Asthma is one of the diseases which has a high prevalence in developed and developing countries. The relationship between asthma and obesity has always been focused by researchers. In this field, adipokines, especially adiponectin and leptin have highly attended by the scientist. The aim of this study was to determine the serum level of adiponectin, leptin and the leptin/adiponectin ratio in asthmatic patients and its relationship with disease severity, lung function and BMI (body mass index).
MethodsIn this cross-sectional study, 90 asthmatic women admitted to the tertiary referral hospital in Kurdistan province – Iran, were examined. First, BMI was measured and then pulmonary function tests were performed in all asthmatics patient. Forced expiratory volume in 1s (FEV1), forced vital capacity (FVC), and FEV1/FVC, were measured. At the end, blood samples were collected and serum level of adiponectin and leptin were measured by ELISA method.
ResultSerum leptin and leptin/adiponectin levels correlated positively with asthma severity and BMI (p=0.0001), but there was no correlation between adiponectin level with asthma severity and BMI (p>0.05), also serum leptin and leptin/adiponectin levels inversely correlated with FEV1 and FVC in patient (p=0.0001).
ConclusionAsthma is linked with obesity, and there is an association between asthma severity and BMI with serum leptin and leptin/adiponectin levels, but our results do not support a significant role of adiponectin in obesity or asthma.
Several studies have reported the spread of asthma and obesity as a health problem in the world.1–4 The prevalence of obesity in America (BMI ≥30kg/m2) in 20–74 year adults has increased from 15% in 1970 to 35% in 2010. The World Health Organization has estimated the number of obese or overweight people in the world as 2 billion people.5
Asthma is also one of the diseases which has a high prevalence in developed and developing countries so that asthma and allergy has affected 1/3 of the children in some Western countries.6,7 Asthma has affected 22 million people in America and 300 million people in the entire world.8 In Iran, according to the statistics provided by allergy and asthma clinic, 10% of people are suffering asthma.9
The relationship between asthma and obesity has always been focused by researchers, and different studies have indicated various results in this area.10–12 Epidemiological studies indicate that the lifestyle is one of the most important factors affecting asthma. These studies consider the role of inactivity and consumption of high-calorie foods in the prevalence of asthma. High-calorie diet with inactivity leads to obesity in adolescents and adults.13 Longitudinal surveys have shown that obesity is the beginning of asthma and the relative risk of asthma is aggravated by obesity.14 The mechanisms of developing this relationship could include mechanical effects such as constriction of respiratory tract due to smooth muscles of the of the airways, the effects of adipose tissue on the immune system function, hormonal factors, nutritional factors and inactivity.15 As possible mechanisms through which obesity could lead to the development of asthma in adults, decreased lung function by changing the balance of inflammatory and pre-inflammatory cytokines along with a diet, obesity, atopy and hormonal effects have been discussed.16 Disruption of immune tolerance due to cytokines and adipokines associated with obesity, is another mechanism that links obesity to asthma and autoimmune diseases.
Despite much research, the relationship between asthma and obesity remains unclear and has not been definitively identified and confirmed.10,11 Adipokines, especially adiponectin and leptin have highly attended by the scholars in this field. Leptin plays an important role in the regulation of appetite, body weight and energy balance. Leptin and its receptors which are expressed on the surface of the airways can be associated with asthma. Leptin is a pro-inflammatory factor that affects the innate and adaptive immune system, and increases in obese individuals as well.17
Unlike leptin, adiponectin reduces in obese people and is considered as an anti-inflammatory factor that inhibits proinflammatory cytokines (TNF-a, IL-6, and nuclear factor kB) and the stimulation of anti-inflammatory cytokines (IL-10 and IL-1 receptor antagonist).17 According to the above information, the hypothesis of the relationship between adipkine and asthma was established. Animal studies strengthened this hypothesis.18 It became clear that adiponectin reduces allergen-induced airway inflammation and hyperresponsiveness in mice.19 Some human studies have relatively supported the hypothesis. In a case–control study in premenopausal women, it was guessed that leptin may be a dependent risk factor for asthma.20 In another study, it was found that a high serum adiponectin concentration may protect against current asthma in premenopausal women but does not explain the association between asthma and adiposity.21 However, some human studies have not support the hypothesis and did not report any relationship between adipokines and asthma.22,23
Therefore, this hypothesis has not been definitely confirmed in human studies and there is a need for more studies.24 The aim of this study was to determine the serum level of adiponectin and leptin, and leptin/adiponectin ratio in asthmatic patients and its relationship with disease severity, lung function and BMI.
