Studies have reported that children with atopic dermatitis (AD) have a high risk of adverse reactions at first egg ingestion.
MethodsWe enrolled 79 children with AD retrospectively and 45 children without AD (control group) prospectively, who had never eaten egg. All children underwent skin prick tests (SPT) with commercial extracts and prick by prick with natural food (raw and boiled egg). Oral food challenge (OFC) was performed in SPT positive patients.
ResultsSixty-six percent (52/79) of AD group and 11% (5/45) of Control group had at least one positive SPT (p<0.001), Relative Risk (RR)=5.9 and Odds Ratio=15.4. Of the 46/52 sensitised children in the AD group, 36 children ate egg for the first time in hospital during an OFC and 10 children ate egg at home because of their parents’ choice, with 19/46 (41%) resulting in allergic reactions to raw and/or boiled egg. Four/five sensitised children in the control group underwent OFC and three of them (75%) showed an allergic reaction to raw, but not boiled egg. Thirty percent (14/46) of AD group had a systemic reaction vs. 25% (1/4) of Control group.
ConclusionA child with AD has a RR of sensitisation to egg six times higher than a child without AD, before the first known ingestion. We propose to test sensitisation to egg in every child with AD who has never eaten egg, and to perform OFC in those with positive SPT in hospital setting.
Studies have reported that children with atopic dermatitis (AD) have a higher risk of adverse reactions at the first egg ingestion.1–4 Caffarelli et al.1 studied 21 infants (19 with AD) affected by IgE-mediated food allergy (FA) and 12 infants (control group) with non IgE-mediated FA. Sixty-two percent of patients in the active group and 8% in the control group had immediate reactions to oral food challenge (OFC) with boiled egg (p<0.01), one patient had anaphylactic shock. Monti et al.2 enrolled 107 children with AD (66 boys, 41 girls), aged 1–19 months; skin prick test (SPT) resulted positive in 63% of them. The egg OFC was conducted with raw egg at age 12–24 months, and resulted positive in 72/107 children (67.3%). Adverse reactions were observed in 48% of children with mild AD, 77% with moderate AD and 80% with severe AD. Seven percent of patients underwent anaphylactic reactions (5/72), 3/72 children with severe AD, 2/72 with mild/moderate AD. De Boisseau et al.3 studied 30 children with AD and IgE positive for egg, 24/30 children ate egg for the first time at a mean age of 30±9 months, and 18 presented adverse reaction. Dieguez et al.4 studied 104 cow's milk-allergic children (60% with AD); IgE for egg and OFC were performed at the age of 14 months, 65/104 (62.5%) resulted sensitised and 38/65 (76% with AD) allergic to egg; egg allergy was diagnosed in 22% (10/44) of children with IgE-mediate cow's milk allergy and without AD. Recent studies which tested the cooked egg tolerance in children allergic or sensitised to egg5,6 showed that adverse reaction at the ingestion of baked cake with egg was possible in patients with AD who had never eaten it. In children who presented specific IgE and had never eaten the suspected trigger food, some position papers7–9 suggested to perform OFC in the hospital setting. The authors gave this suggestion even for children with AD who had never eaten egg.8 This indication is quite expensive because of the economic and human resources employed and, to confirm the appropriateness of this indication, it is necessary to consider a control population (without AD or food allergy). There are no case-control studies available at the moment in this field.
We aimed to quantify the risk of sensitisation and allergy to egg in children with AD (first aim) by enrolling a group of healthy children without AD and without known food allergy – control group –, we tested their sensitisation and allergy to egg, and we compared these data to those obtained in a group of paediatric patients with AD. Moreover, since we know that the reactivity to raw egg is higher than that to heated egg,10 we tested both reactivities in our population (second aim).
Material and methodsInclusion criteriaThe study was performed in the Paediatric Department and Paediatric Allergy Day-Case Unit at Agostino Gemelli Hospital of Rome. Children with AD, with no limit of age, were retrospectively enrolled from June 2010 to June 2011 (AD group). AD was defined mild, moderate or severe according to the holistic assessment.11 Children of AD group were referred to our Paediatric Department by a family paediatrician, or taken to the Unit by their parents due to suspected food allergy. We prospectively enrolled from June 2011 to September 2011 healthy children referred to the General Paediatric Department of Agostino Gemelli Hospital of Rome for health supervisions (control group).
Each time a paediatrician established that children of both groups had never eaten egg before, even as an ingredient of a manufactured meal (such as biscuits, cakes, ice creams, sauces, pasta, meatballs). We excluded from the study children suffering from chronic illnesses, treated with immunosuppressor in the last four months or antihistaminic drugs in the last four weeks, or those who refused to consent.
