In recent decades, the prevalence of allergic diseases has markedly increased worldwide; however, there are still many cases which remain undiagnosed. Epidemiological studies have the potential to elucidate the prevalence and risk factors for these diseases.
ObjectivesThis study aimed at evaluating the capability of a new original non-translated questionnaire in Arabic language to determine the prevalence and severity of these diseases in a sample from Taif citizens. Thus, it could provide a framework as an initial step towards accomplishing the first national questionnaire-based survey study determining the actual prevalence of various allergic diseases in Saudi Arabia.
MethodsA detailed seven-section questionnaire including 143 closed questions covering almost all of the usual and unusual symptoms of various allergic diseases, in Arabic language, was handed out to 1050 subjects, from whom 877 (83.52%) questionnaires were completed; however, 23 questionnaires were discarded as they were not accurately filled in. Thus, 854 (81.33%) were enrolled in this study.
ResultsUrticaria, allergic rhinitis with or without other co-morbidities, and atopic dermatitis were the most prevalent allergic morbidities, however, other allergic diseases could be diagnosed by the aid of the questionnaire. Likelihood ratio-evidenced agreement between diagnosis reached by the questionnaire and that reached by doctor occurred in 50 sample cases (p<0.0001).
ConclusionsThe questionnaire proved its capability in aiding the diagnosis of various allergic morbidities. It evidenced a high prevalence of allergic diseases in Taif city. This is an important health issue which requires strategic application of primary health care facilities to achieve adequate control.
Allergic diseases are common and increasing in prevalence, resulting in morbidity and mortality in all age groups, thus a clear understanding of the spectrum of allergic diseases and the accurate identification of environmental triggers can enable the doctor to recommend optimal allergen specific treatment, thereby minimising morbidity and mortality.1
“Allergy Unit”, in Taif University is the first of its kind in all Saudian Universities. Since its establishment in 2007, the lack of awareness of many allergic patients about the presence of allergic co-morbidities that affected negatively their response to therapy has been noted. Moreover, many cases lacked knowledge about the allergic nature of their long-lasting troublesome symptoms because of misdiagnosis. Thus the Unit has a primary goal of increasing the awareness of Saudian citizens about the benefits of early diagnosis and competent management of various allergic diseases which unfortunately pass undiagnosed for years; years that count for the quality of life of those patients.
In the last few decades, the instruments most used to enable the investigation of population samples have been written questionnaires (WQs), both those applied by trained interviewers and those which are self-applied. Such procedures when standardised and validated locally facilitate temporal and regional comparison of the clinical and epidemiological data obtained.2,3 However, the questionnaires currently available include in their content questions focusing on one or few allergic diseases. This would not be beneficial in a city where the actual magnitude of the problem is unknown.
Therefore the purposes of this study were: (1) elaborate a new original non-translated Arabic language questionnaire in simple, direct and familiar language that could be easily understood and thus self-replied by respondents of all socio-economic and educational status; (2) describe the prevalence and severity of various allergic diseases in a sample of children, adolescents, and adults in Taif city, and to detect any prevalence differences between different age and sex groups; (3) obtain baseline measures to assess future health plans effects on prevalence and severity of these diseases; (4) provide a framework for the first national questionnaire-based survey study to determine the actual prevalence of various allergic diseases in Saudi Arabia that may reveal important risk factors; and (5) provide a questionnaire that could aid family physicians in their clinical evaluation, decisions and needs for referral.
Subjects and methodsStudy sample and sampling methodTaif cityThe study was conducted from April 2008 till March 2009 in Taif, a city at the gates of Mecca, and is located 1700-2500m above sea levels in Saudi Arabia. It is characterised by its dry climate almost all the year round, and cultivation of roses, grapes, grenades, and olives. One characteristic of the city, as with some of the Saudian cities, is that most of its citizens are from tribes which are the original natives of the country.
Sabry's Arabic Questionnaire for Allergy Diagnosis-143(SAQAD-143)An original non-translated Arabic questionnaire (appendix), formed by seven sections, including 143 questions covering most of the usual and unusual symptoms of various allergic diseases was developed. Development was based on international guidelines for these diseases and data from the literature together with the effects on the quality of life.4–11 This study was in compliance with the Helsinki Declaration and the Ethical Principles for Medical Research Involving Human Subjects. It was not financially supported. The questionnaire was either self-applied (by 54% of studied population) or was conducted by face-to-face trained interviewers (by 46% of studied population) in the Allergy unit.
An e-mail allergyunit@yahoo.fr was provided at the end of each questionnaire for further inquires by the studied population.
Questionnaire testingFifty cases selected randomly were first supplied with the questionnaire to fill out and then were interviewed by the senior Consultant in the Unit (not necessarily on the same day), who was blinded to their questionnaire replies. Thereafter, comparison was performed between the diagnosis reached by the aid of the questionnaire and that reached by the Consultant. This allowed for questionnaire testing, to help to determine problems caused by the respondent's inability or unwillingness to answer the questions; to discover poor wording or ordering of questions; to identify errors in the questionnaire layout and instructions; to suggest additional response categories which can be pre-coded on the questionnaire in the future; and to provide a preliminary indication of the length of the interview and any refusal problems.