MethodologyStudy populationIn this cross-sectional study the study population is comprised of asthmatic women admitted to tertiary referral hospital in Kurdistan province-Iran.
Inclusion criteriaThe individuals were examined by asthma and allergy specialists and their illnesses were confirmed according to GINA and spirometric criteria. Then, they were entered the study.
Exclusion criteriaHaving other allergic diseases at the same time, the use of corticosteroids for two weeks before blood collection, the use of asthma medications such as bronchial dilators 24h before sampling, other acute and chronic diseases including upper and lower respiratory system infections and finally the presence of any infectious disease for at least the past two months.
Sample size and sampling methodSamples were selected using a convenience sample method. Considering the 5% type I error, study power of 95%, the sample size was calculated as 60 where 90 samples were studied in order to increase accuracy. Therefore, 90 patients were randomly selected from among the patients with asthma who were admitting the tertiary referral hospital of Kurdistan-Iran. Patients were enrolled deliberately and after filing consents.
Practical and hormonal testsThe height of all the subjects was measured by a standard wall-mounted stadiometer and their weight was also measured by calibrated electronic scales. BMI was calculated by the ratio of weight to height.
Pulmonary function tests in all patients were performed by using a spirometer (spirolab III-Italy). ATS guideline was used to interpret the information from.
Blood samples of the individuals were collected by skilled and qualified technicians. After 10min after being centrifuged at 3000rpm, the serum was separated and stored at −70°C. The samples were thawed before being examined and serum level of adiponectin and leptin was measured according to the manufacturer's instructions (Bioassay technology laboratory – China), and according to the enzyme-linked immunosorbent assay (ELISA).
Ethical considerationsAll moral codes regarding the study and the confidentiality of information were observed, and also informed consent form was obtained from the subjects. No additional process was performed on the patient.
Statistical analysisData analyzed using SPSS15 software. Quantitative variables were expressed and reported as mean±standard deviation and confidence interval based on three variables; leptin, adiponectin and leptin/adiponectin ratio. For relationship between leptin and asthma severity, since, the severity of asthma is a ranking variable and the amount of leptin is a ratio variable, ANOVA and Tukey POST HOC test has been used. Since, the severity of asthma is a ranking variable and the level of adiponectin is a ratio variable, Kruskal–Wallis test was used for relationship between adiponectin and asthma severity. Since, the severity of asthma is a ranking variable and the ratio of leptin/adiponectin is a ratio variable, Kruskal–Wallis test was used for relationship between the ratio of leptin/adiponectin with asthma severity. Because the two variables of BMI and leptin, adiponectin and the leptin/adiponectin ratio were two quantitative (ratio) variable, Pearson and Spearman correlation tests were used. To determine the relationship between leptin and BMI with normal distribution, Pearson correlation test was conducted. To investigate the relationship between the two variables of adiponectin and BMI, as adiponectin was not normally distributed, Spearman correlation test was used.
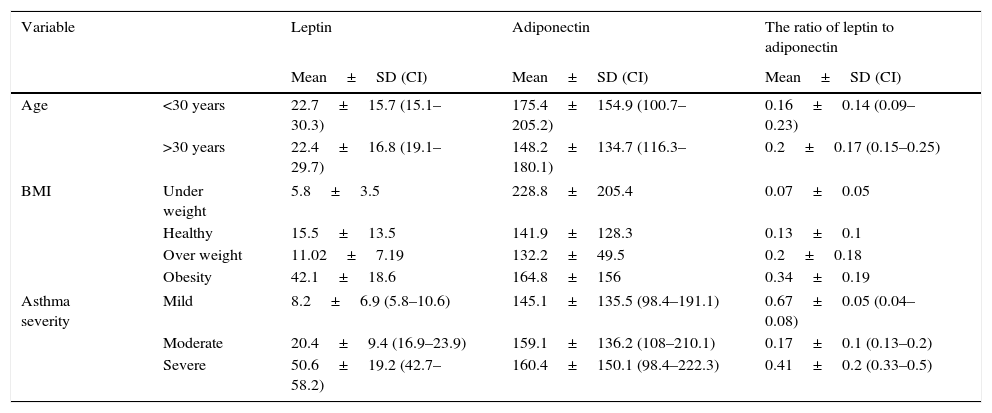
ResultsThe descriptive information (mean and standard deviation, confidence interval) of serum levels of adiponectin, leptin and leptin/adiponectin ratio in patients with asthma has been presented in Table 1 by age, BMI and severity of symptoms. As can be seen from the first part, by aging, serum level of adiponectin indicates a decreasing trend. But this change has not been observed in leptin hormone. Mean (± SD) and severity of asthma symptoms were also evaluated. 38.89% of the subjects had mild asthma (8.22±6.91), 33.33% had moderate asthma (20.46±9.45) and 27.78% (50.84±19.68) had severe asthma.
