Perimenstrual asthma (PMA) has been documented in 30–40% of asthmatic women; however, there have been few epidemiological investigations of PMA in practice.
ObjectivesDetermination of the prevalence of perimenstrual asthma in a sample of female Saudi asthmatic patients, and to study the relation of PMA to asthma severity, aspirin-induced asthma and to other allergic co-morbidities.
Study designData were analysed from all female asthmatic patients followed up in the unit from January 2008 to May 2009 who were not pregnant, not on oral contraceptive pills, not menopausal, nor had had a hysterectomy. They were asked about exacerbation of their asthma state regarding worsening of symptoms, need for more rescue medications and even visits to emergency room just before or in the first days of menstruation, or both. Moreover, relation with aspirin-induced asthma and other associated allergic co-morbidities recorded in their medical files with prevalence of PMA was reported.
ResultsThe prevalence was found to be 8.2%. Asthma severity was found to be significantly related to PMA (p<0.0001). Aspirin-induced asthma and allergic co-morbidities were more prone to occur in cases with PMA than other studied asthmatics.
ConclusionWe have found a low prevalence of PMA in Saudi women of fertile age compared to other studies published. Study findings support the hypothesis that PMA is related to asthma severity.
The incidence of asthma has a strong sex bias.1–3 Asthma not only occurs more frequently among adult women in the reproductive years of their lives, but adult females also exhibit a more severe form of asthma.4–6 Gender differences in severity may have their origin in differences in the pathogenetic mechanisms, variations in pathophysiology and differences in response to treatment. The information available is too scant to allow any meaningful hypothesis to be developed regarding the reasons behind the gender differences in asthma.7
It has been recognised that many women have the nadir of their control just a few days before and/or during the menstrual periods. This presentation of asthma in females has been described as “perimenstrual asthma” (PMA).7 One report mentioned that there were significantly more near fatal asthma episodes on the first day of menstruation. However, another study reported that emergency room visits for acute asthma were most common during the preovulatory phase (from 5th day to 11th day).8,9
In studies carried out in Western industrialised countries, 30–40% of female asthmatics report perimenstrual deterioration in their condition, while in studies carried out in Japan the prevalence rate was 11%.7,10–14
Because bronchial asthma is one of the most common diseases, the management of bronchial asthma, including medical interviews, can play an important role in actual clinical settings. During the medical interview, it is very important for the physician to note predictive factors of asthma exacerbation, such as menstruation.7
Until now no epidemiological study has reported the prevalence of PMA in Saudi Arabia. Thus, the purpose of this study was to report the prevalence of PMA and its relation to asthma severity and other allergic co-morbidities.
Patients and methodsThe study was conducted in accordance with the ethical principles of the Declaration of Helsinki and Geneva Declaration of the World Medical Association. During the period from January 2008 to May 2009 all female asthmatics aged 17–54 years who were followed up in the “Allergy Unit” in Taif University were enrolled in this study. Those who were pregnant, on oral contraceptives, postmenopausal or following hysterectomy were excluded.
Patients medical files included direct questions regarding worsening of their respiratory symptoms (i.e. increase in asthma symptoms severity, increased drug demands that may require visiting the emergency room) within a few days before menstruation, during the first few days of the menstrual period, or both. Even those who were sceptical were asked to report to their treating doctor in their next monthly follow-up visit. Additionally, other diagnosed allergic co-morbidities were reported. Mild, moderate, and severe asthma diagnosed according to guidelines15 were encountered in five (21.7%), two (8.7%), and 16 (69.6%) patients in the PMA group, respectively, and in 150 (58.4%), 43 (16.7%), and 64 (24.9%) in the non-PMA group, respectively.
No pulmonary function study was performed to those cases before their menstrual period as it was not feasible for every patient to monitor the peak expiratory flow rate (PEFR) at home and some even showed reluctance to perform it.
Statistical analysisStatistical analyses were performed using the computer-based analysis program SPSS version 15.0 (Chicago, USA). Statistical significance was defined as a p-value <0.05. Prevalence rate of PMA, as well as odds ratio and 95% confidence intervals were calculated. The comparisons of some indices and other variables in the selected sub-groups were carried out by Chi-square for independent variables.
