Respiratory allergy is characterised by an IgE-mediated reaction. The immune system functions, including IgE production, progressively decline over time, such as growing up and ageing. Molecular-based allergy diagnostic defines sensitisation profile. This study aimed to evaluate the impact of age on serum allergen-specific IgE to molecular component levels in a large sample of subjects.
MethodsSerum IgE to: Phl p1, Bet v1, Ole e1, Cup a1, Par j2, Can f1, Der p2, and Fel d1 were assessed by ISAC method. Sera from 2788 patients, 1230 males (44.1%) and 1558 females (55.9%), median age 23 years (1st and 3rd quartiles: 9.7–49.7 years; age range: 1 month–103 years) were analysed.
ResultsThe number of positive tests (i.e. sensitisation) tended to increase between birth and school-age till young adulthood and then decreased (p<0.0001) with the exception of Fel d 1 (p=0.14). A similar age-dependent trend was observed considering the levels of each allergen components: the levels of each allergen component, with the exception of Fel d 1, tended to increase till early adulthood and then to decrease reaching the lowest levels in the elderly.
ConclusionsAllergen-specific IgE production to inhaled molecular components trend to reduce with ageing, but with differences between allergens. This phenomenon should be adequately evaluated managing allergic patients.
Respiratory allergy, such as allergic rhinitis and asthma, has a negative impact on patients, as it may negatively affect the school and job performance, the daily activities, and the quality of life. This fact is impressively amplified by allergy prevalence: up to 40% of the general population.1,2 The hallmark of the immune reaction in allergic patients is the on-going production of allergen-specific IgE. This phenomenon is defined sensitisation and can be considered the condicio sine qua non for detecting allergy. The natural history of allergy is frequently characterised by an increasing number of sensitisations (such as the poly-sensitisation phenomenon), also during childhood.3,4 Poly-sensitisation is an immunological event that is relevant from an epidemiological and clinical point of view.5–7 The poly-sensitisation prevalence ranges from 20% to 90%, with a great variability depending on the investigated population.5–7 Nevertheless, a fundamental concept must be pointed out: sensitisation, such as the mere production of allergen-specific IgE, does not always correspond to true allergy, such as symptom occurrence after exposure to the sensitising allergen. Therefore, the terms sensitisation and allergy are not synonymous. The allergy diagnosis is rigorously based on the formal demonstration of a consistency between sensitisation and the history of symptoms occurrence after inhaling the sensitising allergen.
Sensitisation can be demonstrated in vivo (by skin prick test) or in vitro (by serum IgE measurement). Traditionally, natural allergen extracts from allergenic sources are used in the common practice. However, the extract mixtures are usually heterogeneous because they may include not only the major allergens, but also cross-reactive allergens, non-allergenic antigens, and interfering substances.8,9 To remedy this bias, molecular-based allergy diagnostic tests have been recently introduced in clinical practice, allowing to define and characterise exactly the sensitisation profile.10 This methodology is based on allergen molecular components that are involved in the specific immune response to allergens. Allergen molecules may be purified, recombinant, or synthetic. The use of molecular allergen components has changed the allergy workup, being highly useful in poly-sensitised patients, mainly concerning the allergen-specific immunotherapy prescription.11 In fact, the positivity to major allergens excludes false reactivity to pan-allergens. In other words, a patient may be sensitised to many allergens, but he/she may be allergic only to a few (or even to none!).
On the other hand, a progressive decline of almost all the functions of organs and systems characterises ageing.12 In particular, ageing significantly affects the immune system with relevant changes, defined as “immune-senescence”.13–15 There is evidence that allergy prevalence trends to decline with age. A Dutch general population study documented that serum IgE levels were lower in the oldest subpopulation, such as 45–70 years.16 This result was confirmed in stratified population sample with an age range between 8 and 73 years.17 Another study, conducted on a general population with age between 19 and 99 years, also confirmed that the elderly subjects had the lowest IgE levels.18 Moreover, studies on allergic patients reported consistent findings: the older patients usually have the lowest IgE levels.19–23 However, these surveys were usually conducted on relatively limited samples of allergic patients, seldom with narrow age ranges, and rarely evaluating allergen molecular components.
The present study tested the hypothesis that age could also impact on allergen-specific IgE production to the inhaled molecular components. Therefore, we enrolled a large cohort of patients measuring serum IgE to the most common allergens.