Questionnaire qualityCertain criteria were intended to be fulfilled while preparing the questionnaire: 1) inclusion of frequently encountered allergic symptoms, provoking factors and effect on quality of life; 2) reliability in discriminating between actual allergic from non-allergic symptoms; 3) simplicity i.e. short sentences, words which are simple, direct and familiar to all respondents. Questions with two to three possible answers for each question (yes-no- do not apply); 4) questions clear and as specific as possible with an overall questionnaire flow; 5) avoidance of any leading or loaded questions; and 6) questions which should be applicable to all respondents.
Survey target populationThe target population were the Saudian students, employees and staff members in Taif University; the idea of this choice was that they represent different age groups and tribes and reside in different districts in Taif city. Moreover, they were encouraged to pass copies to others, thus allowing the inclusion of subjects aged less than 17 and more than 56 years, and those with different educational and socio-economic status. Explanation of the purpose of the survey was the duty of the Unit's trainee when handling the questionnaire. Moreover, any difficulty while completing the questionnaire and time needed to fill it was reported by the trainee.
Exclusion criteriaAll questionnaires from non-Saudian citizens or those from other cities of the kingdom even if they were living in Taif city were discarded from the study.
Phase IThis questionnaire-based epidemiological survey was planned to be “Phase I” of two phases. Phase I was designed to assess the prevalence and severity of allergic diseases in defined population and evaluate the acceptance of the questionnaire by the studied subjects, especially since the questionnaire comprised 143 questions which could be considered long for a questionnaire. However, as there were no previous documented data of the most prevalent allergic diseases in the city, and as the studied population had no previous knowledge that most of their long lasting symptoms were allergic in nature; this necessitated a questionnaire covering almost all the usual and unusual symptoms of various allergic diseases. Phase II, which has yet to be developed, will be a national cross-sectional survey study. This phase may also reveal prevalence of certain allergic diseases in certain Saudian tribes.
StatisticsData were collected; the percentage of prevalence of various allergic diseases (total and according to gender) was calculated, tabulated and graphed.
Overall agreement between diagnoses reached by questionnaire and that reached by the doctor for the 50 sample cases, was compared using the likelihood-ratio test. This is a statistical test in which a ratio is computed between the maximum probabilities of a result under two different hypotheses, so that a decision between two hypotheses based on the value of this ratio can be made. The numerator corresponds to the maximum probability of an observed result under the null hypothesis. The denominator corresponds to the maximum probability of an observed result under the alternative hypothesis. Lower values (0.1) of the likelihood ratio mean that the observed result was less likely to occur under the null hypothesis. Higher values (10) mean that the observed result was more likely to occur under the null hypothesis.
ResultsParticipantsThe questionnaire was handed to 1050 subjects, from those 877 (83.52%) were completed, however, 23 questionnaire were discarded due to missing replies. Thus 854 (81.33%) were included in this study with age range from 3 years to 65 years. Total female participants were 543 (63.58%), and total male participants 311(36.42%). The average time to fill out the questionnaire was estimated to be between 15 to 20minutes.
Prevalence of urticaria and angio-oedemaSymptoms of various forms of urticaria±angio-oedema were reported in 547 subjects (64.05%) (490 with urticaria per se and 57 with both urticaria and angio-oedema) (Table 1). In addition, 13 cases reported angio-oedema without associated urticaria. Urticaria was encountered more frequently in the women 344/543 (63.35%) than in the men 146/311 (46.95%). Many studied subjects had more than one form of urticaria (Table 2). The distinction between acute and chronic urticaria was not used in this study for the sake of simplicity, meanwhile, the questions were precise to enable to identify the eliciting factor(s) of urticaria.
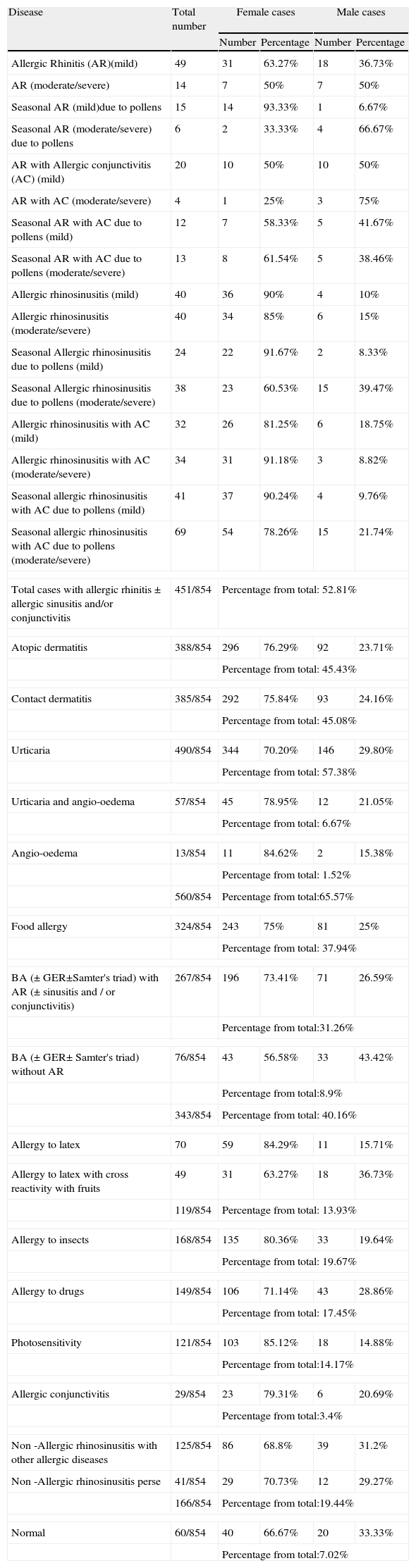
Prevalence of various allergic diseases in the studied population.
