There is currently no standard tool for the measurement of asthma in epidemiological studies. The objectives of this study were to determine the prevalence of asthma, to describe the potential local risk factors, and to assess the agreement between written and video questionnaires in 13- to 14-year-old schoolchildren.
MethodsWe performed a cross-sectional study involving 5427 adolescents in 26 schools. Prevalence of asthma symptoms were evaluated using the International Study of Asthma and Allergies in Childhood (ISAAC) written and video questionnaire. The adolescents were asked additional questions for risk factors of asthma.
ResultsThe prevalence of lifetime wheeze, wheeze in the last 12 months and doctor-diagnosed asthma with written questionnaire were found as 13.5%, 6.3% and 11.2% respectively. Prevalence of lifetime wheeze, wheeze in the last 12 months, wheeze after exercise in the last 12 months, with video questionnaire were found as 9.6%, 5.5%, 11.9% and 1.9% respectively. The proportion of total agreement between the two questionnaires was high (0.77–0.81) with poor kappa value (0.25–0.50). In multivariate analysis, family history of atopy, stuffed toys and accompaniment of children to their parents after school hours in textile industry were found as risk factors for asthma. In addition kind of bird, such as canary was found as a risk factor.
ConclusionPrevalence of asthma is moderate in Turkey. Agreement between the two questionnaires was high. Accompaniment of children to their parents in textile industry is a newly-described risk factor for asthma.
Asthma has become the most common chronic disease and is one of the major causes of hospitalisation and school absence among children. The prevalence of asthma changes in both developed and developing countries.1,2
Many surveys have determined the prevalence of asthma by using questionnaires, spirometry, and assessment of airway hyperreactivity.3,4 The prevalence of asthma varies between countries and between regions in the country.5 Symptoms may not be specific to asthma or it may be difficult for the patient to understand them. The International Study of Asthma and Allergies in Childhood (ISAAC) has established a standardised methodology to compare prevalence and severity of asthma in children between centres.5 Differences between countries may be due to environmental and socioeconomic factors and/or may be related to awareness of the disease.6,7 A video questionnaire (VQ) was developed to assess asthma symptoms more accurately (www.wnmeds.ac.nz/academic/med/warg/ADV.html).8,9
To our knowledge this was the first study made with VQ in Turkey. Denizli is a growing industrial city in the south-western part of Turkey. Denizli has achieved a remarkable economic development in the last decades based notably on textile production and exports. Besides its tourist attractions, the city of Denizli is known for its marble and textile industries and for connected fields of activity such as the dye industry. The textile industry in Denizli grew rapidly in the 1980s and 1990s making itself a place in the domestic market and for exports.10 In addition, the division of Paediatric Allergy was established in 2006 in University Hospital in Denizli. Thereafter, paediatric allergists started working and organising educational programmes about asthma for physicians, pharmacist and parents. To know the prevalence and risk factors of asthma was important for the education and awareness of the population.
This study was planned to determine the prevalence of asthma symptoms and risk factors for asthma in 13- to 14-year-old schoolchildren in Denizli, Turkey by using the ISAAC written questionnaire (WQ) and VQ and to assess the agreement between WQ and VQ.
MethodsStudy areaDenizli is a growing industrial city in the south-western part of Turkey. Denizli plays an important role in the textile and marble industries. Denizli is located in the Aegean Region of Turkey, but the climate is not monotype. There are climatic differences within the Province and even in the urbanised area of Denizli. A terrestrial climate is generally dominant in the centre of the province due to the fact that the area is like a pathway from the seaside to inland areas while the inland areas are cooler and have a higher elevation than the seaside – the western part of the province. The land is open to winds coming from the Aegean Sea because the mountains are perpendicular to the sea. Winters are rainy or sometimes snowy, but generally mild. It has a population of 942,278 with a surface area of 11,868km2. The literacy rate is 96.8% in Denizli, and this is the second highest literacy rate from Turkey.10
Study populationThis study was carried out on 5427 schoolchildren aged between 13 and 14 years. This age group was chosen to give a reflection to the period when mortality from asthma is more common and to enable the use of self-completed questionnaire. The schoolchildren or their parents signed a consent form in order to participate to the study. All students were from Turkey and speak Turkish as a mother language. There was no foreign participant. The study was performed between April and June 2008. All children completed the VQ immediately after the WQ on the same day.