Materials and methodsPatientsThis retrospective study considered subjects suffering from respiratory complaints suggestive for allergy. They went to the Laboratory of the Istituto Giannina Gaslini of Genoa, Italy, for serologic assessment between July 2012 and April 2014. We analysed the findings of serum allergen-specific IgE to the following molecular components: Phl p1, Bet v1, Ole e1, Cup a1, Par j2, Can f1, Der p2, Fel d1, assessed by the ISAC method.
All patients gave written informed consent and the Review Board of the IRCCS-AOU San Martino approved the procedure.
IgE assaySerum IgE were measured by ISAC test according to the manufacturer's recommendations (Thermo-Fisher Italy, Milan, Italy). Synthetically, 20μL of the patient's serum were incubated on the microchip containing 112 allergen spots. After 1-h incubation, slides were washed and a monoclonal anti-IgE antiserum labelled with a fluorochrome was added and incubated for 1h. Then slides were re-washed and the chips were analysed by a Laser Scan Confocal microarray reader (LuxScan 10K/A, CapitalBio, Beijing, China). A microarray Image Analyser immediately analysed the findings. All samples were identified using a single barcode. The results were calculated by the software. The ISAC score was considered as ISAC Standardized Units (ISU), ranging from 0 to 100.
Statistical analysisThe ISAC score was reported as ISAC Standardized Units (ISU), which ranges from 0 to 100 ISU. Positive finding, such as sensitisation, was defined as a value >0.3 ISU, according to the manufacturer's rules.