Determining serum level of adiponectin, leptin and the ratio of leptin to adiponectin in patients with asthma, according to age groups, BMI and severity of asthma symptoms.
| Variable | Leptin | Adiponectin | The ratio of leptin to adiponectin | |
|---|---|---|---|---|
| Mean±SD (CI) | Mean±SD (CI) | Mean±SD (CI) | ||
| Age | <30 years | 22.7±15.7 (15.1–30.3) | 175.4±154.9 (100.7–205.2) | 0.16±0.14 (0.09–0.23) |
| >30 years | 22.4±16.8 (19.1–29.7) | 148.2±134.7 (116.3–180.1) | 0.2±0.17 (0.15–0.25) | |
| BMI | Under weight | 5.8±3.5 | 228.8±205.4 | 0.07±0.05 |
| Healthy | 15.5±13.5 | 141.9±128.3 | 0.13±0.1 | |
| Over weight | 11.02±7.19 | 132.2±49.5 | 0.2±0.18 | |
| Obesity | 42.1±18.6 | 164.8±156 | 0.34±0.19 | |
| Asthma severity | Mild | 8.2±6.9 (5.8–10.6) | 145.1±135.5 (98.4–191.1) | 0.67±0.05 (0.04–0.08) |
| Moderate | 20.4±9.4 (16.9–23.9) | 159.1±136.2 (108–210.1) | 0.17±0.1 (0.13–0.2) | |
| Severe | 50.6±19.2 (42.7–58.2) | 160.4±150.1 (98.4–222.3) | 0.41±0.2 (0.33–0.5) | |
Then, the relationship between adiponectin, leptin and leptin/adiponectin ratio with asthma severity is identified.
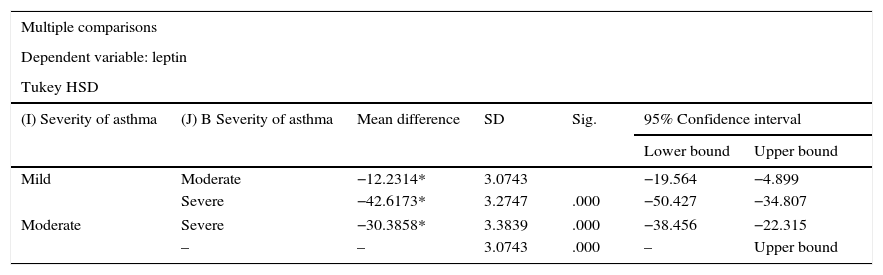
The relationship between leptin and asthma severityThe results of Table 2 indicates that the serum leptin levels varies in patients with different asthma severity (mild, moderate, severe), and is statistically significant (p=0.0001) and the POST HOC test indicates a significant difference (p=0.0001) between the three groups regarding the severity of asthma (mild, moderate, severe). So that the mean and standard deviation of leptin in patients with mild asthma, is lower than leptin in patients with mild and severe asthma. Leptin is also lower in patients with moderate asthma, compared to patients with severe asthma. In fact, there is a positive relationship between leptin serum level and asthma severity (Table 2).
The relationship between leptin and severity of asthma in patients.
| Multiple comparisons | ||||||
|---|---|---|---|---|---|---|
| Dependent variable: leptin | ||||||
| Tukey HSD | ||||||
| (I) Severity of asthma | (J) B Severity of asthma | Mean difference | SD | Sig. | 95% Confidence interval | |
| Lower bound | Upper bound | |||||
| Mild | Moderate | −12.2314* | 3.0743 | −19.564 | −4.899 | |
| Severe | −42.6173* | 3.2747 | .000 | −50.427 | −34.807 | |
| Moderate | Severe | −30.3858* | 3.3839 | .000 | −38.456 | −22.315 |
| – | – | 3.0743 | .000 | – | Upper bound | |
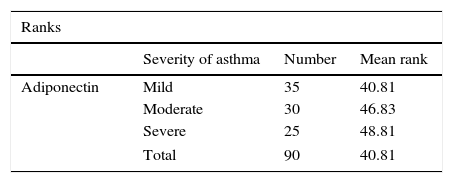
The results of Table 3 indicates that the average ranking of adiponectin in asthma severity (mild, moderate, severe) has no statistically significant difference (p=0.451) (Table 3).
