To the Editor:
Migration studies provide information on the role of environmental factors on the development of atopy and respiratory disease. International studies provide strong and objective evidence for an association of atopic disease with westernisation.1 A metaanalysis has shown higher rates of asthma in immigrants. Immigrants moving to allergy prevalent countries have generally more allergy and asthma comparing both with natives, but also with respect to the prevalence in their countries of origin.2
It has been postulated that parasite-burden in developing countries is inversely associated with atopy and asthma.3,4 Furthermore, climatic conditions for a high prevalence of geohelminths parallel those for growth of different house dust mite (HDM) species. Up to now, most immigrant studies on an epidemiological background have addressed prevalence rates of asthma or allergy without taking into account the specific sensitisation to different aeroallergens.
In our study region, HDM sensitisation is infrequent due to a predominantly dry climate. Otherwise, many immigrants come from tropical or subtropical regions, where HDM are the predominant sensitising allergens. We hypothesise that immigrants from these countries, although developing allergic respiratory disease after migrating, could be sensitised to different aeroallergens in comparison to natives. The aim of this study was therefore to compare the sensitisation profile of allergic immigrants proceeding from helminth endemic developing countries regions, with native patients of our region, in which no significant endemic helminth infection is known.
In a mainly dry region (Madrid, Spain), we performed a cross-sectional study of 49 consecutive adult immigrant patients from South-America and the Philippines who attended our Allergy Service for an allergological evaluation of rhinoconjunctivitis or bronchial asthma (RCBA). Patients were included if they had interview based typical rhinitis or rhinoconjunctivitis symptoms and/or bronchial asthma for at least one year. One hundred native RCBA patients in the same age range of 23–63years served as control group. We asked for the age of migration and onset of RCBA symptoms. Patients were assessed for seasonal and/or perennial symptoms. They could be included in both groups, if seasonal exacerbation of perennial symptoms were present.
Skin Prick Tests (SPT) were performed against house dust mites (HDM, Dermatophagoides pteronyssinus, D. farinae, Tyrophagus putrescentiae), animal dander (cat, dog), 5 pollen mixtures of grass, tree and weed pollen and mould (Alternaria alternata, Cladosporium herbarum). SPT was performed in standard technique and was considered positive with a mean wheal diameter of ≥ 3 × 3mm. Histamine at 1 % concentration and saline solution 0,9 % (NaCl) were positive and negative controls.
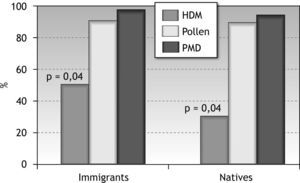
SPT data were analysed separately for HDM, pollen and PMD (group of non-HDM allergens: pollen, mould or dander). Statistical analysis was performed using SPSS 15.0 for Windows Version (SPSS Inc.).
ANOVA and Chi-Square-Test were used for evaluation of significance of means and percentages, respectively.
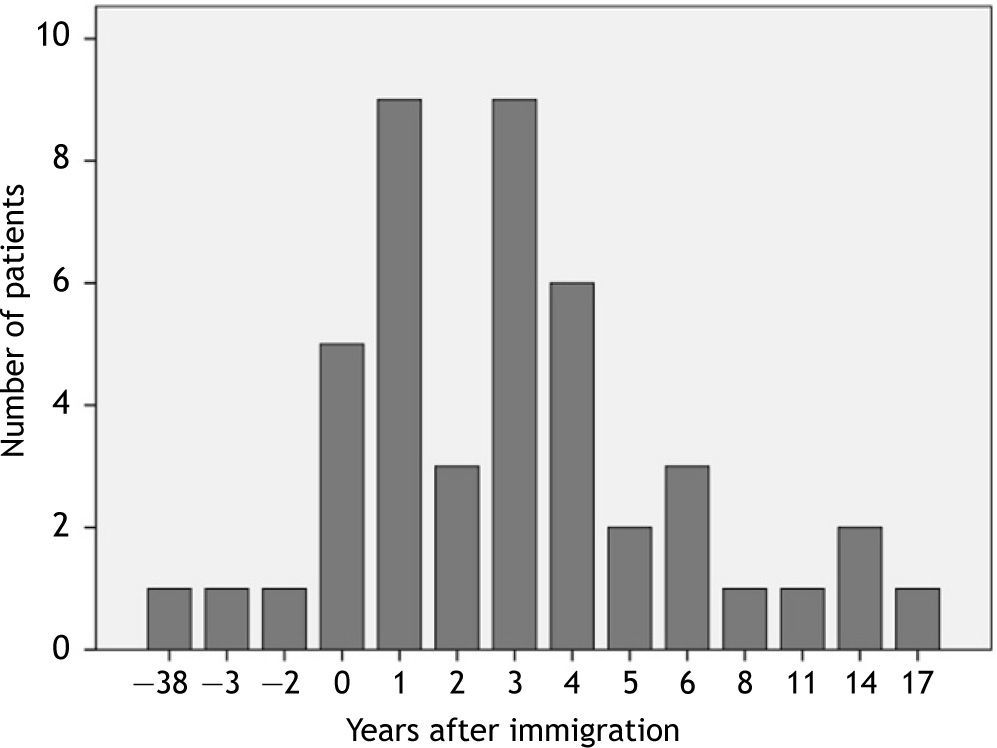
Forty-four of 49 patients began to suffer RCBA after migrating to our region with a mean latency of 3.8 ± 3.8years (Fig. 1). Mean age of symptoms initiation was 36.3 ± 11.0years and 30.6 ± 8.8years in the control group (p = 0.005). 75 % were female in immigrant patients and 68 % in natives (n.s.). Overall SPT reactivity was higher in immigrants than in native patients (95.5 % versus 75.0 %; p = 0.002). Immigrants claimed perennial symptoms in 25 % (natives 56 %, p < 0.0001) and seasonal symptoms in 75 % (natives in other 50 %, p < 0.004).