The study was approved by Agostino Gemelli Hospital’ Ethics Committee.
Skin prick testSPT were performed with: 1) raw egg (mixed albumen and yolk), 2) boiled (for 10min) albumen and yolk separately, and 3) commercial extracts of albumen and yolk (Lofarma, Milan, Italy). Histamine (Lofarma, Milan, Italy 10mg/ml) was used as positive control and saline as negative control. Reactions occurring within 15min were analysed, and SPT were positive if mean diameter of the wheal was at least 3mm bigger than negative control.
Oral food challengeAn open OFC with raw egg was performed in those children with positive SPT to raw egg, using a whole egg with sugar. The meal was given in six increasing doses (one drop, 3 drops, 1ml, 3ml, 10ml, 30ml) every 20mins. An open OFC with boiled egg was performed in those children with positive SPT to boiled egg, using a whole boiled egg (chopped and mixed with salt), starting with one gram and doubling the dose every 20min until reaching one whole egg.
In case of subjective symptoms (oral itching, nausea, abdominal pain) or mild objective ones (a single episode of vomit, few urticaria wheals, few sneezes, mild ocular hyperaemia) OFC was not stopped and the dose causing symptoms administrated again and then slightly increased. OFC was considered positive and stopped in case of objective symptoms and/or serious, persistent, reproducible ones.12 OFC was considered negative in the absence of adverse reactions within two hours after the last dose. Reactions were defined systemic if they were anaphylactic, according to Sampson et al.,13 or generalised, corresponding to old definition of mild or moderate anaphylactic reactions.14
Statistical analysisStatistical analysis was performed using the Statistics program for biomedical disciplines – Stanton Glanz version 5.0. Chi-squared test was used to compare sensitised patients with patients allergic to egg proteins.
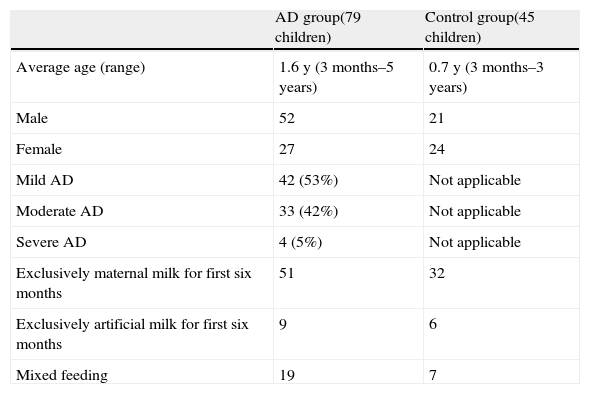
ResultsSeventy-nine children were enrolled in the AD group and 45 in the Control Group. Population characteristics are described in Table 1. Regarding the AD group, the reason for office visits has never been the difficulty of the symptomatic treatment of eczema, but the evaluation of a possible causal relationship with an allergy; so our children with AD are not different, for their severity, from those of the general population of children with AD. Although some children had an advanced age, a careful medical history could be ruled out that they had ever eaten the egg, which in Italy is considered as very allergenic, especially in children with AD. No child had known food allergies (IgE- and non IgE-mediated) at the time of recruitment. No subjects had to be excluded because they had recently received or were receiving antihistamines or immunosuppressor, and no subjects were not included because the parents refused to give consent. Informed consent was collected from parents of every child.
Main features of patients in AD group and control group. The differences between the two groups are not statistically significant.
| AD group(79 children) | Control group(45 children) | |
| Average age (range) | 1.6 y (3 months–5 years) | 0.7 y (3 months–3 years) |
| Male | 52 | 21 |
| Female | 27 | 24 |
| Mild AD | 42 (53%) | Not applicable |
| Moderate AD | 33 (42%) | Not applicable |
| Severe AD | 4 (5%) | Not applicable |
| Exclusively maternal milk for first six months | 51 | 32 |
| Exclusively artificial milk for first six months | 9 | 6 |
| Mixed feeding | 19 | 7 |
Due to its retrospective nature, not all children of the AD group performed the whole SPT panel. Fifty-two/79 children (65.8%) of AD group, resulted positive to at least one SPT, all children sensitised had SPT positive for raw egg. In particular, 39/52 performed a SPT for either raw or heated egg, and 17/39 (44%) resulted positive to raw egg only. 63% of sensitised children vs. 59% of non sensitised children had consumed maternal milk (p=not significant, ns). No child had invalid SPT due to positive dermatographism.
All children of control group underwent a complete SPT panel. Five/45 (11%) were sensitised, all had positive SPT to raw egg, 3/5 to boiled egg too. One hundred percent of sensitised children vs. 67% of non-sensitised children were breastfed (p=ns).