QuestionnairesThe standardised core symptom questionnaire for 13–14 year olds was comprised of eight questions on symptoms relating to asthma.3,11
The definition of asthma was accepted as self-reporting of diagnosed asthma with a physician's confirmation.12 In general, doctors used the terms “allergic bronchitis” or “spastic bronchitis” instead of asthma.13 We used the Turkish translation of the original ISAAC questionnaire but only for question 6 (Have you ever had asthma?) we have added “with doctor's confirmation (spastic bronchitis, allergic bronchitis)”. This is because Turkish doctors usually use the terms “allergic bronchitis or spastic bronchitis instead of asthma”.13 We added the term to the modified version of ISAAC of the text. We revised the sentence about ISAAC questionnaire as “There have been studies carried out in Turkey using the modified version of ISAAC questionnaire”,13–16 therefore it is well known.
In addition, the international version of VQ which was acquired from the ISAAC centre was used in this study (www.wnmeds.ac.nz/academic/med/warg/ADV.html).8,9
There were also questions about demographic and environmental conditions surrounding the children that could be potential risk factors for asthma. These are sex, atopic family history, member of the family with atopic disease, number of atopic people living at home, number of sibling living at home, stuffed toys, education level of child's mother or father, presence of domestic animals, kind of domestic animal, kind of bird, place of the animal in the house, whether mother or father is working in textile and/or marble industry or not, accompaniment of children to their parents after school hours in textile and/or marble industry, active smoking, smoking of child's father or mother, and having allergic disease other than asthma.
Statistical analysisStatistical analysis included percentages, odds ratios (OR), 95% confidence interval (95% CI), chi-squared test and backward logistic regression analysis. The data were entered into a computer. Prevalence of symptoms was calculated by dividing positive responses to the given question by the total number of completed questionnaires. Then, 95% CI of these prevalence rates was calculated. According to ISAAC policy, missing and inconsistent responses were included in the prevalence calculations, but excluded from subsequent bivariate analysis.17,18 Landis and Koch have suggested that kappa values of 0.4 indicate poor agreement, values of 0.4–0.6 moderate agreement and of 0.8 good agreements.19 But there have been problems about kappa value. Feinstein and Cicchetti reported that despite the high proportion of agreement (Po) kappa value was low and to assess the agreement, four measures which are kappa, Po and the proportion of positive and negative agreement (Ppos, Pneg) should be presented.20,21 In our study, to assess agreement between written and video questionnaires, kappa, Po, Ppos, Pneg values were used.
The relation between risk factors and asthma prevalence was performed by univariate analysis using chi-squared tests and univariate odds ratio (uOR) and its 95% CI. P<0.05 was considered significant. To assess the independent risk factors on asthma, multivariate logistic regression analysis was applied to the significant factors after the univariate analysis. The SPSS software package version 12 for Windows (SPSS, Chicago, IL, USA) was used for all statistical analyses.
Ethical considerationThis study was approved by the ethics committee of School of Medicine, Pamukkale University.
ResultsThe final number of children who participated in the study was 4078, with an overall response rate of 75% (46.7% girls and 53.3% boys).