Patients were grouped according to their age as follows: Group 1: from birth to the end of the 1st year (early infancy); Group 2: from the beginning of the 2nd year to the end of the 5th year (preschool age); Group 3: from the beginning of the 6th year to the end of the 12th year (school-age); Group 4: from the beginning of the 13th year (first adolescence and secondary school) to the end of the 17th year (end of adolescence); Group 5: 18–20 years; Group 6: 21–30 years; Group 7: 31–40 years; Group 8: 41–50 years; Group 9: 51–60 years; Group 10: 61–70 years; Group 11: 71 years and older.
Within each allergen group, the number of positive tests in the different age groups, expressed as percentage, was also evaluated.
The Shapiro–Wilk test was used to evaluate the normal distribution. IgE levels were normally distributed and were summarised as means and 95% Confidence Intervals (95% CI); patients’ age was not normally distributed and therefore was reported as median with first and third quartiles. Comparisons in IgE levels among different age groups were performed using ANOVA test. Categorical variables (i.e. the percentage of positive tests) among age groups were compared using the Chi-square test or the Fisher's Exact test in case of expected frequencies less than five. A p value less than 0.05 was considered as statistically significant.
Statistical analysis was performed using the Statistica software package (release 9.0, StatSoft Corp., Tulsa, OK, USA).
