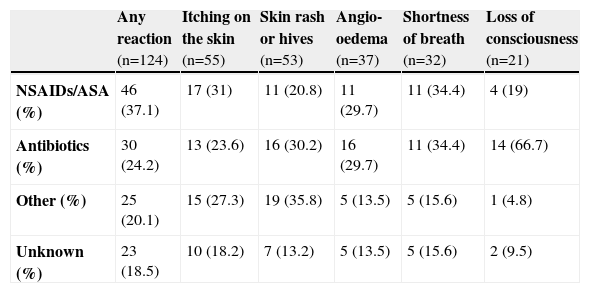
Frequency of reactions to drugs reported by subjects is given in Table 2. Overall, hypersensitivity reactions to NSAIDs or acetylsalicylic acid (ASA) were the most common (37.2% among all reactions). This was followed by antibiotics (24.2%) and other drugs (heart, hypertension, psychotherapeutics, etc….) (20.1%). Among all reactions, the culprit drug was not identified exactly in 18.5% of the reactions, owing to either a recall or discrimination problem. When patients take two or more drugs together they do not report the exact name of the drug which could be the cause of the problem. We classified the name of the drug as ‘unknown’ if the patients gave such a history.
Frequency of reactions to drugs reported by subjects
| Any reaction (n=124) | Itching on the skin (n=55) | Skin rash or hives (n=53) | Angio-oedema (n=37) | Shortness of breath (n=32) | Loss of consciousness (n=21) | |
| NSAIDs/ASA (%) | 46 (37.1) | 17 (31) | 11 (20.8) | 11 (29.7) | 11 (34.4) | 4 (19) |
| Antibiotics (%) | 30 (24.2) | 13 (23.6) | 16 (30.2) | 16 (29.7) | 11 (34.4) | 14 (66.7) |
| Other (%) | 25 (20.1) | 15 (27.3) | 19 (35.8) | 5 (13.5) | 5 (15.6) | 1 (4.8) |
| Unknown (%) | 23 (18.5) | 10 (18.2) | 7 (13.2) | 5 (13.5) | 5 (15.6) | 2 (9.5) |
NSAIDs=Non-steroidal anti-inflammatory drugs, ASA= acetylsalicylic acid.
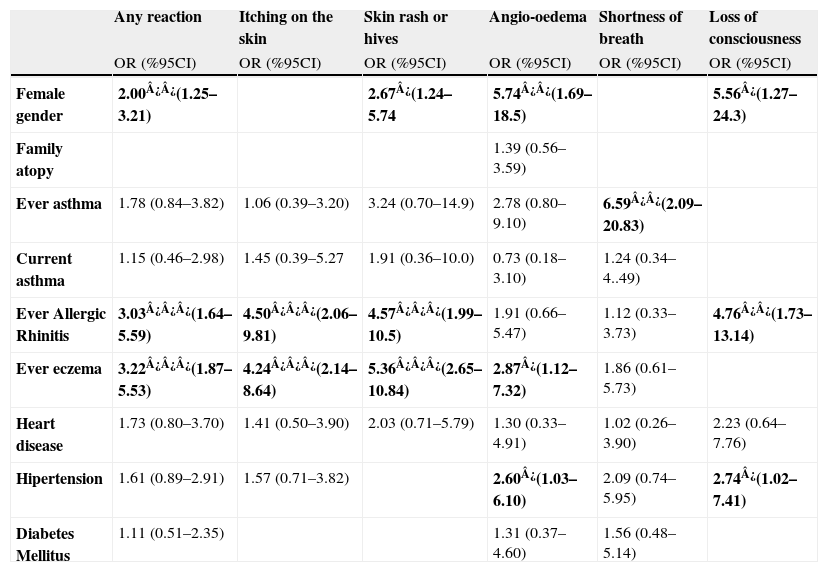
Table 3 shows associations between immediate-type drug hypersensitivity reactions and possible risk factors in multivariate logistic regression analysis. Multivariate analysis showed that female gender (Odds Ratio (OR) 95% Confidence Interval (CI) (2.00 (1.25–3.21)), doctor-diagnosed allergic rhinitis (3.03 (1.64–5.59)), and eczema (3.22 (1.87–5.53)) were associated with any type of drug hypersensitivity reactions. Itching was associated with allergic rhinitis (4.50 (2.06–9.81)) and eczema diagnosis (4.24 (2.14–8.64)). Skin rash/hives were associated with female gender (2.67 (1.24–5.74)), allergic rhinitis (4.57 (1.99–10.05)), and eczema (5.36 (2.65–10.84)). Angio-oedema was higher in females (5.74 (1.69–18.5)). In addition, eczema (2.87 (1.12–7.32)) and systemic hypertension (2.60 (1.03–6.10)) were associated with angio-oedema. Shortness of breath was only associated with ever asthma diagnosis (6.59 (2.09–20.83)). Factors associated with loss of consciousness were female gender (5.56 (1.27–24.30)), allergic rhinitis diagnosis (4.76 (1.73–13.14)), and systemic hypertension (2.74 (1.02–7.41)).