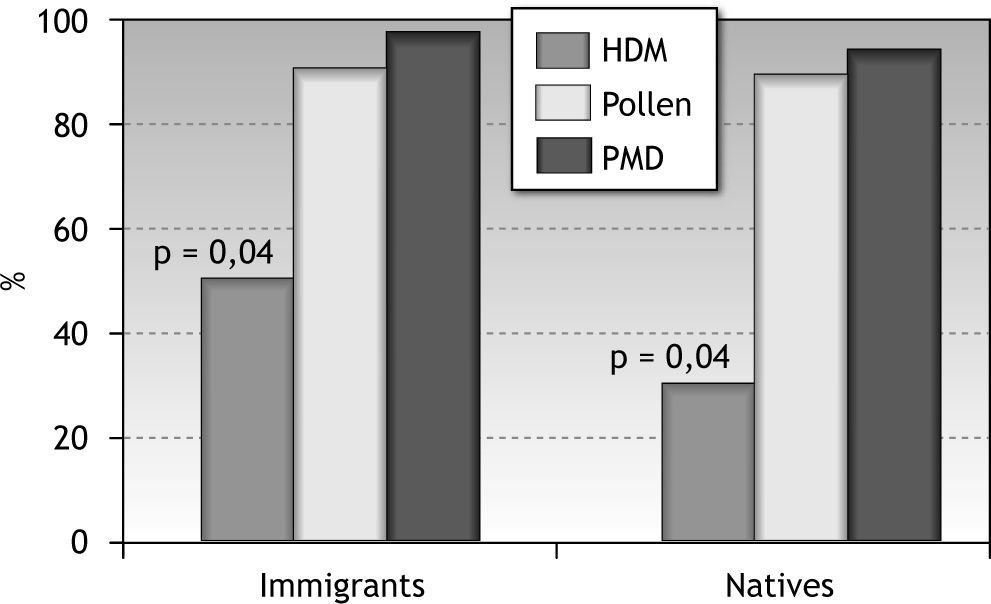
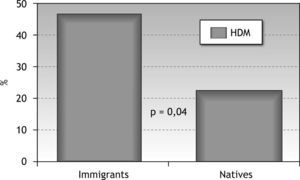
The following prevalence rates are described only for sensitised patients with RCBA (in migrants those who initiated their symptoms after migration (n = 42)): Rhinoconjunctivitis without bronchial asthma was present in 45.2 % of immigrants and 41.3 % of natives (n.s.). HDM sensitisation was significantly higher in immigrant patients (50 % versus 32 %; p = 0.04) (Fig. 2). Pollen sensitisation rate was similar in immigrants and natives (90.5 % and 90.7 %, respectively, p = 0.6). Sensitization against PMD was also similar (97.6 % and 96 %, p = 0.5).
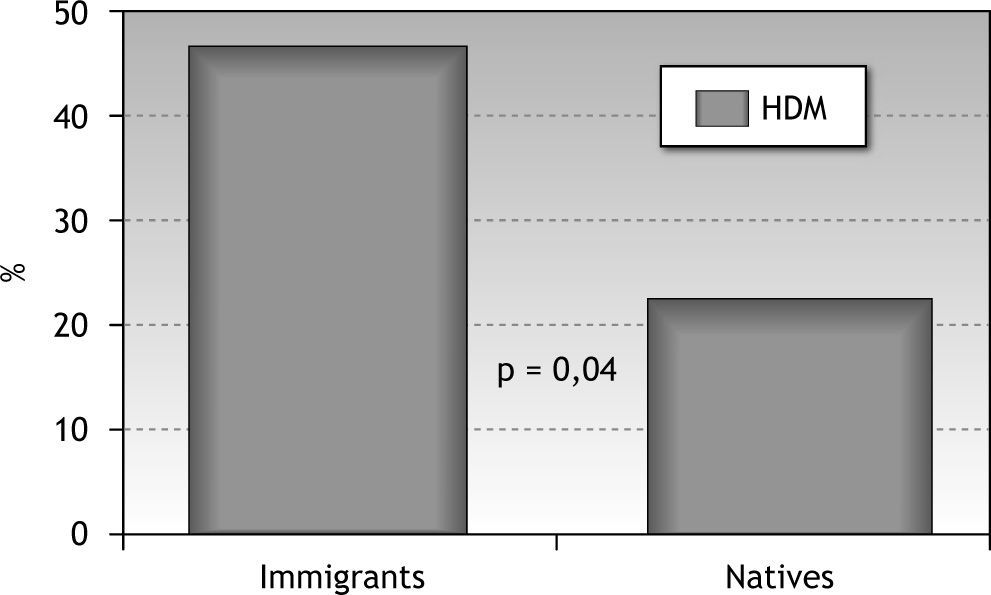
Fourteen of 30 (46.7 %) immigrant patients with pollen sensitisation associated only seasonal RCBA were also subclinically sensitised to HDM (only 21.7 % of native patients with seasonal pollen sensitisation associated RCBA; p = 0,001) (Fig. 3).