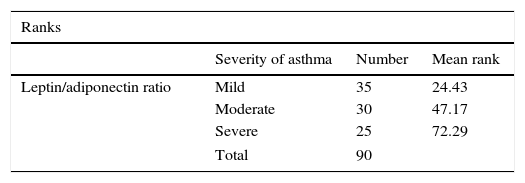
The relationship between leptin/adiponectin ratio with asthma severityAs Table 4 indicates, the average rank of leptin/adiponectin ratio between asthma severity (mild, moderate, severe) indicated a statistically significant difference (p<0.0001). In fact there is a positive relationship between the leptin/adiponectin ratio and increased severity of asthma and by increasing the severity of asthma, the ratio of leptin/adiponectin increases (Table 4).
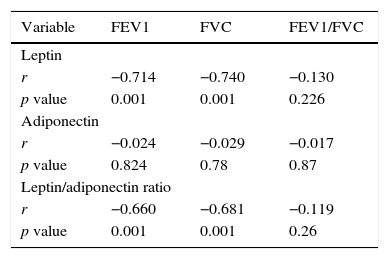
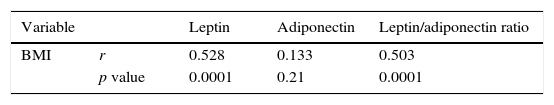
In Table 5, the relationship between adiponectin, leptin and the leptin/adiponectin ratio has been provided with the pulmonary function tests. As can be observed, there is a significant relationship between the serum level of leptin, adiponectin and the ratio of leptin to adiponectin with FVC and FEV1 (p<0.05). To determine the relationship between leptin and BMI with normal distribution, Pearson correlation test was conducted so that there was a significant correlation between the two variables (r=0.52) (p=0.0001). To investigate the relationship between the two variables of adiponectin and BMI, as adiponectin was not normally distributed, Spearman correlation test was used and no significant correlation was observed (p=0.21), but the ratio of leptin to adiponectin and BMI (Spearman correlation) was equal to (r=0.503) and statistically significant (p=0.0001) (Table 6).
Correlation of leptin, adiponectin and the ratio of leptin/adiponectin with FEV1, FVC and FEV1/FVC.
| Variable | FEV1 | FVC | FEV1/FVC |
|---|---|---|---|
| Leptin | |||
| r | −0.714 | −0.740 | −0.130 |
| p value | 0.001 | 0.001 | 0.226 |
| Adiponectin | |||
| r | −0.024 | −0.029 | −0.017 |
| p value | 0.824 | 0.78 | 0.87 |
| Leptin/adiponectin ratio | |||
| r | −0.660 | −0.681 | −0.119 |
| p value | 0.001 | 0.001 | 0.26 |
The aim of this study was to investigate the relationship between serum levels of adiponectin, leptin and leptin/adiponectin ratio in women with asthma severity, lung function, as well as the BMI. According to the findings of the present study, there was a positive relationship between serum levels of leptin and leptin/adiponectin ratio with the severity of asthma symptoms, so that the increase in these two markers, the severity of asthma has also increased. In this regard, few studies have investigated adults with asthma. In a similar study conducted by Agori et al., they indicated that leptin hormone level in patients with asthma and the ratio of leptin/adiponectin is higher in comparison with the control group, and the two values also increase with the increasing asthma severity.23 During a cohort study conducted by Jarttil, the relationship between leptin and asthma symptoms in three different periods of 3–18 years, 9–24 years and 24–39 years was investigated. The results indicated that leptin hormone has a positive and significant correlation with the severity of asthma at the age range of 24–39.25 In a population based, cross sectional study, Sood et al. indicated that the level of leptin is high in adults with asthma, especially women, compared to the healthy subjects.20
According to these results, these two indices can be seen as a marker to determine the severity of asthma. Leptin can play a key role in the pathophysiology of asthma. Some studies have indicated that leptin level increases during inflammation26,27 and in turn promote inflammation. Increased expression of leptin mRNA in adipose tissue of mice, after the injection of proinflammatory cytokines such as tumour necrosis factor (TNF-a) and IL-1 were the confirmation to this claim.26
Previous studies have shown that IL-17 could be involved in asthma exacerbations. It is known that when naive splenic CD4+T grows in the presence of Th17, the injection of leptin can exacerbate the production of Th17.28 Leptin also inhibits the function of regulatory T cells (T regs) and it is expected to strengthen the activity of allergen induced T-cell.29 Other studies have shown that there is such a relationship between leptin serum level and asthma severity in children.30,31
However, in the study by Dixon, although leptin level indicated a positive relationship with the severity of asthma, but it was not statistically significant.22 The results of these studies may be due to differences in study designs, or a different sample size in them.