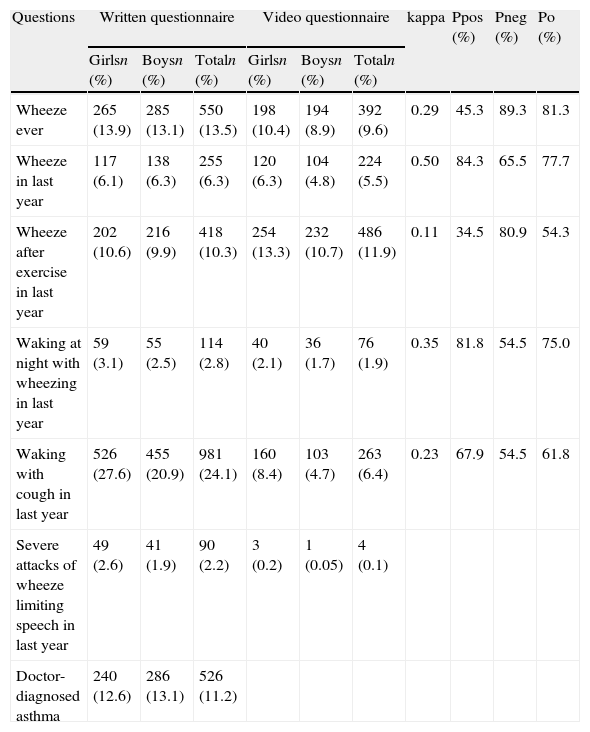
According to the WQ, the prevalence of lifetime wheeze, wheeze in the last 12 months, doctor-diagnosed asthma, wheeze after exercise in the last 12 months, nocturnal cough in the last 12 months, sleep disturbing wheeze in the last 12 months, and severe wheeze in the last 12 months were found to be 13.5%, 6.3%, 11.2%, 10.3%, 24.1%, 2.8% and 2.2%, respectively (Table 1).
Prevalences of wheeze, asthma and other symptoms and agreement of questionnaires (n=4078).
| Questions | Written questionnaire | Video questionnaire | kappa | Ppos (%) | Pneg (%) | Po (%) | ||||
| Girlsn (%) | Boysn (%) | Totaln (%) | Girlsn (%) | Boysn (%) | Totaln (%) | |||||
| Wheeze ever | 265 (13.9) | 285 (13.1) | 550 (13.5) | 198 (10.4) | 194 (8.9) | 392 (9.6) | 0.29 | 45.3 | 89.3 | 81.3 |
| Wheeze in last year | 117 (6.1) | 138 (6.3) | 255 (6.3) | 120 (6.3) | 104 (4.8) | 224 (5.5) | 0.50 | 84.3 | 65.5 | 77.7 |
| Wheeze after exercise in last year | 202 (10.6) | 216 (9.9) | 418 (10.3) | 254 (13.3) | 232 (10.7) | 486 (11.9) | 0.11 | 34.5 | 80.9 | 54.3 |
| Waking at night with wheezing in last year | 59 (3.1) | 55 (2.5) | 114 (2.8) | 40 (2.1) | 36 (1.7) | 76 (1.9) | 0.35 | 81.8 | 54.5 | 75.0 |
| Waking with cough in last year | 526 (27.6) | 455 (20.9) | 981 (24.1) | 160 (8.4) | 103 (4.7) | 263 (6.4) | 0.23 | 67.9 | 54.5 | 61.8 |
| Severe attacks of wheeze limiting speech in last year | 49 (2.6) | 41 (1.9) | 90 (2.2) | 3 (0.2) | 1 (0.05) | 4 (0.1) | ||||
| Doctor-diagnosed asthma | 240 (12.6) | 286 (13.1) | 526 (11.2) | |||||||
Po: proportion of total agreement; Pneg: proportion of negative agreement; Ppos: proportion of positive agreement.
According to the VQ, prevalence of lifetime wheeze, wheeze in the last 12 months, wheeze after exercise in the last 12 months, nocturnal wheeze in the last 12 months, nocturnal cough in the last 12 months, and severe wheeze in the last 12 months were 9.6%, 5.5%, 11.9%, 1.9%, 6.4%, and 0.1%, respectively (Table 1).