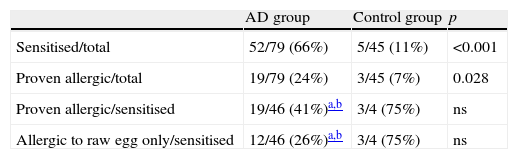
The differences in sensitisation rates between AD group (52/79=65.8%) and Control group (5/45=11%) leads a child with AD to have 5.9 Relative Risk (RR, C.I.=2.2–15.9) and 15.4 Odds Ratio (OR, C.I.=5.4–43.6) of being sensitised to egg before eating it (p<0.001, Table 2).
Egg sensitisation and allergy in AD group and control group.
In AD group 36/52 sensitised children performed OFC (12 both with raw egg and with boiled egg, 11 with raw egg only, 13 with boiled egg only). Seventeen/36 (47%) had at least one positive OFC (seven either with raw egg or with boiled egg); ten of them with positive OFC to raw egg underwent a SPT with both raw egg and the commercial extract of albumen and yolk, the latter tested negative for two of them. Nineteen/36 children (53%) had negative OFC, but 12 of them performed OFC only with boiled egg. Symptoms that occurred during OFC were urticaria, vomiting, abdominal pain, asthma, rhino-conjunctivitis. Sixteen/52 sensitised patients in AD group did not undergo OFC in hospital setting as their parents refused to consent. Of these, 10 children ate egg at home under parents’ decision and responsibility. Two/10 had an adverse reaction; one had a general reaction (urticaria and vomiting) with raw egg, one an anaphylactic reaction (urticaria and asthma) with boiled egg. Then, 46/52 sensitised children of AD group ate egg for the first time (36 OFC+10 at home), 19/46 (41%) resulted allergic (Table 2). 27 of the enrolled 79 children with AD had negative SPT, 17/27 consumed egg at home without adverse reactions.
Five children in the control group were sensitised to egg, four received raw and heated egg in hospital and three resulted allergic to raw egg only (Table 2). Symptoms were the same as those children in the AD group.
The minimum SPT that led to positive reaction in the raw egg challenge was 3mm and in the boiled egg challenge was 5mm.
Systemic reactionsFourteen children in AD group (30% of 46 sensitised children who ate egg) had a systemic reaction: three anaphylactic reactions and 11 generalised reactions. Some details are given below.
Fifty-three percent (42/79) of children in AD group were affected by mild AD, 17 were sensitised and, when they ate egg for their first time, had one organ reaction (six children with raw egg) or generalised reactions (five children, three with raw egg and two with boiled egg). Forty-two percent (33/79) of children in AD group were affected by moderate AD, 17 were sensitised and, when they ate egg for the first time, had one organ reaction (four children, three with raw egg and one with boiled egg), or generalised reaction (six children, three with raw egg and three with boiled egg), or anaphylactic reaction (three children, one with raw egg and two with boiled egg). Four children of AD group (5%) had severe AD, and only one of them (25%) ate egg, without adverse reactions.
In the Control Group, one patient sensitised to raw egg showed a generalised reaction after the ingestion of raw egg.
DiscussionWe have found that a child with AD has a RR of sensitisation to egg, before eating it, six times higher than a child without AD. Based on modelling studies that provide estimates of the magnitude of effect that is very unlikely to be explained by bias, the GRADE system defines a large effect as a relative risk (RR) of >2.0 or <0.5 (based on consistent evidence from at least two studies, with no plausible confounders) and a very large effect as a RR of >5.0 or <0.2 (based on direct evidence with no major threats to validity).15 This means that it is highly unlikely that our result is due to bias.
Why this happens is not known with certainty. The possible role of maternal milk, hypothesized by Han et al.,16 is not confirmed in our study in so far as the percentage of breastfed children was similar with regards to sensitised and non-sensitised children in both of the groups. In any case, this would not explain why just the children with AD have such an elevated RR. It is possible that the increase of the RR can be explained by transdermal sensitisation, helped by the lesions of AD.17 Anyway, 19/46 (41%) sensitised children with AD who ate egg for the first time, resulted allergic to it, and 3/19 (16%) showed an anaphylactic reaction according to a conservative definition.13 We believe that this is a problem that deserves to be prevented. How do we do with the best cost/benefit?