ResultsSera from 2788 patients, 1230 males (44.1%) and 1558 females (55.9%), median age 23 years (1st and 3rd quartiles: 9.7–49.7 years; age range: 1 month–103 years) were analysed.
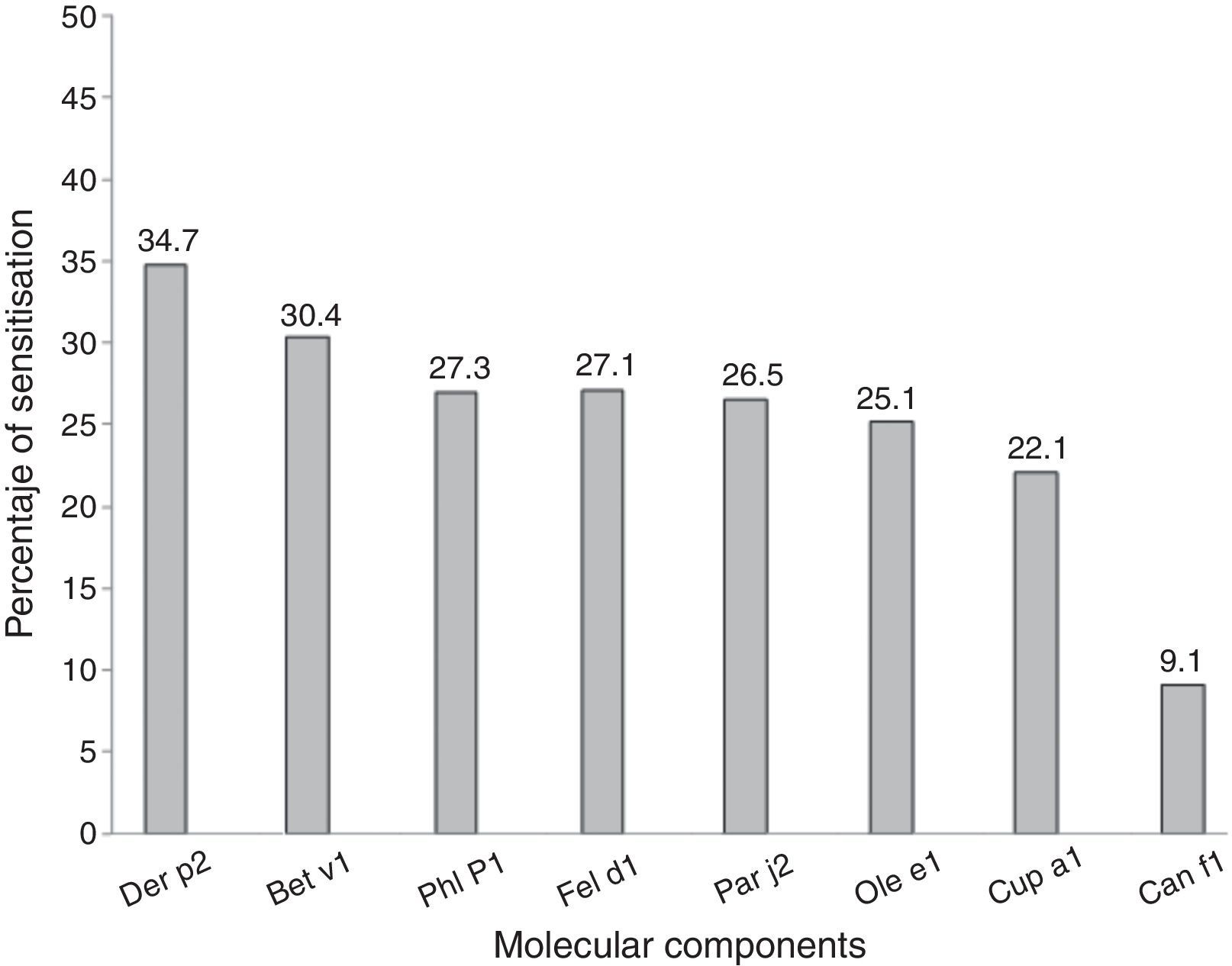
Most of the subjects were positive to Der p 2 (34.7%), followed by Bet v 1 sensitisation (30.4%) and Phl p 1 (27.3%). Only 9.1% of subjects were positive to Can d 1 (Fig. 1).
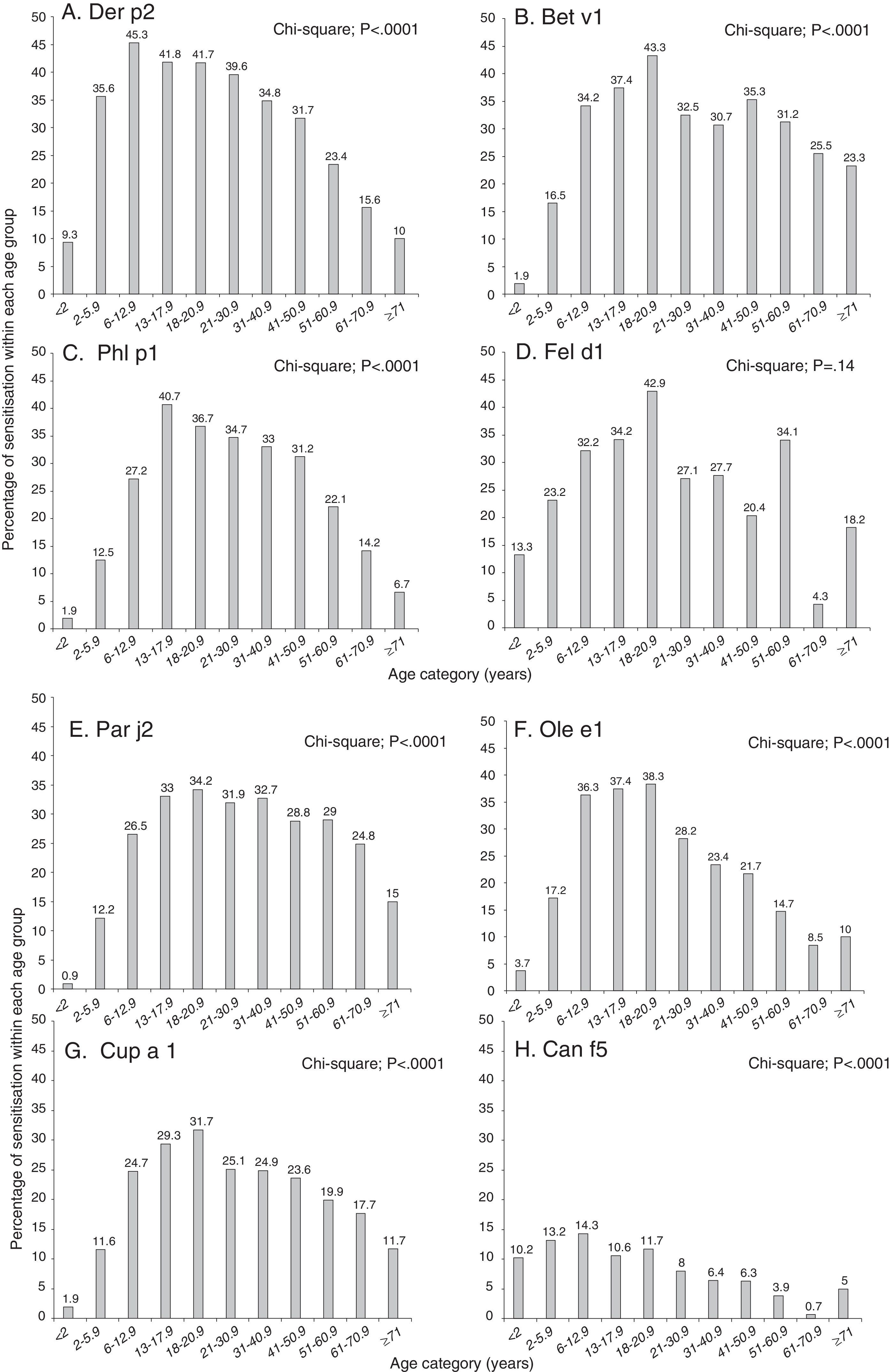
Analysing each allergenic molecular component separately, we found that the number of positive tests (i.e. sensitisation) tended to increase between birth and school-age till young adulthood and then decreased (p<0.0001) with the exception of Fel d 1 (p=0.14).
Particularly, the highest frequency of positive test for specific IgE in the youngest age (<2 years) was found analysing Fel d 1 (13.3%) (Fig. 2D) followed by Can f 1 (10.2%) (Fig. 2H) and Der p 2 (9.3%) (Fig. 2A); the lowest frequency of positive test for specific IgE in the youngest age was detected analysing Par j 2 being 0.9% (Fig. 2E).
Frequency of positive test for specific IgE for each allergen component according to the age of the patients: Der p1 (panel A), Bet v1 (panel B), Phl p1 (panel C), Fel d1 (panel D), Par j2 (panel E), Ole e1 (panel F), Cup a1 (panel G) and Can f1 (panel H). Patients were grouped according to their age as follows: early infancy (<2 years), preschool age (2 to <6 years), school-age (6 to <13 years), adolescence (13 to <18 years), 18–20 years, 21–30 years, 31–40 years, 41–50 years, 51–60 years, 61–70 years, 71 years and older.