| Disease | Total number | Female cases | Male cases | ||
| Number | Percentage | Number | Percentage | ||
| Allergic Rhinitis (AR)(mild) | 49 | 31 | 63.27% | 18 | 36.73% |
| AR (moderate/severe) | 14 | 7 | 50% | 7 | 50% |
| Seasonal AR (mild)due to pollens | 15 | 14 | 93.33% | 1 | 6.67% |
| Seasonal AR (moderate/severe) due to pollens | 6 | 2 | 33.33% | 4 | 66.67% |
| AR with Allergic conjunctivitis (AC) (mild) | 20 | 10 | 50% | 10 | 50% |
| AR with AC (moderate/severe) | 4 | 1 | 25% | 3 | 75% |
| Seasonal AR with AC due to pollens (mild) | 12 | 7 | 58.33% | 5 | 41.67% |
| Seasonal AR with AC due to pollens (moderate/severe) | 13 | 8 | 61.54% | 5 | 38.46% |
| Allergic rhinosinusitis (mild) | 40 | 36 | 90% | 4 | 10% |
| Allergic rhinosinusitis (moderate/severe) | 40 | 34 | 85% | 6 | 15% |
| Seasonal Allergic rhinosinusitis due to pollens (mild) | 24 | 22 | 91.67% | 2 | 8.33% |
| Seasonal Allergic rhinosinusitis due to pollens (moderate/severe) | 38 | 23 | 60.53% | 15 | 39.47% |
| Allergic rhinosinusitis with AC (mild) | 32 | 26 | 81.25% | 6 | 18.75% |
| Allergic rhinosinusitis with AC (moderate/severe) | 34 | 31 | 91.18% | 3 | 8.82% |
| Seasonal allergic rhinosinusitis with AC due to pollens (mild) | 41 | 37 | 90.24% | 4 | 9.76% |
| Seasonal allergic rhinosinusitis with AC due to pollens (moderate/severe) | 69 | 54 | 78.26% | 15 | 21.74% |
| Total cases with allergic rhinitis±allergic sinusitis and/or conjunctivitis | 451/854 | Percentage from total: 52.81% | |||
| Atopic dermatitis | 388/854 | 296 | 76.29% | 92 | 23.71% |
| Percentage from total: 45.43% | |||||
| Contact dermatitis | 385/854 | 292 | 75.84% | 93 | 24.16% |
| Percentage from total: 45.08% | |||||
| Urticaria | 490/854 | 344 | 70.20% | 146 | 29.80% |
| Percentage from total: 57.38% | |||||
| Urticaria and angio-oedema | 57/854 | 45 | 78.95% | 12 | 21.05% |
| Percentage from total: 6.67% | |||||
| Angio-oedema | 13/854 | 11 | 84.62% | 2 | 15.38% |
| Percentage from total: 1.52% | |||||
| 560/854 | Percentage from total:65.57% | ||||
| Food allergy | 324/854 | 243 | 75% | 81 | 25% |
| Percentage from total: 37.94% | |||||
| BA (± GER±Samter's triad) with AR (± sinusitis and / or conjunctivitis) | 267/854 | 196 | 73.41% | 71 | 26.59% |
| Percentage from total:31.26% | |||||
| BA (± GER± Samter's triad) without AR | 76/854 | 43 | 56.58% | 33 | 43.42% |
| Percentage from total:8.9% | |||||
| 343/854 | Percentage from total: 40.16% | ||||
| Allergy to latex | 70 | 59 | 84.29% | 11 | 15.71% |
| Allergy to latex with cross reactivity with fruits | 49 | 31 | 63.27% | 18 | 36.73% |
| 119/854 | Percentage from total: 13.93% | ||||
| Allergy to insects | 168/854 | 135 | 80.36% | 33 | 19.64% |
| Percentage from total: 19.67% | |||||
| Allergy to drugs | 149/854 | 106 | 71.14% | 43 | 28.86% |
| Percentage from total: 17.45% | |||||
| Photosensitivity | 121/854 | 103 | 85.12% | 18 | 14.88% |
| Percentage from total:14.17% | |||||
| Allergic conjunctivitis | 29/854 | 23 | 79.31% | 6 | 20.69% |
| Percentage from total:3.4% | |||||
| Non -Allergic rhinosinusitis with other allergic diseases | 125/854 | 86 | 68.8% | 39 | 31.2% |
| Non -Allergic rhinosinusitis perse | 41/854 | 29 | 70.73% | 12 | 29.27% |
| 166/854 | Percentage from total:19.44% | ||||
| Normal | 60/854 | 40 | 66.67% | 20 | 33.33% |
| Percentage from total:7.02% | |||||
*OAS: oral allergy syndrome; **GER: Gastro-esophageal reflux.