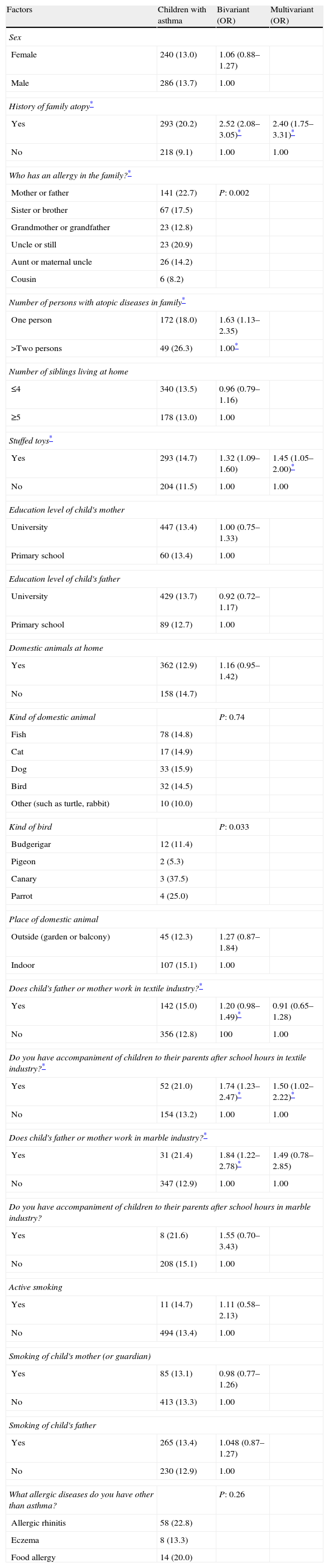
Risk factorsAccording to the WQ with univariate analysis, family history of atopy, an allergic person in the family, number of persons with atopic diseases in family, stuffed toys, the kind of bird, whether father or mother is working in the textile industry or not, accompaniment of children to their parents after school hours in textile industry, and whether father or mother is working in the marble industry or not, were found as risk factors for asthma. Multivariate analysis was performed for the significant risk factors (family history of atopy, stuffed toys, accompaniment of children to their parents after school hours in textile industry). Since other significant risk factors would decrease the number of children inserted into the analysis, they were not applied to multivariate analysis in order to prevent their possible effects on the evaluation of other risk factors (Table 2).
Risk factors affecting prevalence of asthma.
| Factors | Children with asthma | Bivariant (OR) | Multivariant (OR) |
| Sex | |||
| Female | 240 (13.0) | 1.06 (0.88–1.27) | |
| Male | 286 (13.7) | 1.00 | |
| History of family atopy* | |||
| Yes | 293 (20.2) | 2.52 (2.08–3.05)* | 2.40 (1.75–3.31)* |
| No | 218 (9.1) | 1.00 | 1.00 |
| Who has an allergy in the family?* | |||
| Mother or father | 141 (22.7) | P: 0.002 | |
| Sister or brother | 67 (17.5) | ||
| Grandmother or grandfather | 23 (12.8) | ||
| Uncle or still | 23 (20.9) | ||
| Aunt or maternal uncle | 26 (14.2) | ||
| Cousin | 6 (8.2) | ||
| Number of persons with atopic diseases in family* | |||
| One person | 172 (18.0) | 1.63 (1.13–2.35) | |
| >Two persons | 49 (26.3) | 1.00* | |
| Number of siblings living at home | |||
| ≤4 | 340 (13.5) | 0.96 (0.79–1.16) | |
| ≥5 | 178 (13.0) | 1.00 | |
| Stuffed toys* | |||
| Yes | 293 (14.7) | 1.32 (1.09–1.60) | 1.45 (1.05–2.00)* |
| No | 204 (11.5) | 1.00 | 1.00 |
| Education level of child's mother | |||
| University | 447 (13.4) | 1.00 (0.75–1.33) | |
| Primary school | 60 (13.4) | 1.00 | |
| Education level of child's father | |||
| University | 429 (13.7) | 0.92 (0.72–1.17) | |
| Primary school | 89 (12.7) | 1.00 | |
| Domestic animals at home | |||
| Yes | 362 (12.9) | 1.16 (0.95–1.42) | |
| No | 158 (14.7) | ||
| Kind of domestic animal | P: 0.74 | ||
| Fish | 78 (14.8) | ||
| Cat | 17 (14.9) | ||
| Dog | 33 (15.9) | ||
| Bird | 32 (14.5) | ||
| Other (such as turtle, rabbit) | 10 (10.0) | ||
| Kind of bird | P: 0.033 | ||
