Alternaria is the most important fungal species belonging to the class Deuteromycetes which causes allergic respiratory diseases. The fungus pattern often shows a pronounced seasonal periodicity and with fluctuations related to meteorological conditions. In this study, we aimed to investigate the effect of outdoor Alternaria spore concentrations on monthly lung function tests, symptoms, and medication scores in children sensitised only to Alternaria. Additionally, we planned to determine the Alternaria spores of the outdoor environment in Adana, with special respect to their relationships with meteorological conditions and their seasonal changes.
MethodsTwenty-five patients with a clinical diagnosis of asthma and/or rhinitis sensitised only to Alternaria were enrolled in the prospective study. Meteorological data and outdoor samples of airborne fungi were obtained between November 2006 and October 2007.
ResultsThe outdoor Alternaria spore concentrations were significantly correlated with the monthly average temperature (r=0.626, p=0.03) and monthly average barometric pressure (r=−0.613, p=0.03). Similarly, the outdoor Alternaria spore concentrations were significantly correlated with mean monthly asthma medication score (r=0.599, p=0.04), value monthly PEF (r=−0.737, p=0.006), value monthly FEF25–75% (r=−0.914, p=0.0001) and, variation in PEF (r=0.901, p=0.0001).
ConclusionsThe atmospheric concentration of Alternaria spores are markedly affected by meteorological factors such as air temperatures and barometric pressures. In hypersensitive patients, Alternaria spores can induce decreases in respiratory functions and development of allergic symptoms between May and September, being especially more influential in August.
Biological materials are present in the atmosphere in the form of pollens, fungal spores, bacteria, viruses, and any fragments from plants and animals. Alternaria and Cladosporium spores are the most common airborne particles of fungal origin in outdoor air. Their threshold concentration in the air for evoking allergic symptoms has been estimated to be 100 and 3,000 spores/m3, respectively.1,2 People are always exposed to varying concentrations of these mould particles everywhere - home, school, workplace, or outdoors.3 Outdoor fungal spores are mainly present on decaying leaf materials, dung, straw, grass piles, plant stems and in damp areas and they are spread into the atmosphere during some activities performed by using grass-cutting machines, rakes and ploughs. Additionally, the airspora concentrations of outdoor environments depend on numerous factors, including: time of day, meteorological factors, seasonal climatic factors, and type of vegetation.4
Hypersensitivity to Alternaria is usually seen in combination with other allergens. In a very small percentage of patients isolated allergy to Alternaria spores can be detected.5 Although the relationship between asthma severity and exposure to airborne fungi has been well studied, little is known about the contribution of outdoor moulds to the symptoms of children monosensitised to moulds.6
In this study, we aimed to investigate the effect of outdoor mould spore concentrations on monthly lung function tests, symptoms, and medication scores in children with asthma and/or rhinitis sensitised only to Alternaria. Additionally, we planned to determine the Alternaria spores of the outdoor environment in Adana, with special respect to their relationships with meteorological conditions and their seasonal changes.
Material and methodsSubjectsTwenty-five patients with a clinical diagnosis of asthma and/or rhinitis sensitised only to Alternaria were enrolled in the prospective study. The study was performed between November 2006 and October 2007. Subjects who met the following inclusion criteria were admitted to the study:
- 1.
Living in central region of Adana for at least 2 years
- 2.
Subjects have a clinical diagnosis of asthma and/or rhinitis
- 3.
Subjects who are sensitised only to Alternaria
- 4.
Presence of sensitisation to other aeroallergens was considered as exclusion criteria.
Allergic rhinitis and asthma were diagnosed according to Allergic Rhinitis and its Impact on Asthma Workshop Report and Global Initiative for Asthma guidelines, respectively.7,8 A routine skin prick test was performed for all patients using kits containing prevalent inhalant allergens (Dermatophagoides pteronyssinus, Dermatophagoides farinae, grass mix, tree mix, mould mix, Alternaria species, Cladosporium species, eucalyptus, olive, and dander) (ALK-Abello’, Madrid, Spain) and a wheal with a diameter of ≥3mm was accepted as a positive reaction. None of the subjects had used oral corticosteroids or oral antihistamines for at least 10 days prior to the skin prick test (SPT). The SPT results were confirmed by in vitro IgE determination (UniCAP IgE, FEIA, Pharmacia, Uppsala, Sweden). Children were considered eligible for the study if sensitised to Alternaria, with a clinical history of rhinitis and/or asthma and never treated with specific immunotherapy before. Asthmatic patients were regularly given an antiinflammatory drug, budesonide (measured dose metered inhaler 200μg/dose) and a bronchodilator-salbutamol — (measured dose metered inhaler 100μg/dose) as required. Momentasone nasal spray as a nasal steroid and/or loratadine syrup or tablet were/was recommended for patients with rhinitis as required. All patients were informed in detail about the study protocol and volunteers were enrolled on the study. The study was approved by the Cukurova University Hospital's ethics committee.