In this study, no significant relationship was observed between the adiponectin serum level and asthma severity. Such results were also reported in a study by Dixon et al.22
In a study conducted by Sood et al., the role of adiponectin on asthma and its symptoms were evaluated, but there was no difference in serum adiponectin concentrations between the current asthma and never asthma groups in men and women combined.21 Hayashikawa et al. conducted a study to examine the association between adiponectin and asthma and pulmonary function in Japan. The results indicated that the serum total adiponectin level was not significantly different between asthmatic subjects and control non-asthmatic subjects in both sexes in both groups.32 This marker appears to have less value and importance in determining the severity of asthma.
According to the findings of the present study, there is a negative and significant relationship between serum levels of leptin and the leptin/adiponectin ratio in patients with FEV and FCV pulmonary function tests. The increase in leptin in patients with asthma was associated with a reduction in lung function. But the serum level of adiponectin was not associated with these tests. This finding is consistent with the results of the study conducted by Agori.23 In a study to evaluate the immune response and lung function in adults with asthma, Dixon et al. indicated that both forced expiratory volume in 1s (FEV1) and forced vital capacity (FVC) were significantly lower in asthmatics than in non-asthmatics.22
In a study conducted by Hickson et al., they investigated the relationship between leptin serum level with FEV1, FEV in 6s (FEV6), and vital capacity (FVC). The results indicated that the increased level of leptin is associated with reduced FEV1, FEV6, and FVC%.33 Animal studies have indicated that leptin regulates the lungs physiological function. Six isoforms of leptin receptors have been identified in lung tissue and Ob-Rb isoform has had the highest concentration on epithelial cells of the lung.34 In another study aimed to investigate the role of leptin receptors in the lungs, it became clear that these receptors also exist in human lungs and increased levels of leptin have stimulatory effects on the human respiratory.35
A positive and significant correlation was observed between serum level of leptin, and leptin/adiponectin ratio with the patients’ BMI in this study. But no significant relationship was observed in case of adiponectin. The relationship between these two hormones and leptin/adiponectin ratio with asthma severity and BMI is still contradictory after several studies. According to the results of the present study, the direct correlation between leptin hormone and leptin/adiponectin ratio with BMI is possible. And an increase in BMI can predict the severity of asthma. In a study conducted by Salah et al., these biomarkers and BMI were examined in non-obese control, obese control, non-obese asthmatics and obese asthmatics. The results indicated that in obese patients with asthma, and obese individuals, serum level of leptin and adiponectin are higher than the control group. In this study, obesity criteria was considered BMI >30.35 In a study conducted by Sutherland et al., a positive and significant correlation was reported between the leptin hormone and BMI in adults.36 In the study conducted by Agori et al., BMI indicated a significant relationship with the severity of asthma.23 In the study conducted by Jartti et al., the relationship between obesity, leptin and adiponectin biomarkers with BMI were investigated in three age periods in healthy subjects and patients with asthma. The results showed that in adulthood, increasing BMI an independently (from adipokines) be a predictor of asthma.25 Sood et al. after adjustment for serum levels of leptin indicated that the relationship between BMI and asthma was attenuated but remained a borderline significance.20 This means that perhaps the relationship between BMI and asthma is not much affected by leptin. And this relationship is also affected by other pathophysiologic pathways. As mentioned, this relationship has remained unclear and requires further investigation.
ConclusionIn this study, leptin hormone indicated a relationship with the severity of asthma, reduction in lung function, and increased BMI. As mentioned, this hormone is a key factor in obesity and can be involved in the inflammatory process of asthma. However, it can be helpful in predicting the severity of asthma and pulmonary function of the individuals. In this study, adiponectin had no relationship with asthma severity and pulmonary function of the patients. Perhaps this biomarker is less important in predicting asthma, however, the small sample size in this study and type of study design were the limitations of this study which was not able to accurately investigate the role of this biomarker in patients with asthma.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Protection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
Conflict of interestThe authors declare that they have no conflict of interest.
This study was the result of a research project approved by the Research deputy of Kurdistan University of Medical Sciences and it was conducted under its financial support. We would like to appreciate those who paid special attention to this project.