| Budgerigar | 12 (11.4) | ||
| Pigeon | 2 (5.3) | ||
| Canary | 3 (37.5) | ||
| Parrot | 4 (25.0) | ||
| Place of domestic animal | |||
| Outside (garden or balcony) | 45 (12.3) | 1.27 (0.87–1.84) | |
| Indoor | 107 (15.1) | 1.00 | |
| Does child's father or mother work in textile industry?* | |||
| Yes | 142 (15.0) | 1.20 (0.98–1.49)* | 0.91 (0.65–1.28) |
| No | 356 (12.8) | 100 | 1.00 |
| Do you have accompaniment of children to their parents after school hours in textile industry?* | |||
| Yes | 52 (21.0) | 1.74 (1.23–2.47)* | 1.50 (1.02–2.22)* |
| No | 154 (13.2) | 1.00 | 1.00 |
| Does child's father or mother work in marble industry?* | |||
| Yes | 31 (21.4) | 1.84 (1.22–2.78)* | 1.49 (0.78–2.85) |
| No | 347 (12.9) | 1.00 | 1.00 |
| Do you have accompaniment of children to their parents after school hours in marble industry? | |||
| Yes | 8 (21.6) | 1.55 (0.70–3.43) | |
| No | 208 (15.1) | 1.00 | |
| Active smoking | |||
| Yes | 11 (14.7) | 1.11 (0.58–2.13) | |
| No | 494 (13.4) | 1.00 | |
| Smoking of child's mother (or guardian) | |||
| Yes | 85 (13.1) | 0.98 (0.77–1.26) | |
| No | 413 (13.3) | 1.00 | |
| Smoking of child's father | |||
| Yes | 265 (13.4) | 1.048 (0.87–1.27) | |
| No | 230 (12.9) | 1.00 | |
| What allergic diseases do you have other than asthma? | P: 0.26 | ||
| Allergic rhinitis | 58 (22.8) | ||
| Eczema | 8 (13.3) | ||
| Food allergy | 14 (20.0) | ||
OR, odds ratio.
According to the WQ, the prevalence of lifetime wheeze and prevalence of wheeze in the last 12 months were found as 13.5% and 6.3%, respectively. These results were found as 9.6% and 5.5% respectively with the VQ. Kappa values varied from 0.29 to 0.50. The proportions of positive agreement varied from 0.45 to 0.84, of negative agreement varied from 0.65 to 0.89 and of total agreement varied from 0.77 to 0.81 (Table 1).
The ratios of people who firstly gave a negative answer, but gave a positive answer after watching the video for lifetime wheeze, wheeze in last 12 months, wheeze after exercise, night cough and serious wheeze were 5.3%, 12.8%, 3.2%, 5.4% and 9.8%, respectively.
The ratios of people who firstly gave a positive answer, but gave a negative answer after watching the video for lifetime wheeze, wheeze in last 12 months, wheeze after exercise, night cough and serious wheeze were detected as 9.6%, 12.1%, 5.3%, 25.6%, 17.8% and 17%, respectively.
The VQ showed lower prevalence rates for asthma symptoms resulting in poor agreement between responses.