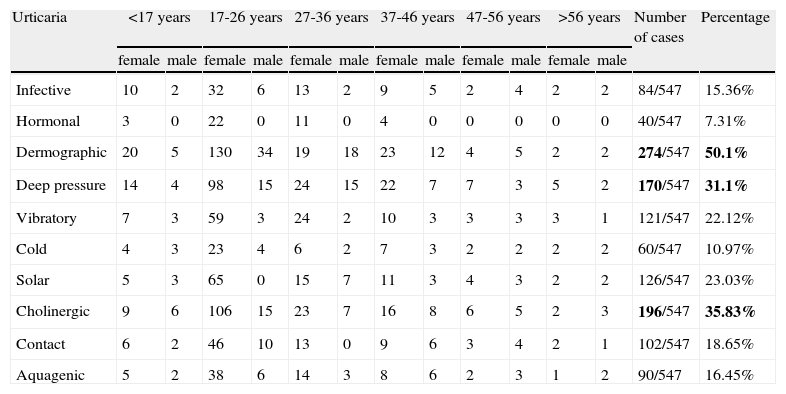
Prevalence of urticaria in different age and sex groups.
| Urticaria | <17 years | 17-26 years | 27-36 years | 37-46 years | 47-56 years | >56 years | Number of cases | Percentage | ||||||
| female | male | female | male | female | male | female | male | female | male | female | male | |||
| Infective | 10 | 2 | 32 | 6 | 13 | 2 | 9 | 5 | 2 | 4 | 2 | 2 | 84/547 | 15.36% |
| Hormonal | 3 | 0 | 22 | 0 | 11 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 40/547 | 7.31% |
| Dermographic | 20 | 5 | 130 | 34 | 19 | 18 | 23 | 12 | 4 | 5 | 2 | 2 | 274/547 | 50.1% |
| Deep pressure | 14 | 4 | 98 | 15 | 24 | 15 | 22 | 7 | 7 | 3 | 5 | 2 | 170/547 | 31.1% |
| Vibratory | 7 | 3 | 59 | 3 | 24 | 2 | 10 | 3 | 3 | 3 | 3 | 1 | 121/547 | 22.12% |
| Cold | 4 | 3 | 23 | 4 | 6 | 2 | 7 | 3 | 2 | 2 | 2 | 2 | 60/547 | 10.97% |
| Solar | 5 | 3 | 65 | 0 | 15 | 7 | 11 | 3 | 4 | 3 | 2 | 2 | 126/547 | 23.03% |
| Cholinergic | 9 | 6 | 106 | 15 | 23 | 7 | 16 | 8 | 6 | 5 | 2 | 3 | 196/547 | 35.83% |
| Contact | 6 | 2 | 46 | 10 | 13 | 0 | 9 | 6 | 3 | 4 | 2 | 1 | 102/547 | 18.65% |
| Aquagenic | 5 | 2 | 38 | 6 | 14 | 3 | 8 | 6 | 2 | 3 | 1 | 2 | 90/547 | 16.45% |
The results of the prevalence of allergic rhinitis with or without allergic conjunctivitis and/or sinusitis are shown in Table 1. A total of 451 subjects (52.81%) had complaints evidencing the disease, according to ARIA 2008.4 However, to simplify the terms “in a certain season” for seasonal AR, and “all year round” for perennial AR were used to simplify the questions to the subjects.
This study evidenced 233/451 (51.66%) with mild AR and 218/451 (48.34%) with moderate/severe AR. Those showing evidence of pollen allergy accounted for 218 subjects (45.89%). Meanwhile, 166 subjects (19.44%) show evidence of rhinitis and/or sinusitis of no allergic basis according to ARIA 2008,4 however, the exact cause of the encountered rhinosinusitis was not within the scope of this study.
The agreement between AR diagnosed by questionnaire and that by the Consultant in the 50 sample cases using likelihood ratio evidenced positive predictive value (PPV); negative predictive value (NPV); sensitivity; specificity; and likelihood ratio of 50% (95%CI 39.02-60.98); 50% (95%CI 23.02-76.98); 86% (95% CI 73.23-94.18); 14% (95%CI 5.82-26.77); and 1, respectively.
Prevalence of atopic dermatitis symptomsThe next most prevalent allergic disease in the studied population was atopic dermatitis (AD) where 388/854 subjects (45.43%) satisfied the widely accepted diagnostic criteria developed by Hanifin and Rajka.12 The agreement between AD diagnosed by questionnaire and that by Consultant in the 50 sample cases using likelihood ratio evidenced PPV; NPV; sensitivity; specificity; and likelihood ratio of 50% (95%CI 39.02-60.98); 50% (95%CI 23.02-76.98); 86% (95%CI 73.23-94.18); 14% (95%CI 5.82-26.77); and 1, respectively.
Prevalence of asthma symptomsA total of 343 subjects (40.16%) suffered from symptoms consistent with bronchial asthma. Samter's triad and gastro-oesophageal reflux were detected in 59 cases (17.20%) and 159 cases (46.36%), respectively. Allergic rhinitis was detected in 267/343 cases from the total studied subjects (77.84%) suffering from asthma. Thus, 56.21% of the total subjects with AR had evidence of asthma, and 77.84% of subjects with bronchial asthma showed symptoms evidencing coexistent AR.
