Food allergy (FA) is a frequent and common health problem; however, there are few population-based studies. Prevalence studies based on self-reported symptoms associated to FA are generally imprecise, ranging from 1.4 % to 33 %1–5. The prevalence of FA in the population depends on factors such as eating habits, cultural influences as well as the genetic background and methodologies applied6–10. However, few studies have been conducted at the population level. Most researchers suggest that the public's belief in FA is much higher than prevalence data support. However, FA self-perception questionnairebased studies conducted on a diverse population serve as groundwork for further objective studies11–16.
In the last few years several studies have suggested that the prevalence of FA is increasing17–19. A recent meta-analysis enclosing more than fifty studies, showed great heterogeneity in reported FA prevalence among different populations, and concluded that this could be a result of both differences in study design or methodology and populations20. The same study recommends that measurements be made using standardised methods, if possible food challenge. Europreval, a European Union funded integrated project, is the first initiative towards delivering information and tools necessary to undertake such a problem. In order to obtain reliable FA prevalence estimates, standard protocols and questionnaires are used21,22. To date there are few studies in developing countries showing the real dimension of FA as a public health issue23,24. The present study was carried out on 3099 subjects using a questionnaire. Our objectives were: a) to establish the prevalence of self-perception of FA; b) which were the most important foods implicated; c) the frequency of the most referred symptoms; d) the prevalence in each age range; and e) the most frequent food implicated according with age range.
METHODSPopulationThis is a cross-sectional study. A total of 3099 individuals in a randomised selection, aged 1-83years, and living in neighbourhoods in Cartagena were questioned about personal and family history of allergies and food allergy. Ethnically, Cartagena population is defined as a mixture between Caucasoids (Spaniards) and Negroids (Africans) that are named mulattos25. The subjects answered a questionnaire applied door-to-door by trained medical students. The sample was calculated according to Cartagena population size, and a proportional scale was used in each neighbourhood related to the number of houses. A pilot test with 50 individuals was carried out in order to validate the questionnaire.
QuestionnaireThe subjects were asked a questionnaire with ten questions in the following order: 1) personal data and occupation; 2) sex and age; 2) personal history of atopic diseases, rhinitis, asthma and eczema; 3) evaluation by allergist; 4) if yes, the result of the test; (5) the use of latex gloves; (6) if yes, tolerance to gloves. The following questions were designed to detect an allergic reaction after food or drink intake. In the case of positive reply, questions 9 and 10 were designed to establish the characteristics of reactions, and which, and how many foods, are implicated by the subjects.
Self-reported symptoms classificationWe classified the reported symptoms according to affected organs after food intake: 1) skin reactions if individuals reported symptoms, such as rash, itching, and redness; 2) gastrointestinal symptoms if the adverse reactions were vomits or nauseas, diarrhoea, and stomach pain; 3) respiratory symptoms, if these were throat tightness, wheezing, coughing, shortness of breath, and nasal congestion; 4) and other symptoms such as headache, itch and swelling of lips or mouth, swelling of face, and anaphylactic shock.
Statistical analysisThe data obtained were stored in SPSS software version 13. Statistical analysis was performed using descriptive statistics and we carried out a Chi square test to compare groups according to personal history for atopy and FA. A t-student test was done to establish OR with a confidence intervals of 95 %. If p < 0.05 it was considered significant.
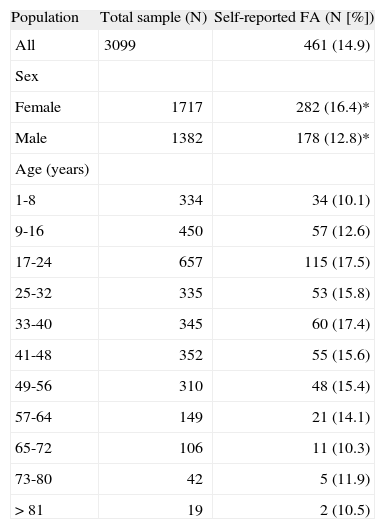
RESULTSA total of 3099 individuals participated in the survey. Report of food allergy (FA) was 14.9 % (n = 461). The prevalence of self-reported FA was higher in females (16.4 %) than in males (12.8 %) (p < 0.05). According to the age range, self-reported prevalence in patients from 1–8years, was 10.1 %; from 9–16years, 12.6 %; from 17–24years, 17.5 %; from 25–32years, 15.8 %; from 33–40years, 17.4 %; from 41–48years, 15.6 %; from 49–56years, 15.4 %; from 57–64years, 14.1 %; from 65–72years, 10.3 %; from 73–80years, 11.9 %; and more than 81years, 10.5 % (Table I).