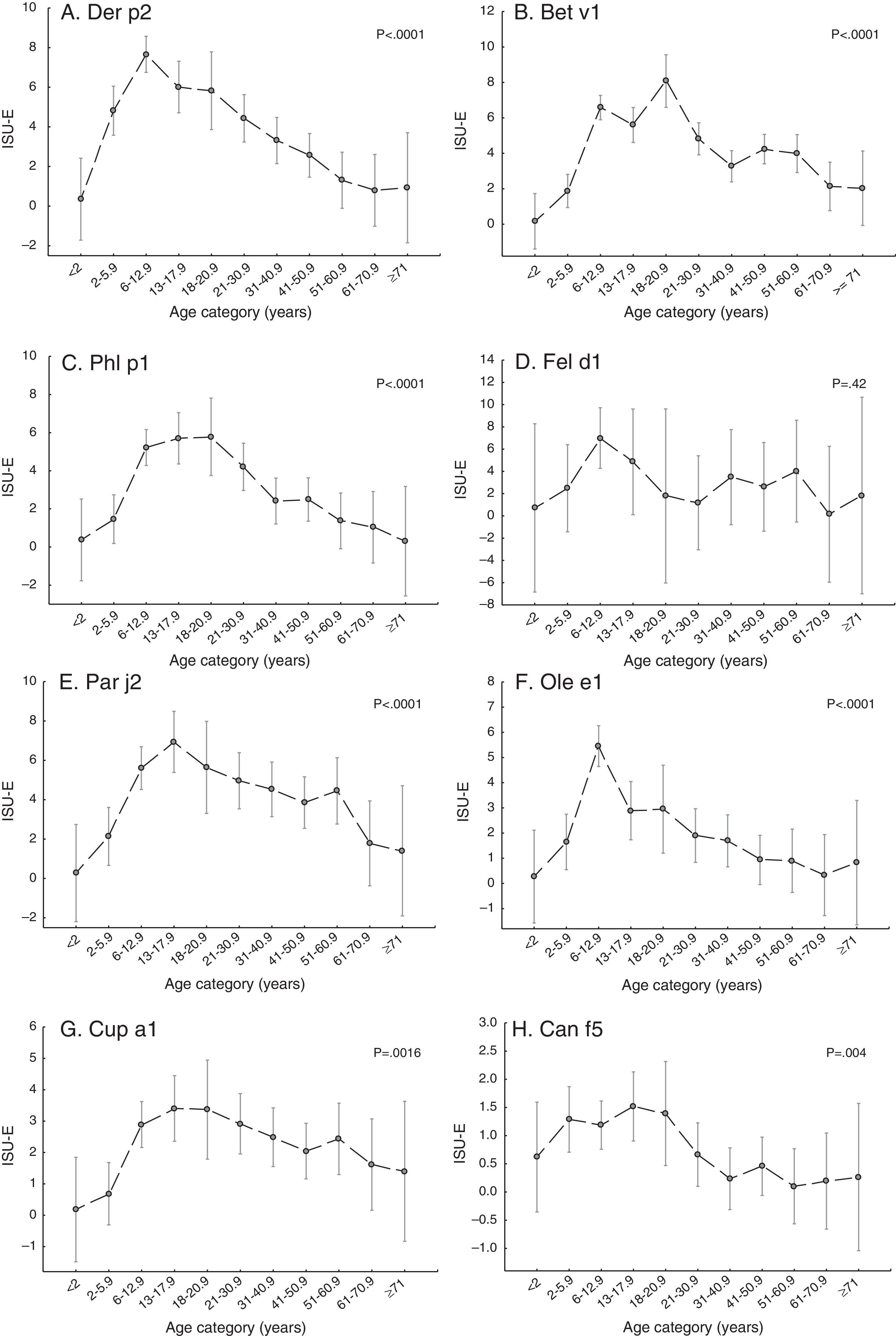
A similar age-dependent trend was observed considering the levels of each allergen component (Fig. 3): the levels of each allergen component, with the exception of Fel d 1 (Fig. 3D), tended to increase till early adulthood and then to decrease reaching the lowest levels in the elderly.
Levels of each allergen component according to the age of the patients: Der p1 (panel A), Bet v1 (panel B), Phl p1 (panel C), Fel d1 (panel D), Par j2 (panel E), Ole e1 (panel F), Cup a1 (panel G) and Can f1 (panel H). Levels are expressed as ISU-E. Patients were grouped by their age as follows: early infancy (<2 years), preschool age (2 to <6 years), school-age (6 to <13 years), adolescence (13 to <18 years), 18–20 years, 21–30 years, 31–40 years, 41–50 years, 51–60 years, 61–70 years, 71 years and older.
Detecting at what age the maximum levels of each allergen was reached, we found that the highest percentage of positive tests was reached in school-age children (from 6 to <13 years) for Der p 2 (45.3%) (Fig. 2A) or for Can f 1 (14.3%) (Fig. 2H); the peak frequency of positive tests was reached in early adolescence (from 13 to <18 years) for Phl p 1 (40.7%) (Fig. 2C) and in early adulthood (from 18 to <21 years) for Bet v1 (43.3%) (Fig. 2B), Fel d 1 (42.9%) (Fig. 2D), Ole e 1 (38.3%) (Fig. 2F), Par j 2 (34.2%) (Fig. 2E) and Cup a 1 (31.7%) (Fig. 2G).