DiscussionWe used the ISAAC WQ and VQ with an overall response rate of 75%. According to the ISAAC study, the response rate ranged from 67% to100%.5 At the current study period, there was a high school entrance exam. So, absenteeism during this time may be the reason for low participation of children to our study.
Prevalence resultsWritten questionnaireIn our study, the prevalence of lifetime doctor diagnosed asthma was found as 11.2%. There was great variability for the prevalence of asthma between different countries. It ranged from 1.3% to 3.6% in India (Chennai, 1.3%), Iran (Tehran, 2.6%), Ethiopia (2.3%), Georgia (3.3%), Lithuania (3.3%), Albania (3.6%), and from 26.5 to 37.6% in Singapore (26.5%), Channel Islands (Guernsey, 26.9%), United Kingdom (Wales, 27.1%), Isle of Man (28.6%), Peru (33.1%) and New Zealand (Wellington, 36.3%; Christchurch, 37.6%).2 There was significant correlation between diagnosis of asthma and wheeze in the last 12 months.5 In some countries (Ethiopia, South Africa, South Korea, Iran, Brazil, Mexico, Paraguay, Estonia Finland, Romania, Russia, Ukraine, Austria, and Germany) the prevalence of wheeze within the last 12 months was relatively higher than asthma; however, it was relatively lower in other countries (Morocco, Indonesia, Japan, Malaysia, Philippines, Singapore, Taiwan, Kuwait, Sultanate of Oman, Peru).2 In our study, the prevalence of asthma (doctor-diagnosed asthma) was also found to be higher than wheeze within the last 12 months. This result was neither too high nor too low according to the results of the ISAAC committee.2 ISAAC committee reported that in general, prevalence of wheeze after exercise in the last 12 months was higher than that of wheeze in the last 12 months. The prevalence of wheeze after exercise in the last 12 months ranged from 2.6% to 42.5%2 and it was 10.3% in our study. Similar to the ISAAC committee results, prevalence of wheeze after exercise in the last 12 months was found higher than wheeze in the last 12 months.
In Turkey, only two studies have been made with the ISAAC questionnaire in the age group of 13 and 14 years. Lifetime wheeze, wheeze in the last 12 months and doctor-diagnosed asthma were found as 14.9%, 5.6%, 7% and 10.2%, 5.0%, 2.1% in the study of Sapan,22 and of Akcay et al.,14 respectively. When we compared our study with the previous study of Akcay et al.14 made in the same city, Denizli, in 2002, it was seen that there was a slight increase in the prevalence of lifetime wheeze (from 10.2% to 13.5%) and approximately two times decrease (from 10.2% to 6.3%) in the prevalence of wheeze in the last 12 months. But there was a 5.3 times increase in the prevalence of doctor-diagnosed asthma (from 2.1% to 11.2%).
When we look at the results from neighbouring countries to Turkey; the prevalence of current wheeze was 8.4% and 5.7% in Thessaloniki and Athens regions of Greece23 respectively; 24.1% in Lebanese24 and 8.7% in Cyprus.25 Prevalence of lifetime asthma was 11.5% and 7.7% in Thessaloniki and Athens regions of Greece23 respectively; 8.3% in Lebanese and 11.3% in Cyprus.24,25 In the Syrian Arab Republic the prevalence of wheezing in the last 12 months in different centres ranged from 3.9% to 6.5% and the prevalence of severe speech-limiting wheeze was ranged from 2.0%-3.5% in 13–14-year-olds.26 These results were similar to our results (life time DDA, 11.2%; current wheeze in the last 12 months, 6.3%). But prevalence of current wheeze in Lebanese was nearly four times higher than our results. Additionally, the prevalence of severe wheeze in Syrian was also similar to our result (2.2%).