The agreement between asthma diagnoses reached by questionnaire and that by Consultant in the 50 sample cases using likelihood ratio evidenced PPV; NPV; sensitivity; specificity; and likelihood ratio of 50% (95%CI 26.02-73.98); 50% (95%CI 38.75-61.25); 18% (95% CI 8.57-31.43); 82% (95%CI 68.57-91.43); and 1 respectively.
Prevalence of other allergic diseases- -
Complaints matching with contact dermatitis had been reported in 385 subjects (45.08%), mostly women (75.84%). The main offending materials were leather (196 cases), cosmetics (170 cases), and nickel jewellery (164 cases).
The agreement between contact dermatitis cases diagnosed by questionnaire and that by Consultant in the 50 sample cases using likelihood ratio evidenced PPV; NPV; sensitivity; specificity; and likelihood ratio of 50% (95%CI 36.83-63.17); 50% (95%CI 33.82-66.18); 60% (95% CI 45.22-73.62); 40% (95%CI 26.38-54.78), and 1, respectively.
- -
Symptoms featuring possible food allergy were encountered in 324/854 subjects (37.94%). Food allergy manifested by gastrointestinal manifestations in 139 cases (42.9%), oral allergy syndrome (OAS) in 123 cases (37.96%), angio-oedema in 68 cases (20.9%), and urticaria in 62 cases (19.14%).
Meanwhile, provocation or exacerbation of existing allergic rhinitis, asthma, induction of anaphylaxis or occurrence of eczema were recorded in 119 (36.73%), 73 (22.53%), 37(11.42%) and 42 (12.96%) cases respectively following one or more food intake. Symptoms compatible with infection with anisakiasis simplex were recorded in 66 cases (20.37%).
The agreement between food allergy diagnosed by questionnaire and that by Consultant in the 50 sample cases using likelihood ratio evidenced PPV; NPV; sensitivity; specificity; and likelihood ratio of 50% (95%CI 34.59-65.41); 50% (95%CI 36.34-63.66); 44% (95% CI 30.01-58.70); 56% (95%CI 41.30-69.99); and 1, respectively.
- -
Complaints suggesting allergy to latex were reported in 119 of the studied subjects (13.93%). Only 49 subjects evidenced cross-reactivity to food elements, especially banana, tomato, and kiwi. Seventy-four (62.18%) cases reported contact urticaria on exposure to latex products and 28 (23.53%) reported symptoms of rhino-conjunctivitis, wheezes and angio-oedema. Out of the 119 cases, 18 (15.13%) reported symptoms suggestive of oral allergy syndrome, and 47 (39.5%) gave history evidencing hand eczema. All these cases had complaints of other allergic diseases, especially allergic rhinitis which was encountered in 81 (68.07%) cases.
The agreement between allergy to latex diagnosed by questionnaire and that by Consultant in the 50 sample cases using likelihood ratio evidenced PPV; NPV; sensitivity; specificity; and likelihood ratio of 50% (95%CI 15.71-84.29); 50% (95%CI 39.42-60.58); 8% (95%CI 2.22-19.24); 92% (95%CI 80.76-97.78); and 1, respectively.
- -
Symptoms suggestive of immunological drug hypersensitivity reactions were reported in 149 (17.45%) studied subjects mainly to antibiotics and non-steroidal anti-inflammatory drugs. Thirty-four (22.82%) evidenced angio-oedema of eyelids following certain drug intake, especially antibiotics (question number 94), forty subjects (26.85%) evidenced urticaria after certain medications intake (questions number 95,96), two (1.34%) experienced pruritus (question number 96), 53 (35.57%) experienced symptoms matching with serum sickness (questions number 95,97,98), 10 (6.71%) evidenced bleeding from mucosa following drug intake suggesting occurrence of complicated thrombocytopenia, 55 (36.9%) evidenced permanent pigmentation, 31 (20.8%) experienced widespread reddish coloration of skin (suggestive of erythroderma), 51 (34.23%) experienced wheezing or difficulty of breathing especially following antibiotics, lastly, only five (3.4%) subjects reported shedding of part of their skin surface; however, this was never serious enough to require hospitalisation.
The agreement between allergy to drugs diagnosed by questionnaire and that by Consultant in the 50 sample cases using likelihood ratio evidenced PPV; NPV; sensitivity; specificity; and likelihood ratio of 50% (95%CI 11.81-88.19); 50% (95%CI 39.56-60.44); 6% (95%CI 1.25-16.56); 94% (95%CI 83.44-98.74), and 1, respectively.
- -
Allergy to insects (especially to bees, ants, ticks and mosquitoes) was reported in 168 (19.67%) of studied subjects, all suffered from other forms of allergic diseases. The type of reaction to insect bites varied markedly in those cases, 116 (69.05%) suffered from generalised urticaria, 37 (22.02%) from nausea, vomiting and abdominal pain, and 28 (16.67%) from dyspnoea. None of the 50 sample cases evidenced allergy to insects.