The prevalence of self-reported food allergy (FA) in Cartagena population
| Population | Total sample (N) | Self-reported FA (N [%]) |
| All | 3099 | 461 (14.9) |
| Sex | ||
| Female | 1717 | 282 (16.4)* |
| Male | 1382 | 178 (12.8)* |
| Age (years) | ||
| 1-8 | 334 | 34 (10.1) |
| 9-16 | 450 | 57 (12.6) |
| 17-24 | 657 | 115 (17.5) |
| 25-32 | 335 | 53 (15.8) |
| 33-40 | 345 | 60 (17.4) |
| 41-48 | 352 | 55 (15.6) |
| 49-56 | 310 | 48 (15.4) |
| 57-64 | 149 | 21 (14.1) |
| 65-72 | 106 | 11 (10.3) |
| 73-80 | 42 | 5 (11.9) |
| > 81 | 19 | 2 (10.5) |
OR 1.33, CI 95 % (1.08-1.64), p < 0.05
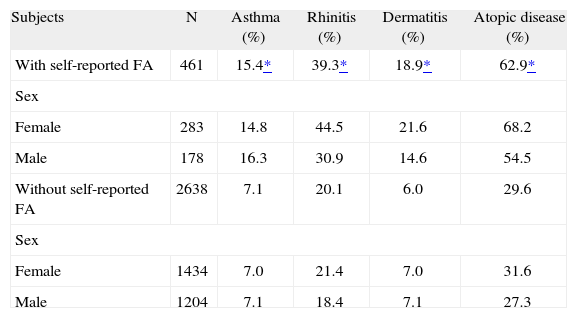
Atopic diseases were more frequent in subjects with self-reported FA than in the non self-reported FA (62.9 % vs. 29.6 %, OR 3.97, CI 95 %, 3.21-4.91, p < 0.0001). Asthma was present in 15.4 %, rhinitis in 39.3 %, and dermatitis in 13.2 % of patients with self-reported FA (Table II).
Atopic diseases in subjects with self-reported food allergy (FA) vs. without self-reported food allergy
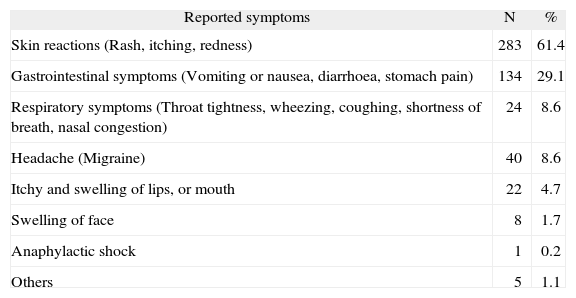
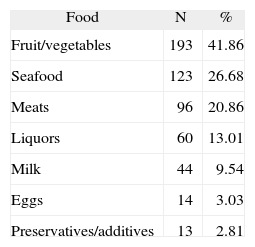
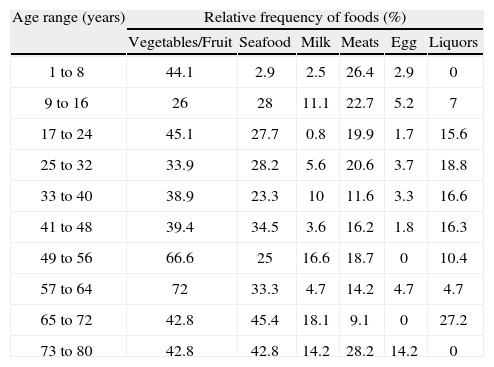
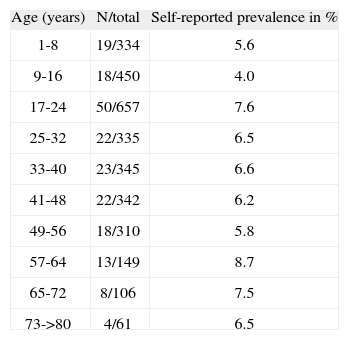
The most frequent symptoms reported were skin reactions (61.4 %), gastrointestinal (29.1 %), and respiratory symptoms (8.6 %) (Table III). Fruit and vegetables were the most implicated foods (41.86 %) followed by seafood with 26.8 % and meats with 20.86 % (Table IV). The relative frequency of responsible foods by age showed that fruit and vegetables were the most reported food allergen in almost all age ranges, except in the age range of 9-16years (Table V). The prevalence of self-reported reactions to fruits and vegetables according to age shows that they are important contributors to the overall prevalence in all age ranges (Table VI).