ResultsData regarding allergic co-morbidities and worsening of symptoms, need for more rescue medications and even visit to emergency room just before, in the first days of menstruation, or both of all female asthmatic patients followed up in the Allergy unit in Taif University from January 2008 till May 2009 who were non pregnant; not on oral contraceptive pills; not menopausal; nor had had hysterectomy, were analysed from patients’ medical files. Thus 280 eligible women from 315 (88.8%) with average age of 30.5 years old were included in this study.
They reported early onset of menarche (11–12 years old) and asthma starting during childhood. Only 23 asthmatics (8.2%) reported symptoms matching with PMA, however, none suffered from symptoms severe enough to require emergency department visits. Those who were known to have asthma exacerbations related to menstruation were allocated to the PMA group; those who were not were allocated to the non-PMA group.
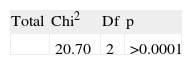
Table 1 shows that PMA was more commonly encountered the more severe the asthma, with a Chi-square 20.7 and Df=2 (p<0.0001).
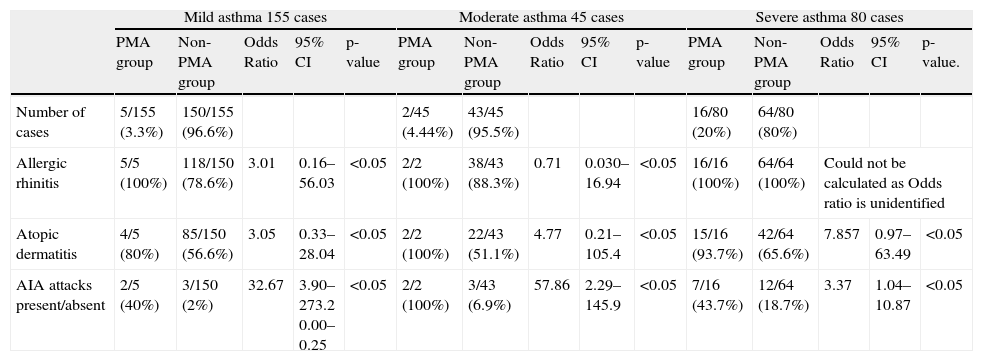
Table 2 shows the prevalence of allergic co-morbidities, AIA attacks, and family history of allergy according to asthma severity in PMA and non-PMA groups. All severe asthmatic cases suffer from allergic rhinitis. PMA is more frequent in severe asthmatics (3.3% of all mild asthmatic cases, 4.44% of all moderate asthmatic cases and 20% of all severe asthmatic cases). PMA is related to AIA (40% of all mild asthmatic cases, 100% of all moderate asthmatic cases and 43.7% of all severe asthmatic cases).
Prevalence and associated odds ratio and 95% confidence interval of allergic co-morbidities, AIA attacks and family history of allergy according to asthma severity in PMA and non-PMA groups
| Mild asthma 155 cases | Moderate asthma 45 cases | Severe asthma 80 cases | |||||||||||||
| PMA group | Non-PMA group | Odds Ratio | 95% CI | p-value | PMA group | Non-PMA group | Odds Ratio | 95% CI | p-value | PMA group | Non-PMA group | Odds Ratio | 95% CI | p-value. | |
| Number of cases | 5/155 (3.3%) | 150/155 (96.6%) | 2/45 (4.44%) | 43/45 (95.5%) | 16/80 (20%) | 64/80 (80%) | |||||||||
| Allergic rhinitis | 5/5 (100%) | 118/150 (78.6%) | 3.01 | 0.16–56.03 | <0.05 | 2/2 (100%) | 38/43 (88.3%) | 0.71 | 0.030–16.94 | <0.05 | 16/16 (100%) | 64/64 (100%) | Could not be calculated as Odds ratio is unidentified | ||
| Atopic dermatitis | 4/5 (80%) | 85/150 (56.6%) | 3.05 | 0.33–28.04 | <0.05 | 2/2 (100%) | 22/43 (51.1%) | 4.77 | 0.21–105.4 | <0.05 | 15/16 (93.7%) | 42/64 (65.6%) | 7.857 | 0.97–63.49 | <0.05 |
| AIA attacks present/absent | 2/5 (40%) | 3/150 (2%) | 32.67 | 3.90–273.2 0.00–0.25 | <0.05 | 2/2 (100%) | 3/43 (6.9%) | 57.86 | 2.29–145.9 | <0.05 | 7/16 (43.7%) | 12/64 (18.7%) | 3.37 | 1.04–10.87 | <0.05 |
Mechanisms explaining sex differences in asthma pathophysiology remain largely unexplored and little attention is paid to differences in treatment responses between men and women. Yet studies investigating these aspects of sex differences in asthma are essential for developing optimal treatments for both men and women.16
It is well known that some female asthmatic patients experience aggravation of asthma symptoms during the premenstrual or menstrual phase of their cycle. The term “premenstrual asthma” describes those women with nadir control of their asthma symptoms just a few days before the menstrual periods. However, as some patients with cyclic variations in symptoms may experience exacerbation of the symptoms at other times during a menstrual cycle, other terms have been used to describe this phenomenon, including “menstrual-linked asthma”, “menstrual-associated asthma” and “perimenstrual asthma”.17 Perimenstrual asthma (PMA) can be severe and even life-threatening with fatal cases often reported. Therefore, prevention and treatment of PMA is of great interest.2,18–20
In this study, there was an interesting discrepancy between the prevalence rate recorded in previous studies performed in western countries (30–40%,), and in Japan (11.3%),1 and that reported in this study (8.21%). However; in accordance with the results of the study by Forbes et al.,21 which also used self-reports of exacerbated symptoms in response to a questionnaire to define PMA, a similar rate of 8.2% was observed. This suggests that the observed differences in the incidence of PMA are not due to race, but to the study design.