Peak expiratory flow rate measurementsEach child was instructed in the use of the peak flow meter (Personal Best, Respironics Health Scan, USA) and practiced the manoeuvre under the supervision of a technician. Three peak expiratory flow rate (PEFR) measurements were made in a standing position on arising in the morning and again in the evening before bedtime. PEFR diaries were collected at approximately 4-week intervals. The mean variability in PEFR was then calculated for all children participating in each reporting period as the mean of the daily (amplitude as a percent of the mean, PEFR [difference between morning and evening values divided by the mean]).9 Ultimately, the daily mean variability of PEFR were converted to the monthly mean.
Lung function testingLung function was measured by maximum expiratory flow volume loops (ZAN 100 spiromed, Germany), recording the test with the highest forced vital capacity (FVC), forced expiratory volume in one second (FEV1), peak expiratory flow (PEF), forced expiratory flow between 25–75% of vital capacity (FEF 25–75%) and FEV1/FVC ration value as the best of three tests. Lung function testing was subsequently performed for all patients at approximately 4-week intervals.
Assessment of symptoms and medication scoresPatients were taught on their first day of treatment how to mark their symptoms into a standardised chart and which medication they had to take to counteract those symptoms. The severity of symptoms was assessed on a scale of 0–4 (0: no symptoms, 4: very severe symptoms) for five symptoms in rhinitis (itching nose, sneezing, blocked nose, nasal discharge and itching (eyes, throat, palate) and for four symptoms in asthma (cough, dyspnoea, wheezing and chest tightness)). These charts were provided for the patients or their parents and were subsequently brought to our clinic every month. These forms reported the nasal and bronchial symptoms, as well as the possible necessary medications, for every day. Upper respiratory tract infections were excluded from the scoring of rhinitis. We calculated each patient's average daily score after one year of the study. The final medication and symptom scores were calculated as the mean of the daily scores.10,11
Fungal spore countsThe outdoor samples of airborne fungi were collected by Burkard 7-day recording volumetric trap in Adana atmosphere. The device was placed on the roof of the town hall at a height of 15metres (m) above the ground and samples were collected from November 2006 to October 2007. The air was sucked at a flow rate of 10 litres per minute and spore grains impacted on to tapes coated with a thin film of vaseline-paraffin wax in toluene. The tape was then mounted with glycerine jelly,15 and 24 transverse travels were observed for a daily slide. Spores were identified visually with a light microscope at a magnification of 400× by an experienced aerobiologist. Fungal spore counts were expressed as fungal spores per m3 of air.
Meteorological dataAdana is situated at 37°00′N, 35°19′E South of Turkey at an altitude 27metres above sea level. Adana has a Mediterranean vegetation, a generally Mediterranean climate, and with a population of approximately 1,500,000. The city is located on east Mediterranean coast, at sea level, in a temperate climate and characteristically has mild winter and very humid summer months. Meteorological data were obtained from the bulletin of the meteorological station located in the city centre. The monthly variations in meteorological data were recorded. Monthly data for temperature (°C), rainfall (precipitation) (kg/m2), wind speed (m/sn), maximum wind speed (m/sn), barometric pressure (hpa), and relative humidity (%) for Adana were extracted from Meteorological Office databases (from November 2006 to October 2007).
Statistical analysis of dataAll the analyses were performed using computer software (SPSS version 12.0; SPSS; Chicago, Illinois, USA). Descriptive statistics were expressed as mean+SD, geometric mean, median and range. Pearson correlation test was used to test the relation between outdoor spore counts and meteorological data, symptom scores, lung function test, and variability in PEF.
ResultsWe studied 25 allergic patients; their median age was 10.5±2.15 (7.5–14.5) years. Among the 25 patients enrolled to the study, only 20 patients completed a great portion of the diaries. Demographic data of patients are shown in Table 1.