Most frequent symptoms in subjects with self-reported food allergy (FA) (n = 461)
| Reported symptoms | N | % |
| Skin reactions (Rash, itching, redness) | 283 | 61.4 |
| Gastrointestinal symptoms (Vomiting or nausea, diarrhoea, stomach pain) | 134 | 29.1 |
| Respiratory symptoms (Throat tightness, wheezing, coughing, shortness of breath, nasal congestion) | 24 | 8.6 |
| Headache (Migraine) | 40 | 8.6 |
| Itchy and swelling of lips, or mouth | 22 | 4.7 |
| Swelling of face | 8 | 1.7 |
| Anaphylactic shock | 1 | 0.2 |
| Others | 5 | 1.1 |
Relative frequency of seven food allergens according to age range
| Age range (years) | Relative frequency of foods (%) | |||||
| Vegetables/Fruit | Seafood | Milk | Meats | Egg | Liquors | |
| 1 to 8 | 44.1 | 2.9 | 2.5 | 26.4 | 2.9 | 0 |
| 9 to 16 | 26 | 28 | 11.1 | 22.7 | 5.2 | 7 |
| 17 to 24 | 45.1 | 27.7 | 0.8 | 19.9 | 1.7 | 15.6 |
| 25 to 32 | 33.9 | 28.2 | 5.6 | 20.6 | 3.7 | 18.8 |
| 33 to 40 | 38.9 | 23.3 | 10 | 11.6 | 3.3 | 16.6 |
| 41 to 48 | 39.4 | 34.5 | 3.6 | 16.2 | 1.8 | 16.3 |
| 49 to 56 | 66.6 | 25 | 16.6 | 18.7 | 0 | 10.4 |
| 57 to 64 | 72 | 33.3 | 4.7 | 14.2 | 4.7 | 4.7 |
| 65 to 72 | 42.8 | 45.4 | 18.1 | 9.1 | 0 | 27.2 |
| 73 to 80 | 42.8 | 42.8 | 14.2 | 28.2 | 14.2 | 0 |
The prevalence of self-reported plant food allergy in Cartagena population (3099)
| Age (years) | N/total | Self-reported prevalence in % |
| 1-8 | 19/334 | 5.6 |
| 9-16 | 18/450 | 4.0 |
| 17-24 | 50/657 | 7.6 |
| 25-32 | 22/335 | 6.5 |
| 33-40 | 23/345 | 6.6 |
| 41-48 | 22/342 | 6.2 |
| 49-56 | 18/310 | 5.8 |
| 57-64 | 13/149 | 8.7 |
| 65-72 | 8/106 | 7.5 |
| 73->80 | 4/61 | 6.5 |
The majority of studies related to FA have been carried out in European countries; to our knowledge, this is the first publication of a population-based study on FA in a Latin American country. In Colombia we do not have any epidemiological data related to this issue. This study is the first step in the knowledge about food allergy in order to identify if this condition is a public health problem in developing countries. The self-reported prevalence of FA was 14.9 %, which was higher in females than in males (16.4 % vs. 12.8 %). These results agree with other reports that used similar methodologies3,23. We believe that our prevalence is overestimated due to difficulties in conducting population-based studies with an objective assessment of FA. However, in a recent meta-analysis, where the authors reviewed fifty-one studies, they observed a high heterogeneity in the prevalence reports, even in studies of different countries following the same methodology26. Previous studies have shown less than 50 % of self-reported reactions being confirmed when controlled challenges are used5,11. The highest prevalence (17.5 %) was found between individuals with ages ranging from 17 to 24years, an interesting finding considering that the majority of studies report the highest prevalence among children4,27. The overall prevalence was higher among adults (> 16years) than children, possibly due to seldom reported child FA related symptoms by the parents as opposed to frequent adult reporting of their own symptoms. Questionnaire-based prevalence studies could overestimate data, but these are important tools for information about problems. Confirmation of these results will come only from further studies that include objective diagnostic tests.
FA prevalence was found to be more frequent among atopic individuals than in non-atopics (62.9 % vs. 29.6 %, p < 0.0001), as previously described by other studies. This result suggests that the atopic condition could be a risk factor to develop FA. Skin reactions were the most frequent symptoms related by the subjects (61.4 %), as reported in other populations1,2,28. A low frequency of anaphylactic shock related to FA was found in our study, in accordance with previous reports, probably due to the scarce reactions to nuts in our population1,20.
The most frequently implicated foods were fruit/vegetables with 41.86 % followed by seafood and meats with 26.8 % and 20.8 % respectively. In contradiction with other studies we found that fruit/vegetables were the most frequently related foods among the child population4,20, this profile could be due to the eating habits of our population. However, this study was questionnaire-based and reactions could be intoxications and other gastrointestinal conditions, hence these results should be confirmed by objective tests. It is very important to point out that this is the first population based study conducted in Latin America, and one of the first in a developing country. For this reason we conclude that this is the first step towards recognising FA as a public health issue in our population.
ACKNOWLEDGMENTSThis work was supported by the University of Cartagena, Colombia. Special thanks to Dr. Luis Caraballo for his critical reading of the manuscript, and the University of Cartagena's medical school students for their assistance in the interviews.