- -
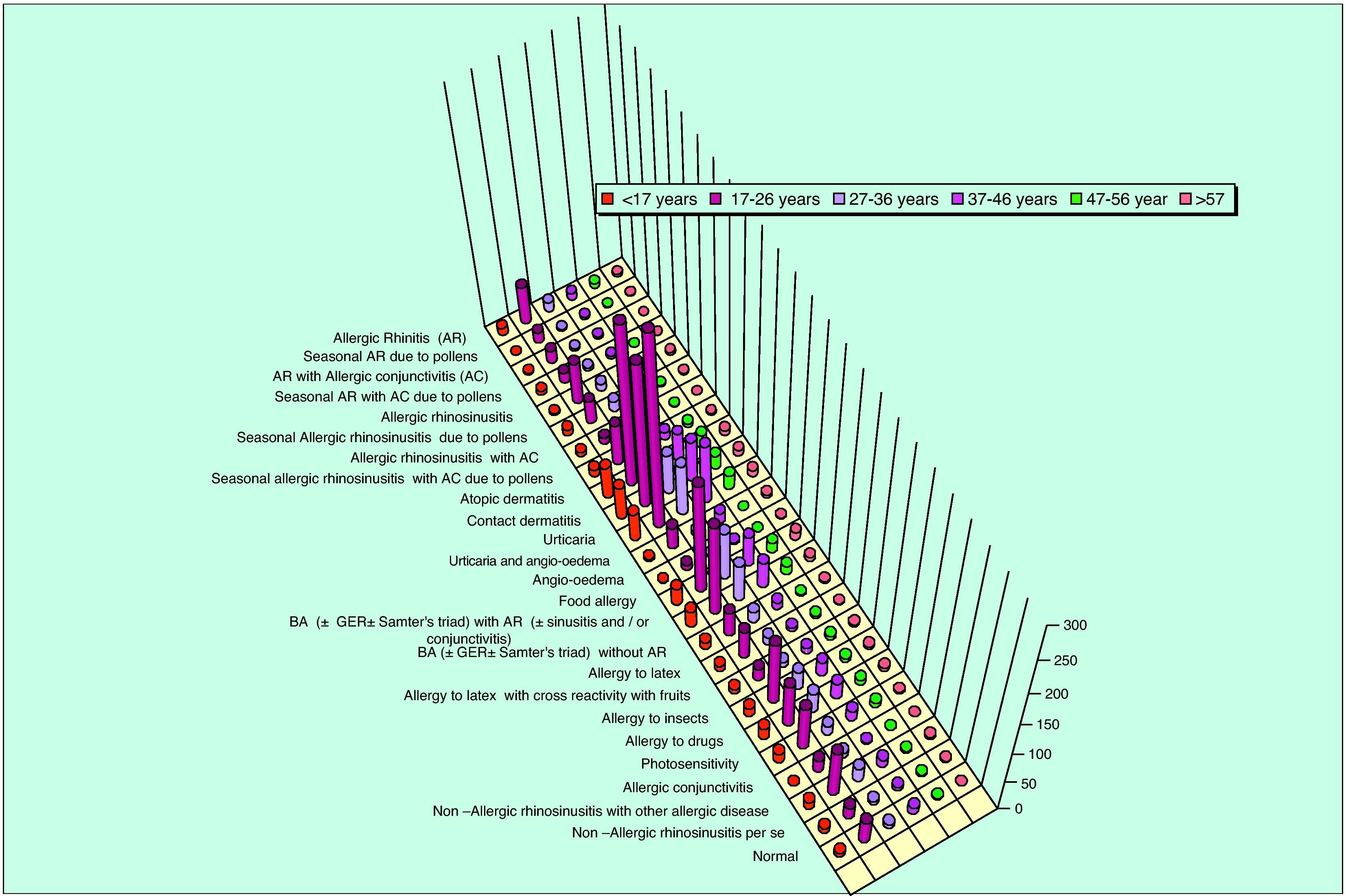
Photoreactions in the form of polymorphous light eruption were detected in 121 (14.17%) cases; they experienced itchy skin eruption and not urticaria following exposure to sun.Lastly, only 60 (7.02%) subjects had no complaints matching with any allergic disease(s). The prevalence rates of various allergic diseases in studied population according to age group are shown in Fig. 1.
Symptom-based questions have been recommended to avoid underestimation of the prevalence, to achieve comparable results in different populations, and to screen even patients with mild symptoms. To the best of the author's knowledge, this cross-sectional randomised study using a questionnaire aiding in determining the prevalence and severity of various allergic diseases, rather than just one or two, in Saudi population in general and specifically in Taif city is the first of its kind in this country.
The information obtained from the study is valuable for determining the burden of the disease in the city and later on maybe in the whole country. It can be used for the development of a strategic public health plan for optimal management of these diseases. However, unfortunately, our data cannot be compared with similar studies in the country, as there are no similar previous population-based studies.