Demographic data and some characteristics of the patients
| Age | |
| Range in years | 7.5–14.5 |
| Mean ± SD | 10.5±2.15 |
| Sex n (%) | |
| Male | 15 (60%) |
| Female | 10 (40%) |
| Duration of the disease | |
| mean±SD (range in years) | 4.77± 2.70 (1.5–10) |
| Diagnosis | |
| asthma | 11 children |
| asthma+rhinitis | 14 children |
| Treatment protocol | |
| for asthma | Budesonide 200–400μg/day, Salbutamol inhaler (100μg/dose) as required |
| for rhinitis | Nasal steroid and/or oral antihistamines as required |
| Clinical and lung function data of the patients (mean±SD) | |
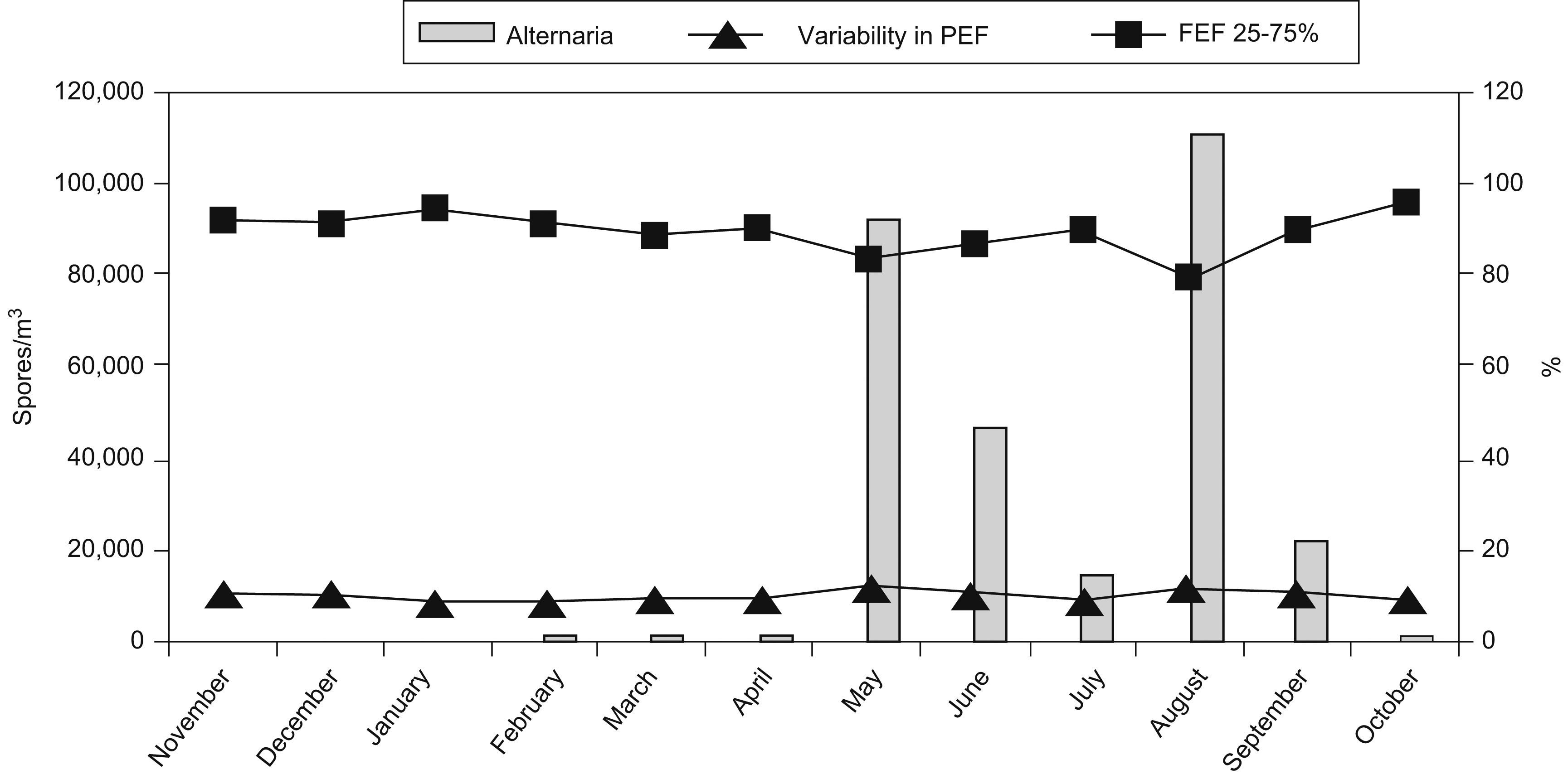
The outdoor Alternaria spore concentrations were significantly correlated with mean monthly asthma medication score (r=0.599, p=0.04). Mean monthly asthma medication scores were highest in May and August, while the lowest value of mean asthma scores were in March and April. Similarly, the outdoor Alternaria spore concentrations were significantly correlated with the value for monthly PEF (r=−0.737, p=0.006), value for monthly FEF25–75% (r=−0.914, p=0.0001), and variability in PEF (r=0.901, p=0.0001) (Figure 1, Table 2). Clinical and lung function data are shown in Table 3.