Association between drug hypersensitivity reactions and possible risk factors in multivariate logistic regression analysis
| Any reaction | Itching on the skin | Skin rash or hives | Angio-oedema | Shortness of breath | Loss of consciousness | |
| OR (%95CI) | OR (%95CI) | OR (%95CI) | OR (%95CI) | OR (%95CI) | OR (%95CI) | |
| Female gender | 2.00¿¿(1.25–3.21) | 2.67¿(1.24–5.74 | 5.74¿¿(1.69–18.5) | 5.56¿(1.27–24.3) | ||
| Family atopy | 1.39 (0.56–3.59) | |||||
| Ever asthma | 1.78 (0.84–3.82) | 1.06 (0.39–3.20) | 3.24 (0.70–14.9) | 2.78 (0.80–9.10) | 6.59¿¿(2.09–20.83) | |
| Current asthma | 1.15 (0.46–2.98) | 1.45 (0.39–5.27 | 1.91 (0.36–10.0) | 0.73 (0.18–3.10) | 1.24 (0.34–4..49) | |
| Ever Allergic Rhinitis | 3.03¿¿¿(1.64–5.59) | 4.50¿¿¿(2.06–9.81) | 4.57¿¿¿(1.99–10.5) | 1.91 (0.66–5.47) | 1.12 (0.33–3.73) | 4.76¿¿(1.73–13.14) |
| Ever eczema | 3.22¿¿¿(1.87–5.53) | 4.24¿¿¿(2.14–8.64) | 5.36¿¿¿(2.65–10.84) | 2.87¿(1.12–7.32) | 1.86 (0.61–5.73) | |
| Heart disease | 1.73 (0.80–3.70) | 1.41 (0.50–3.90) | 2.03 (0.71–5.79) | 1.30 (0.33–4.91) | 1.02 (0.26–3.90) | 2.23 (0.64–7.76) |
| Hipertension | 1.61 (0.89–2.91) | 1.57 (0.71–3.82) | 2.60¿(1.03–6.10) | 2.09 (0.74–5.95) | 2.74¿(1.02–7.41) | |
| Diabetes Mellitus | 1.11 (0.51–2.35) | 1.31 (0.37–4.60) | 1.56 (0.48–5.14) |
¿: p<0.05, ¿¿: p<0.01, ¿¿¿: p<0.001, Significant findings are marked in bold.
OR: Odds ratio, CI: Confidence interval, adjustment was made for age.
The present study reported the prevalence of immediate-type hypersensitivity reactions and related risk factors in a Turkish population. Any type of life-time reactions to drugs was reported as 11.8% in our population. Prevalence of other type of reactions were 5.2%, 5.0%, 3.5%, 3.0%, and 2.0%, respectively, for itching on the skin, skin rash or hives, angio-oedema, shortness of breath, and loss of consciousness. NSAIDs and antibiotics were responsible for most of the reactions as confirmed by previous population-based studies.8 In addition, they tended to have more systemic reactions such as shortness of breath and loss of consciousness in the present study. Other drugs (cardiovasvular agents, psychotherapeutics, gastrointestinal etc…) were mostly responsible for the skin manifestations.