Urticaria is described as one of the most common skin diseases, additionally; two or more different subtypes of urticaria can coexist in any given patient. Of all the diagnostic procedures, the most important is to obtain a thorough history including all possible eliciting factors and significant aspects of the nature of the urticaria.13 As in the literature, dermographic urticaria was the most frequent form of physical urticaria, encountered in 50.1% of our studied population. Meanwhile, for special types of urticaria, cholinergic urticaria (35.83%) had a higher prevalence than reported previously in other studies (11.2%).14
Angio-oedema is associated with chronic urticaria in about 40%,15 however, in this study, 6.67% only of the studied population evidenced angio-oedema associated with urticaria. This study demonstrated herein the high and low prevalence of certain types of urticaria in the studied population compared with other studies.
Allergic rhinitis (AR) is a global health problem; in many countries its prevalence is often higher than 50% of the population in some age groups.4 In this study, AR was the second most prevalent allergic disease, encountered in 451 of studied subjects (52.82%), with symptoms suggestive of pollinosis in 45.89%. These results are higher than in any other studies which detected prevalence of allergic rhinitis (seasonal and /or perennial) by questionnaire.16–19 However, in some studies the high prevalence rates were proved when using questionnaire alone.17,20 Comparison of co-existing morbidities’ prevalence with AR in this study with other studies, revealed a higher percentage than in the literature regarding bronchial asthma, which was detected in 56.21%.21 The present study showed the relevance of this health problem, and corroborates the recommendations of the World Health Organization (WHO) regarding an integrated diagnostic, therapeutic, and prophylactic approach to AR and asthma.4
Atopic dermatitis (AD) is one of the most common chronic inflammatory skin diseases and its incidence is increasing. It is thought to affect 10-15% of the population.22 Meanwhile, different prevalence rates were reported in other studies, from a rate as low as 1–2% in adults and 10–15% in children,23 to as high as 9.7%, 23% and 24.8% in Great Britain, Scandinavian countries and Puerto Rico.24–26
AD was the third most prevalent disease according to the questionnaire (45.43%), with a higher percentage rate than has ever been reported in the literature. In Taif, the all year round dry weather and the marriage of natives from similar tribes or from other native tribes may be a risk factor. On the contrary, while high altitude is mentioned to improve AD27 it was not the case in this study.
Contact dermatitis (CD) is an inflammatory skin condition induced by exposure to an environmental agent. It is one of the most common skin diseases. In this study, most cases reported CD to leather, nickel, and cosmetics. Leather articles are known to contain several substances that may cause allergic contact dermatitis.28 Nickel is the most common cause of allergic CD in women in almost all countries. The greater exposure of women to high-nickel content jewellery is a predisposing factor.29 However, in the literature there were no data available about the actual prevalence of CD due to leather, nickel, nor cosmetics. As far as the author's knows; this is the first study in Saudi Arabia reporting the prevalence of contact dermatitis to nickel, leather and cosmetics.
A basic problem in questionnaire studies dealing with asthma is the absence of any gold standard for the diagnosis of asthma. However, written questionnaires are probably the method of choice for comparing prevalence.
Previous survey studies conducted in Saudi Arabia showed a prevalence rate as low as 3.59%–6.9% in some studies, and as high as 19.5%–23% in other studies.30–32 However, the prevalence increased threefold in one study in a period of 10 years.32 In this study the prevalence of asthma was as high as 40.16%, with prevalence of asthma in 56.21% of patients with allergic rhinitis. The only explanation to this high prevalence rate is the high prevalence rate of allergic diseases among the studied population due to the criteria mentioned before, especially that almost all the studied population gave a positive reply to the presence of an allergic family member.
Food allergy is recognised as a common worldwide problem, although about one-third of the world's population perceives that it is allergic to one or more foods, the actual incidence of food allergy is estimated at 2–4% in adults and 6–8% in children. Moreover, Eriksson in 197833 stated that when a questionnaire is used for diagnosis, food allergens causing immediate reactions will mainly be discovered.
In this study, trying to limit the bias of overestimation of allergy, two questions were repeated in the questionnaire with every mentioned symptom: “Do these symptoms recur every time you eat the same type of food?” and “Do these symptoms recur even when eating small quantity of the same type of food?” Additionally, most questions dealt with immediate allergic food reaction.
According to various studies, about 20–40% of patients suffering from pollinosis and develop adverse food reaction after ingestion of some vegetable foods, the so-called oral allergy syndrome (OAS), a similar result was detected in this study (37.96%). Moreover, 36.73% reported sneezing, rhinorrhea and eye redness after certain food intake; those were already suffering from allergic rhinitis. The prevalence of food-induced allergic rhinitis reported to be less than 1%; although 25 to 80% of patients with documented IgE-mediated food allergy have nasal symptoms during oral food challenges, other food-induced allergic manifestations were also detected. Urticaria, angio-oedema, and eczema were high and reached up to 19.14%, 20.9% and 26.52%, respectively. The skin is a common target organ for allergic responses to food, with “acute” urticaria and angio-oedema as the most common cutaneous disorders. In addition, 22.53% of cases with reported food allergy had evidenced breathlessness and/or wheezes.