Since this study only addressed limited clinical features of asthma, thus comparison with the clinical characteristics of PMA that were discussed previously seems difficult, namely, the associations with duration and cycle of menstruation, and PMA-specified symptoms. However, as shown in Table 1, patients of the PMA group suffered from more severe asthma than patients in the non-PMA group, similar to results from previous studies.11,14,17 Among the clinical features of PMA outlined in this study, were the interesting findings of a significantly greater proportion of AIA among patients in the PMA group (68.8%) compared with the non-PMA group (7%). This may indicate a significant association between PMA and AIA. Lower percentage was reported by Suzuki et al.7 with a prevalence rate of 25.5% in the PMA group and 8.4% in the non-PMA group. Nevertheless, their study similarly reported higher prevalence rate with the PMA group. As leukotriene antagonists have been reported to be effective in asthma control in both PMA22 and AIA,11,22 thus these results may indicate that a shared dysfunction of leukotriene and prostaglandin metabolism may be involved in PMA and AIA.7
One limitation to this study was the possibility that perimenstrual and preovulatory presentations with acute asthma may have been increased by the patients’ concomitant ingestion of aspirin or analgesics, which may worsen asthma was not tested on depth. However, Forbes et al. reported that there was no association between the use of non-steroidal anti-inflammatory drugs and PMA.21
Unfortunately, in the literature there were no previous studies associating PMA with other allergic co-morbidities to be compared with, however, this adds strength to the current study.
This study has other potential limitations regarding the lack of hormonal and functional documentations; which could have evidenced more cases. However, the objective evaluations of airway function during the menstrual cycle in women with stable asthma have yielded inconsistent results.15 Moreover; the self reporting of PMA by the patients without sufficient knowledge may be a leading cause of the reported low rate of PMA, which may not be an accurate representation of the actual incidence of the disease. Despite these potential limitations, this study is the first to be conducted in the Middle East and could be a step towards actual estimation of PMA in the Arab countries to be compared with the rate in Western countries, aiming at the possible finding of racial, genetic or other aetiology responsible for this discrepancy in the prevalence rates.
Conclusion and recommendationIn summary, although the prevalence rate of PMA was much lower than in previous studies, severity of asthma was markedly related to PMA, similar to other conducted studies. These data may suggest that factors of asthma severity are sex-dependent and that hormonal factors could be involved in the severity of asthma. The clinical similarity of PMA to AIA in this study may also provide a new insight into the mechanism of PMA.
Taking into account the worldwide increasing prevalence of asthma and the fact that nearly 40% of women may suffer from PMA, it should therefore be considered as a major management problem in asthma that necessitates better understanding of its various aspects. This is especially so as there are many issues in PMA which are not yet well understood, besides the several contradictions in the literature. Moreover, the consequences of PMA on patients’ quality of life and relation with other allergic co-morbidities need to be studied.
Conflict of interestThe author does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. There was no funding source to report.
I would like to thank all those who helped in the establishment of the “Allergy Unit”, in Taif University — the first in all Saudian Universities. I thank the patients who agreed to participate in this study, for sharing their time, experiences and opinions with me.