Similar to the previous studies, we found that female gender was a risk factor for most of the reactions.2,6 Family history of drug allergy has been suggested as a risk factor for the patients with penicilin allergy.9 Our study did not show a relationship between family history of allergic diseases, including drug allergy. Ever asthma diagnosis in the present study was associated with shortness of breath as a manifestation of drug hypersensitivity supporting that asthma is an aggrevating factor for such adverse drug reactions.10 Similar to our study, a previous study consisting of 187 patients with drug-induced bronchospasm reported asthma and atopy as risk factors and NSAIDs and anti-infectious agents for the most common causes of this manifestation.11 We found significant association between drug hypersensitivity reactions and diagnosis of allergic rhinitis and eczema supporting other allergic conditions as risk factors for drug hypersensitivity reactions.4 Interestingly, diagnosis of eczema was associated with skin manifestations of drug reactions suggesting that prior skin sensitisation might be a predisposing factor for drug-related skin reactions; as described previously for drug-induced urticarial lesions after exposure to aspirin and other NSAIDs in chronic urticaria patients.12 We interrogated for common chronic systemic diseases which could be related with drug reactions either by predisposing effects of diseases or the medications that were administered to treat the underlying disease or its complications. Althogh NSAIDs and antibiotics were the most frequent causes of angio-oedema as expected, among risk factors, hypertension was found to be associated with increased prevalence of angio-oedema. This result is supported by a previous study which showed that increasing rates of angio-oedema hospitalisations were associated with hypertension.13 One of the reasons for the association between drug-induced hypersensitivity reactions and systemic diseases may be medications that are used to treat the diseases. In recent decades, angiotensin converting enzyme inhibitor drugs have played an important role in hypertension treatment. Pathophysiologically, angiotensin converting enzyme inhibitor drugs are well-known causes of angio-oedema.14 In addition, ingestion of aspirin or NSAIDs with angiotensin converting enzyme inhibitors has been shown to cause angio-oedema, which was not present when patients were taking angiotensin converting enzyme inhibitor drugs alone.15 Reporting angio-oedema mostly after taking NSAIDs and antibiotics in the present study suggested to us that association between this manifestation and hypertension might be because of the medications such as angiotensin converting enzyme inhibitor drugs. Another aggravating factor for drug hypersensitivity reactions is the beta-blocking agents mainly used in the treatment of cardiovascular diseases, which are thought to be a possible factor for the association of drug reactions and hypertension.10 Other systemic diseases such as heart disease, diabetes mellitus, and goitre were not associated with drug hypersensitivity reactions in multivariate logistic regression analysis in the present study. Because of small numbers of subjects having other chronic-systemic diseases such as kidney, liver disease or collagen tissue disorders, they were not included in the analysis.
A limitation in this study might be some unpredictable selection or recall biases, which could have originated from the subjects. Patients may report those symptoms that they considered as important and can make a selection bias. To diminish this effect we did not use the terms ‘allergy’ or ‘hypersensitivity’ for the interviews because most of the people in Turkey do not know the term ‘hypersensitivity’ and may use the term ‘allergy’ to explain any type of drug reaction including side effects. Instead, we asked for the most common and distinguishable hypersensitivity reactions following drug intake. There may be some recall bias by the people in cross-sectional studies. Considering that prevalences of current asthma and systemic diseses such as hypertension and diabetes mellitus were very similar to the previous studies, such biases can be accepted as low.16,17
The present study was the first that demonstrated the prevalence and associated risk factors of immediate type drug hypersensitivity reactions in a Turkish adult population. Female gender, asthma, allergic rhinitis, eczema diagnosis, and presence of systemic hypertension were found to be as risk factors for these types of drug hypersensitivity reactions. Those risk groups should be followed closely with regard to the use of such drugs.
Conflict of interestThe authors have no conflict of interest to declare.