This study was not designed to gain information about prevalence rates of allergic respiratory disease of immigrants neither compared with the population in their countries of origin, nor with respect to the native population. However, our results corroborate some data of previous epidemiological reports and enrich our understanding on the different possible sensitisation profiles due to new or missing environmental factors.
Nearly all adult immigrants began to suffer rhinoconjunctivitis or bronchial asthma (RCBA) after migrating, a fact that corroborates results by other studies5. This fact, together with the elevated age of onset of symptoms has already been described previously and favours the hypothesis of environmental factors leading to the appearance of allergic symptoms6. We do not know the possible sensitisation profile of these immigrants before their onset of symptoms, or even before migrating. Pollen sensitisation reaches 90 % in patients with RCBA, both in immigrants and natives. The higher HDM prevalent rate in immigrants compared to our age-matched control group attracts attention, but even more so does the fact that immigrants show a more than twice higher sensitisation rate against HDM, if only patients with seasonal RCBA were analysed. Due to geographic and climatic conditions, these results are to be interpreted in the special circumstance of a low prevalence of HDM sensitisation in Central Spain. Whereas HDM sensitisation is associated with perennial asthma7, seasonal RCBA is mainly related to pollen sensitisation. Therefore, the mentioned subanalysis gives us information about very high subclinical sensitisation prevalence against HDM in immigrants.
If we search for possible explanations, we cannot rule out a possible selection bias, such as different HDM prevalence favouring living conditions. Taking into account the low HDM allergen prevalence in our region and the relatively short time interval between migration and the first symptoms, this possibility seems unlikely. Thus, if we search for environmental factors, we should look at the country of origin: due to climatic conditions, and the fact that most immigrants are those who can afford the step to migration and proceed from urban or semi-urban regions, contact with sufficient sensitising HDM is a possibility, as is the fact that other arthropods, like cockroaches, or geohelminths with known cross-reactivity with HDM could have sensitised our study population in their country of origin8. This hypothesis is tempting, as it has been shown that a high parasite burden in developing countries is not only inversely associated with asthma and atopy, but otherwise even in the case of sensitisation, high intensity parasite infection is able to inhibit the risk of wheeze3,9.
Early childhood infections outside the US seem to protect against asthma in a cross-sectional survey comparing native and foreign born immigrants10. However, immigrants from developing countries can be asymptomatic, even showing positive SPT, but moving to industrialised centres adds a new environmental exposure, to which immigrants do not seem to be protected2. Pollen sensitisation in developing countries is not as high as HDM sensitisation, but the inverse situation is given in our area.
Thus, it seems that immigrants have been immunologically primed for HDM or equivalent cross-reacting arthropod-helminth allergens, but possibly environmental and lifestyle factors prevented their expression11. In this respect, if environmental aspects of allergic disease in migrants are discussed, also those missing environmental factors should be addressed in future studies. In this study we did not assess prior helminth exposure. It is clear that having evidence of this would strengthen the analysis and is an area of future research. A previous study has shown an increase in skin reactivity to newly acquired allergens following antihelminthic treatment in migrants from Ethiopia12. Together with new environmental factors, which are able to enhance sensitisation, like a polluted atmosphere, this could be the cause for the appearance of new respiratory symptoms in a subgroup of our migrant patients. A previous report proposed a differential atopy evaluation when dealing with the relationship between atopy and parasites13. Thus, arthropod-parasite related sensitisation, which includes HDM sensitivity, in our migrant population could have a different clinical outcome compared to pollen or other aeroallergen sensitisation, as is shown by our results.
This reasoning is not contrary to the possible implication of genetic factors. Evidence supports an increased susceptibility to allergy and asthma among populations with tropical ancestry14. The differences in asthma prevalences due to ethnicity could thus be due to a common genetic factor that predisposes to both allergy and resistance to infection15.
Summarizing, the high prevalence of HDM sensitisation of our migrant patients could be due to previous subclinical sensitisation in their tropical and subtropical countries with more favourable conditions for the presence of different mite species, but other factors have to be taken into account, such as genetic factors, the elevated burden of microbial burden or the higher prevalence of geohelminths, which in turn could be responsible for possible cross-reactive sensitisation against HDM.