Video questionnaireSo far we could not find such a study made by video questionnaire in Turkey. We found that prevalence of lifetime wheeze, wheeze in the last 12 months, wheeze after exercise, nocturnal wheeze, nocturnal cough, and severe wheeze were 9.6% and 5.5%, 11.9%, 1.9%, 6.4%, and 0.1%, respectively. The lowest prevalence of current wheeze (wheeze in the last 12 months) (<3%) were found in Albania (1.6%), Estonia (2.2%), Malaysia (Kota Bharu, 2.8%), and India (Chandigarh, 2.5%); on the other hand, the highest prevalences were found in Peru (15.8%) and India (Jodhpur, 21.4%).2
In our study, according to VQ responses, prevalence of wheeze in the last 12 months was approximately twice higher than in countries with low prevalence, and approximately three times lower than in countries with high prevalence. In other countries, prevalence of wheeze after exercise was generally higher than that of wheeze in the last 12 months.2 In our study, it was 11.9% and higher than prevalence of wheeze in the last 12 months.
Prevalence of nocturnal wheeze was generally lower and of nocturnal cough was generally higher than that of wheeze in the last 12 months.2 Similarly, in our study, prevalence of nocturnal wheeze (1.9%) was lower and prevalence of nocturnal cough (6.4%) was higher than prevalence of wheeze in the last 12 months (5.5%).
Prevalence of severe wheeze in the last 12 months (0.1%) was lower than that of other countries. The lowest prevalence (0.9%) was found in Thailand (Chingmai), while low prevalence were found in Estonia (1.5%), Albania (1.6%), Latvia (1.6%), India (Chennei,1.6%, Chandigarh, 1.9%), China (1.6%), Pakistan (1.9%), Finland (1.9%), and Sweden (2%).2
Agreement between written and video questionnaireAccording to the ISAAC study group, the video and written questionnaires were completed approximately by 317,000 children in the 13–14 year age group in 38 countries.27
In general, prevalence of wheeze in the last 12 months was higher in the WQ than that in the VQ. There were large variations in the prevalence of asthma symptoms between the WQ and VQ throughout the world.27 There are also wide variations in agreement between regions. The kappa value for the wheeze in the last 12 months was between 0.4 and 0.66 (moderate agreement) in only 20 centres, in the other 79 centres, it was less than 0.4 (poor agreement). The overall proportion of agreement (po) was high, ranging from 0.77 to 0.98, with good negative agreement (0.85–0.99) but poor positive agreement (0.06–0.67). In our study overall agreement ranged from 0.71 to 0.85 and kappa value ranged from 0.25 to 0.50. These results are closely correlated with phase one of ISAAC study group. In our study, the best overall agreement was for the lifetime wheeze and the best positive agreement was for the wheeze in the last 12 months. The reason for a high Po but low kappa value was due to mismatching of positive and negative responses. If children answered the written question negatively, then, they tended to answer the video question also negatively. This resulted in good negative agreement. On the contrary, if children answered the written question positively, a certain extent tended to answer positively after the video. This resulted in poor positive agreement. This leads to low kappa vales.
The language also affects the agreement between questionnaires. Some children at first answered negatively to the written questions, but then gave positive answers to the video. These children probably did not understand the written questions but recognised the symptom when they watched the video.27 In our study, the questions for the wheeze after exercise, nocturnal wheeze and severe wheeze were not understood well enough by Turkish children. There may be translation problems in the administration of written questionnaires in different languages. To overcome these problems, the video developed by the Wellington Asthma Research Group, was designed.8 Magnus and Jaakkola28 reported that interpretation of WQ and VQ differs between countries, languages and cultures. Crane et al.27 studied wheezy children with different languages. They reported that 6% of Russian-speaking wheezing children and 28% of Spanish speaking children, having responded negatively to the written question then responded positively to the video. They thought that children did not understand the WQ but recognised the symptom when they saw and heard it with VQ. Some children did not understand the term wheezing or considered their own experience of wheezing was less severe than the video. But 10% of all Russian wheezing children and 38% of English-speaking wheezing children gave a positive answer to both WQ and VQ. These children probably thought the video represented their understanding about wheezing. In addition, 84% of Russian-speaking wheezing children and 48% of English-speaking wheezing children did not agree when they saw the video. In our study, all children were from Turkey and spoke Turkish language. Probably some children in our study did not understand the term of wheezing in the WQ and answered negatively. But after the video description they recognise the wheezing symptom and answered positively. Some other children answered negatively after the video. When they saw the video description about wheezing they thought that their knowledge was inadequate and own experience about wheezing was not serious as video description. The agreement between questions may be improved by revising these questions.