Skin prick test results should not influence the timing of egg introduction in the diet. However, it is true that some paediatricians, for fear of a serious adverse reaction, might suggest to delay the ‘introduction of’ egg in children with positive SPT. Well, this precaution would probably be insufficient, at least for the first three years of life. In fact, De Boisseau et al.3 reported that 75% of children with AD and sensitisation to egg were still allergic at the age of two and a half. Moreover, it does not seem safe to avoid raw or undercooked egg: in at least four studies1,4–6 adverse reactions were reported in children with AD who had eaten lyophilised or boiled or baked egg. In our study too, there were no differences in the adverse reactions, after the ingestion of raw or boiled egg.
Lastly, we assume that a general practitioner may perform SPT with boiled and raw egg (in our experience, SPT with commercial extract of albumen failed to identify two children with AD who were allergic to raw egg) in all children with AD. We think that all sensitised children should be referred to an allergist, to perform OFC in a hospital setting. However, we know that this is not always possible. This depends on how easy is too access an allergist centre and on economic and human resources. For example, by considering that the actual prevalence of AD in Italy varies from 7% to 17%,18 it can be predicted that every year there should be in Lazio (our area) about 2000 new cases of children with AD sensitised to egg who should be undergo OFC.
On the other hand we can consider the project proposed by Vlieg-Boerstra et al.19 They formulated a home programme for first egg administration and for administration of other trigger foods in children with a high risk of food allergies. A schedule was given to the parents together with pictures showing the precise amount of food to be given. For a boiled egg, this could begin with a “very small crumb”, followed by “a small crumb”, then 1/8 of a teaspoon, 1/2 a teaspoon, 1/3 of an egg and so on. The first three doses were given on the same day in three-hourly intervals, the fourth and fifth doses on the second day and so on. Parents should have stopped giving the egg at first sign or symptom. The main problem of this schedule is that the safety of the procedure has not been well demonstrated.
Another possibility could be to give biscuits or cakes made with eggs and wheat as first step, instead of raw or cooked eggs right away. However, some studies5,6 showed that adverse reaction at the ingestion of baked cake with egg was possible in patients with AD who had never eaten it. In addition, it has not been shown that taking the baked egg reduces the risk of adverse reaction to raw or undercooked egg.
Our management suggestions concerned egg only, even if children with AD can be allergic to other foods. A higher risk of adverse reaction at first ingestion has never been described for any food other than egg in children with AD, but every paediatrician and every paediatric allergist knows that this eventuality is possible with other foods, first of all milk. However, we feel that we can only make management recommendation based on published experience, as indeed was the case for adverse reactions to egg in children with AD.
Our study has some limitations, it includes only children admitted to a specialist unit and the AD group was retrospectively enrolled while controls were found prospectively. However, the access to a specialist unit does not limit the generalisability of our observations, the majority of visited children do not have severe or complicated AD; parents request, regardless of the severity level of eczema, if an allergic cause was possible. The age range of children included is broad and could give rise to the suspicion that some of the oldest have, during their life, swallowed the egg. However, we have collected the medical history very carefully, and all parents have categorically ruled out that their child had ever ingested egg in any form. In Italy, it is possible that children with AD avoid the egg until the age of 4 or 5 years. Moreover, Eigenmann also reported a 4-year-old girl with AD who had never ingested egg and turned allergic to raw egg.20
Seven percent of children in the control, non-atopic group, were allergic to egg, this may seem unbelievable. One possible explanation could be the absolute rarity of the raw egg in the diet of the infant: in fact all the controls were allergic only to raw egg, not to boiled egg (which is usually given to the infant).
A child with AD has a RR of sensitisation to egg six times higher than a child without AD, before the first ingestion. Severe reactions may occur even in children who undergo OFC with boiled egg and seem to be independent of the severity of eczema.
We propose to test sensitisation to egg in every child with AD who has never eaten it, and to perform OFC in those SPT positive in a hospital setting.
What is known on this subject
- •
Children with atopic dermatitis (AD) have an increased risk of IgE-mediated allergic reaction to their first ingestion of egg.
- •
The adverse reaction can also be caused by ingestion of heated egg.
- •
The adverse reaction can also be severe in children with mild atopic dermatitis.
What this study adds
- •
Children with AD have a six times higher risk of having specific IgE to egg before eating it than children without AD.
- •
If egg-specific IgE are positive, children with AD have similar risk of allergic reactions at first egg ingestion than children without AD.
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Patients’ data protectionConfidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentRight to privacy and informed consent. The authors have obtained the informed consent of the patients and/or subjects mentioned in the article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Contributorship statement- •
Stefano Miceli Sopo conceived the study, designed the study and approved the final version.
- •
Serena Monaco played the part of clinical care and contributed to drafting the manuscript.
- •
Valentina Giorgio and Salvatore Tripodi made data acquisition and analysis.
- •
Mauro Calvani and Roberta Onesimo made acquisition and interpretation of data and helped draft the manuscript.