In the literature, only 10% of people who reported food allergy/intolerance had breathlessness as a symptom following food ingestion. Finally, as various gastrointestinal food-induced allergic disorders share the same symptoms, such as vomiting, abdominal distension and pain, and diarrhoea, in this study the questions dealing with gastrointestinal food-induced allergic disorders were not specific for a certain disease entity but aimed at determining presence of the disorder.34,35
Systemic allergic reactions to insect stings are estimated to occur in about 1% of children and 3% of adults.6 The diagnosis of insect sting allergy rests on the history, because positive test results can occur in persons who do not react to insect stings.36 In this study, the most common and easily observed systemic manifestations following insect sting allergy were included as three questions. Generalised urticaria was the most experienced manifestation by cases. The high prevalence (19.67%) of insect sting allergy in this study could not be explained, but it should be noted that all the cases manifested multiple forms of allergic diseases and had family history of allergy. In the literature, there is no reference to those more prone to manifest with allergic reactions after insect stings; they are those with multiple allergic diseases and positive family history of allergy as the case in this study, this needs further investigation.
Skin reactions secondary to drug intake may occur as a result of specific immune allergy directed at the drug or its metabolite or by non-immune mechanisms; the latter are more common. Immune-mediated drug hypersensitivity reactions (IDHR) are estimated to account for 6% to 10% of all adverse drug reactions. Identifiable risk factors for drug hypersensitivity reactions include adult age, female gender, concurrent asthma, and previous hypersensitivity to related drugs, the case of most of our studied population.
Unfortunately, there is a lack of comprehensive data; this inadequacy could be attributed to reasons such as diagnostic dilemmas and lack of awareness to report. The questionnaire included questions dealing with the immunological manifestations of drug hypersensitivity such as angio-oedema, urticaria, pruritus, bronchospasm, serum sickness, and haemolytic thrombocytopenia. However, urticaria is reported to occur by a non-immunological mechanism similar to the case with fixed drug eruption.37
As far as the author's knowledge, there are no reported data in the literature evidencing the true prevalence of immunological drug hypersensitivity symptoms in a studied group.
The prevalence of natural rubber latex (NRL) allergy in the general non-atopic population is believed to be less than 1%. However, a higher prevalence up to 6.4% has been reported with serological tests in American and Italian blood donors. Studies indicate that over 50% of persons who are sensitive to latex have a history of some type of atopic illness. A questionnaire on past symptoms of latex allergy can be an important tool to aid diagnosis of latex sensitisation. This screening method can also pave the way for patient understanding and management of latex allergy reactions on a daily basis, thus preventing serious complications.38
In this study, the incidence of reported immediate latex allergy symptoms was as high as 13.93%; this might be explained by the fact that the studied subjects showed co-occurrence of other allergic diseases. It is worth mentioning that non-immediate manifestations of latex allergy were not mentioned in the questionnaire, as their onset is late after exposure to latex, which makes their recognition by ordinary people difficult. Moreover, as our studied population were non-medical subjects, so the questions used were different from other questionnaires used in other studies that stressed on the role of latex as a cause of occupational allergic manifestations.
Photosensitivity is common and probably affects members of all racial and ethnic groups, however, there have been no studies of its prevalence in the general population. Polymorphous light eruption is the most common form of photosensitivity and probably accounts for more than 90% of all cases. This condition was found to have prevalence between 5–21% in various surveys.39 In this study, the prevalence rate reported was 14.17%, with female predominance as a percentage and sex predominance40 similar to that reported in the literature.
The major strength of this study is first that the developed questionnaire proved its efficacy as a tool capable of assessing simultaneously the prevalence of almost all allergic diseases. Secondly, the enrolment of cases from different age groups, different tribes and districts in Taif city; and, its high response rate (81.33%). Lastly, the reported prevalence rates of various symptomatic forms of drug allergy and contact dermatitis.
However, there are some limitations: Firstly, most of the studied population was between the ages of 17–26 years with known high prevalence of allergic diseases; secondly, the questionnaire used on self-reported skin morbidity was subjected to bias. Lastly, no comparison with other validated international questionnaire was made, which is highly recommended in other large-scale studies. Finally, as for a questionnaire, it was long; although focused and non-redundant. However, the questions could not be combined as each aided in either diagnosing allergic or differentiating from other non-allergic causes. Nevertheless, despite these limitations, the results suggest that questionnaire screening for allergic diseases is still a viable approach. A large-scale funded application of the questionnaire in future studies is likely to provide more accurate measures of its diagnostic performance.
In conclusion, in order to promote remarkable changes in medical practice and consequently improvements in-patient outcomes, evidence-based guidelines must be implemented, however, their application must be tailored according to the region and patients and not the opposite. This necessitates full understanding of the actual allergy problems by health care services decision makers in each country and even cities. The best way, with proven success, is the written questionnaire, which could be handed out and disseminated at local and even national levels.
This study proved the capability of a written questionnaire in simple, direct and familiar Arabic language to define the prevalence and severity of various allergic diseases in a sample from the city of Taif. In addition, due to its success; decisions may be taken to perform a larger scale study (Phase II) nationally or even regionally in other Gulf cities. However, it will be shorter as the most prevalent diseases were unveiled.
Nevertheless, as this questionnaire is the first in the Middle East in simple Arabic language that could be easily understood in more than 20 countries, then it could be a step towards the actual estimation of various allergic diseases in a region long deprived of allergy recognition and good management.
Conflict of interestThe authors have no conflict of interest to declare.
I would like to thank all those who helped in the establishment of “Allergy Unit”, the first in all Saudian Universities.