Analysing the different allergen component levels according to the patients’ age, we found that during the first year of life, allergen levels were low (mean values lower than 1 ISU-E) independently from the allergen component. Then allergen levels tended to increase reaching a peak between 6 and 20 years, followed by a decrease that was more pronounced for Der p 2 (Fig. 3A), Phl p 1 (Fig. 3C), Par j 2 (Fig. 3E) and Ole e 1 (Fig. 3F). Specifically, the peak levels were reached in the school-aged children for Der p 2 (Fig. 3A), Fel d 1 (Fig. 3D) and Ole e 1 (Fig. 3F), between the first adolescence and the end of adolescence for Par j 2 (Fig. 3E), at the beginning of adult life for Bet v 1 (Fig. 3B). For both Phl p 1 (Fig. 3C) and Cup a 1 (Fig. 3G), the maximum allergen levels were found in children and young adults aged between 6 and 20 years. For Can f 5 (Fig. 3H), the maximum allergen levels were found in preschool age children and young adults aged between 2 and 20 years.
DiscussionThe definitive diagnosis of allergy is based on positive specific IgE test results. Allergen-specific IgE immunoassay is a reliable, standardised analytical method offering a better accuracy than skin prick test in recognising allergic patients.24 Serum IgE is commonly considered the typical biomarker for the allergic phenotype, as allergic disorders are paradigmatically characterised by an IgE-mediated inflammation. IgE measuring is therefore a popular way to diagnose allergy.
In addition, the recent commercial availability of new molecular tests allows a more accurate diagnosis, focused on the recognition of the true causative allergen; this property leads to a significant increase in test specificity because of the exclusion of false sensitisation due to cross-reactivity. However, in vitro molecular allergy tests are expensive, cannot be performed by all clinical laboratories, and their interpretation requires adequate specialist competence. Although molecular allergy tests are opening encouraging perspectives for the improvement of patient care, results should be evaluated with caution, taking into account the presence and the severity of clinical signs, since sensitisation does not necessarily correspond to true allergy.
On the basis of these assumptions, the present study aimed to investigate the age impact on the allergen-specific IgE production, assessed by molecular component analysis.
The present study was conducted on a large sample of subjects referring to serological assessment for suspected respiratory allergy diagnosis. The percentage of positive subjects, such as sensitised, was 34.7% for Der p 2, 30.4% for Bet v 1, 27.3% for Phl p 1, and 27.1% for Fel d 1, 26.5% for Pa j 2, 25.1% for Ole e 1, 22.1% for Cup a 1, and 9.1% for Can f 1. These findings confirm previous reports, showing that these eight allergens are the most relevant in our geographic area.25,26
Age has an impact on allergen-specific IgE in a different way for every allergen, both considering the sensitisation prevalence and the serum level distributions. Dermatophagoides sensitisation concerned essentially younger subjects, whereas sensitisation to pollen allergens typically showed a peak in the middle age. These conflicting findings could depend on the duration of allergen exposure: perennial for mites and seasonal for pollens. In other words, a continuous allergen pressure (e.g. mites) may induce a more intense and precocious sensitisation than a periodic one (e.g. pollens).
Considering the allergen-specific IgE levels in respect of the age, this study showed that each single allergen was characterised by a particular pattern. House dust mites were capable of inducing the earliest and more intense IgE response, but IgE production significantly and quickly declined over time. The relevant reduction might depend on typical immunological characteristic of mite allergen, but this hypothesis deserves adequate investigation. On the contrary, cat allergy is characterised by a persistence of IgE production. This might depend on characteristics of the cat allergen: very persistent and particularly pro-inflammatory.
About pollens, specific IgE tends to diminish with ageing, but not be abolished. Probably, pollens could be able to stimulate the immune system to produce IgE with a stronger ability than mites. It seems that pollens might have a more intense antigenic activity than mites as suggested by some studies.18,19
These findings are consistent with previous reports that showed an age-dependent reduction of IgE production associated with lowering of allergic symptoms.18,19
This study had some limitations: it was retrospectively conducted on a selected patient population sample, there was no follow-up, and symptoms were not considered. In fact, a recent study performed in an un-selected population gave different results.27 In addition, this study did not consider possible confounding factors, such as smoking status, parasite infestation, environmental exposures, seasonal variations, and number of sensitising allergens. Therefore, there is need to conduct cohort studies and long-term follow up trials to confirm these preliminary findings.
In conclusion, allergen-specific IgE production to inhaled molecular components tends to reduce with ageing, but with differences between allergens. This phenomenon should be adequately evaluated when managing allergic patients.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Conflict of interestAll authors declare that have no conflict of interest concerning the present study.
We wish to thank Giorgio Parodi and Roberto Bologna (Analysis Laboratory, IRCCS Istituto Giannina Gaslini) for their skilful cooperation regarding lab data elaboration.