A clinical problem in patients who have experienced an immediate-type allergic reaction to a medication is represented by how long the persistence of the IgE-mediated allergic sensitisation is. It seems to be different for every drug, ranging from a period of 8–10 years in case of the beta-lactams1 to up to 29 years for the neuromuscular blockers.2 Systemic glucocorticoids, as widely reported in literature, can induce immediate-type hypersensitivity reactions,3 although they are underestimated in clinical practice yet. Currently, the persistence of allergic sensitisation to systemic corticosteroids is unknown, because of the limited number of patients who experience immediate-type hypersensitivity reactions towards these drugs. For that reason, probably, a similar follow-up study has never previously been performed. We observed the case of a patient whose clinical history reported two previous anaphylactic reactions immediately after administration of hydrocortisone hemisuccinate occurred 12 years earlier and who still showed the persistence of serum specific IgE to hydrocortisone.
A 76-year-old female patient not atopic, suffering from chronic bronchitis came to our observation for a bronchial exacerbation with cough and moderate dyspnoea. The patient had also a polyarthrosis, treated with frequent non-steroidal anti-inflammatory drugs (NSAIDs) and analgesics courses. Her medical history stated that facial angio-oedematous reactions appeared after taking various non-steroidal antinflammatory drugs such as diclofenac, ketoprofen, paracetamol. The patient, in addition, had been treated since the age of 44 years with hydrocortisone sodium succinate (HC-SS) intramuscularly as needed, for early menopause and occasional blood hypotension crisis.
In 1997, at the age of 64 years, after the administration of that glucocorticoid, the patient exhibited an anaphylactic reaction with hospitalisation. Few months later, a second anaphylactic episode occurred after a further administration of intramuscular HC-SS. After the acute phase, in an Allergy Unit, the patient underwent an intradermal test (IT) with HC-SS and methylprednisolone sodium succinate (MP-SS) at not specified dilutions with a positive response to HC-SS IT only.
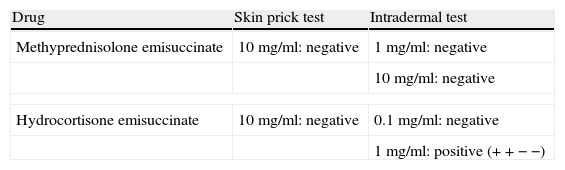
An oral challenge test with nimesulide and an intramuscular challenge test with MP-SS at a dosage of 20mg were carried out, without eliciting any hypersensitivity reaction. One month later, according to the patient's documentations, another challenge test with HC-SS intramuscularly (10mg) was carried out, by provoking a generalised urticarial rash a few minutes after steroid administration. The patient tolerated the oral betamethasone and fluticasone via aerosol. Because the patient asked us to investigate her drug hypersensitivity again, we proceeded to perform skin prick tests (SPT) and IT with extemporaneous commercial injectable preparations of MP-SS (Solumedrol 20mg, Pfizer-Milan, Italy) and HC-SS (Solucortef 100mg/2ml, Pfizer-Milan, Italy) diluted in 0.9% saline with different concentrations as shown in Table 1. Positive and negative controls were histamine dihydrochloride, 10mg/ml and sterile normal saline, respectively. SPT and IT readings were made after 20min to assess the immediate response. Four patients: two atopic and two non-atopic as healthy controls were enrolled and underwent skin tests with HC-SS and MP-SS at the same concentrations with negative results.
To confirm the reaginic pathomechanism of sensitisation to hydrocortisone, the patient's husband, after giving his written consent, accepted to submit himself to a Prausnitz–Kustner (PK) test with his wife's serum.
The patient's serum was diluted and then 0.1ml was injected intradermally into the left forearm of the recipient.
48h later, 0.05ml of HC-SS (at 1mg/ml dilution) was injected intradermally at the same site. As negative control, an intrademal test was performed with the same amount of drug on the opposite forearm. The PK test gave positive result with an erythematous wheal (5mm in diameter) (+ − − −) 20min after the administration, while no reaction appeared on the opposite forearm. The PK test confirmed the persistence of selective IgE to HC-SS 12 years after her previous anaphylactic reactions. Morning serum cortisol dosage (14.7mcg/dl – normal range: 6–30mcg/dl) and serum ACTH (5pg/ml – normal value: <40.0pg/ml) were also carried out before administering a slow intravenously incremental challenge test (ICT) with MP-SS (two doses of 5mg every 30min followed by 10mg aft 30min later and finally 20mg 12h later). Since the intravenous ICT with MP-SS gave a negative result, that steroid molecule (20mg twice/daily) was introduced in patient therapy.
Specific IgE to hydrocortisone and methylprednisolone have been evidenced in vitro by using HC-SS and MP-SS conjugated with human serum albumin,4 but Japanese authors confirmed the presence of specific IgE to corticosteroids through the use of PK test in two selected subjects belonging to a group of seven patients with asthma who had experienced anaphylactic reactions after systemic corticosteroid administration.5 In our case, because the composition of the commercial preparations of MP-SS and HC-SS are identical, the tolerability of methylprednisolone intravenously excluded that the patient had produced an IgE-mediated response against the preservative benzyl alcohol, as previously reported by other authors.6
A decline in the IgE antibody response has been evidenced for some drugs such as chlorhexidine7 and penicillins,1 leading patients to tolerate the drug antigen again,1 while the persistence of specific IgE to hydrocortisone over time could be due, in our opinion, to the endogenous production of cortisol by the body. Lauerma has previously demonstrated that administration of synthetic ACTH in patients with allergic contact dermatitis to hydrocortisone would result in a reactivation of cutaneous lesions, thus suggesting that T cells of sensitised patients recognise as an allergen either endogenous cortisol or cortisol administered orally as a drug in increasing doses.8 Since semisynthetic succinated salts steroids undergo hydrolysis in the body, thus allowing steroid molecule bioavailability for its specific receptor,9 that process could make the drug indistinguishable from the endogenous cortisol amount.
In that way, endogenous cortisol probably contributes to maintain, in our patient, the immunological memory able to induce hydrocortisone specific IgE production, as confirmed by skin tests and PK test. Hydrocortisone allergic sensitisation should be considered lasting lifelong in these patients, but further studies are required to confirm whether such a hypothesis may be applied to other synthetic steroids derived from cortisol.
Ethical disclosureRight to privacy and informed consent. The authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Confidentiality of data. The authors declare that no patient data appears in this article.
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.