Risk factorsAtopic family historyThe presence of atopic family history was reported as the most significant risk factor for the prevalence of asthma and all kinds of allergic disease.29 We also found that atopic family history increased the risk of asthma. Allergy in the first-degree relatives, especially in fathers or mothers, was found important in predicting asthma.29 In our study, according to univariate analysis, we found that when the number of atopic persons in the family increased, the risk of asthma also increased. And also, the presence of allergic disease in father, and mother increased the risk of asthma.
Stuffed toysIt is known that house dust mite allergen is a very important environmental risk factor for allergic sensitisation. They quickly accumulate on the stuffed toys and children often carry these toys with them.30,31 In our study too, stuffed toys increased the risk of asthma.
Presence of domestic animal and kind of domestic animalBener et al. reported that more allergic diseases occurred if there is a domestic animal in the house.32 Studies had reported different results.33,34 In our study, we did not find any relationship between kind of domestic animal and risk of asthma. But kind of bird was found important in such a way that in the presence of canary in the house, risk of asthma increased. This was an interesting finding. So we think more studies are needed in order to understand the relationship between kind of bird and risk of asthma.
Working in textile and marble industryThe textile industry was reported in many studies as one of the reasons for occupational asthma.35 Employees who work in the textile industry are at high risk of becoming sensitised to latex allergens especially when exposed to excessive dust produced by loom tuning machines. This sensitisation can cause asthma and other work-related allergic diseases.35 A considerable part of the people in Denizli work in textile and also in marble industry.10 For this reason, we evaluated whether there is a relationship between risk of asthma and textile and/or marble industry. We found that working mother or father in the textile industry was not associated with risk of asthma, but, accompaniment of children to their parents in textile industry increased risk of asthma. In addition, working mother or father in the marble industry and also accompaniment of children to their parents in marble industry did not increase risk of asthma. In textile workers cotton dust and textile dyeing have been reported to be associated with non-specific respiratory symptoms.36,37 Lai et al. suggested that obstructive lung disease such as asthma was related with textile dust.38 Apart from cotton dust, airborne endotoxin exposure is known to cause various pulmonary responses, such as alveolar-macrophage activation, neutrophil chemotaxis, complement activation, and histamine release from mast cells.39,40 We thought that exposure to cotton dust and airborne endotoxin may increase asthma symptoms in children also.
ConclusionsThe prevalence of asthma was moderate according to the results of ISAAC committee. Comparing with other studies conducted in Turkey, there was a considerable increase in the prevalence of doctor-diagnosed asthma and a decrease in the prevalence of wheeze in the last 12 months. Prevalence of severe wheeze in the last 12 months according to VQ was lower than that of WQ and also lower than that of other countries.
History of family atopy, stuffed toys and canary were associated with asthma. Accompaniment of children to their parents in textile industry is found as a new risk factor for asthma.
ContributorsTB has made contributions to conception and design of the study, acquisition of data.
AA has made contributions to conception and design of the study and interpretation of data, helped to statistical analysis and revising it critically for important intellectual content.
FD has made contributions to analysis and interpretation of data and helped to draft the manuscript.
CB has made contributions to acquisition and analysis of data.
AE has made contributions to analysis of data and performed the statistical analysis.
NG has revised the study and has given final approval of the version to be published.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
Conflict of interestThe authors have no conflict of interest to declare.