Analysis of Pearson's correlation
| Temperature (°C) | Rainfall (mm3) | Relative humidity (% RH) | Barometric pressure (hpa) | Mean wind speed (m/s) | Maximum wind speed (m/s) | |
| Alternaria spore concentrations | r= 0.626* (p=0.03) | r=−0.403 (p=0.2) | r=0.548 (p=0.06) | r=−0.613* (p=0.03) | r=0.102 (p=0.7) | r=0.517 (p=0.08) |
| Asthma medication score | FVC | FEV1 | PEF | FEF 25–75 | Variability in PEF | |
| Alternaria spore | r=0.599 (p=0.04) | r=−0.347 (p=0.2) | r=0.029 (p=0.9) | r=−0.737** (p=0.006) | r=−0.914** (p=0.0001) | r=0.901** (p=0.0001) |
The outdoor Alternaria concentrations were significantly correlated with the monthly average temperature (r=0.626, p<0.03), average barometric pressure (r=−0.613, p=0.03), monthly average PEF value (r=−0.737, p=0.006), monthly average FEF25–75 value (r=−0.914, p=0.0001), and monthly average variability in PEF value (r=0.901, p=0.0001).
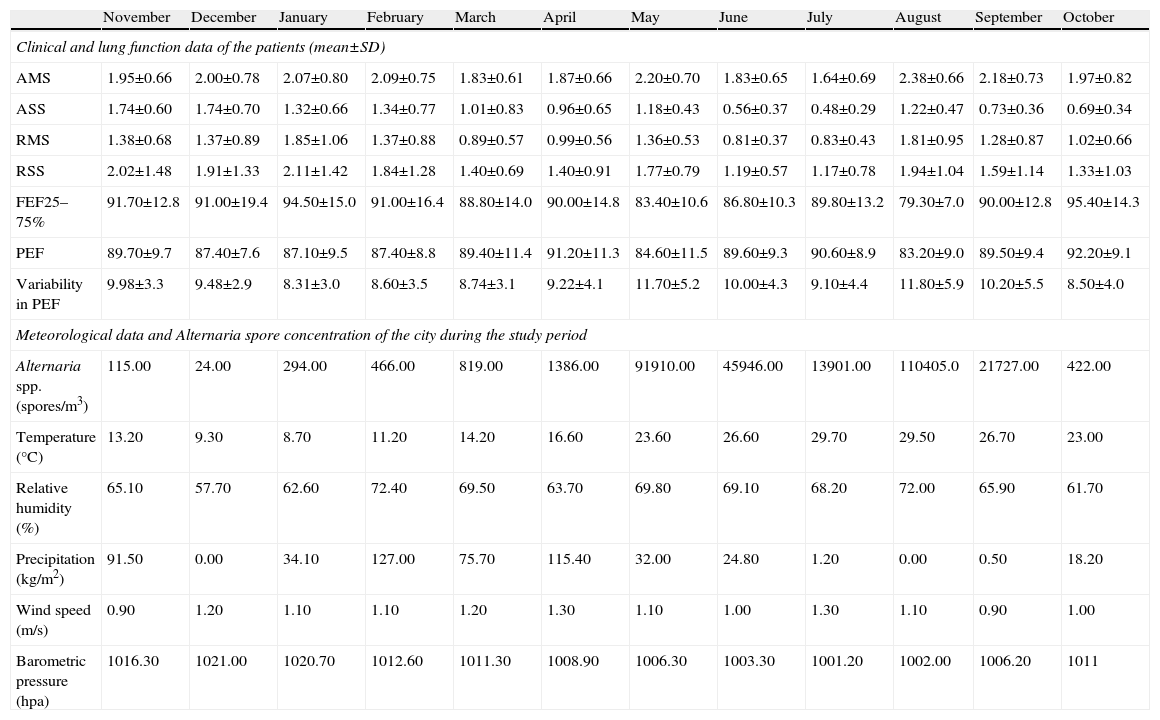
Lung function data of the patients and meteorological data, Alternaria spore concentration of the city
| November | December | January | February | March | April | May | June | July | August | September | October | |
| Clinical and lung function data of the patients (mean±SD) | ||||||||||||
| AMS | 1.95±0.66 | 2.00±0.78 | 2.07±0.80 | 2.09±0.75 | 1.83±0.61 | 1.87±0.66 | 2.20±0.70 | 1.83±0.65 | 1.64±0.69 | 2.38±0.66 | 2.18±0.73 | 1.97±0.82 |
| ASS | 1.74±0.60 | 1.74±0.70 | 1.32±0.66 | 1.34±0.77 | 1.01±0.83 | 0.96±0.65 | 1.18±0.43 | 0.56±0.37 | 0.48±0.29 | 1.22±0.47 | 0.73±0.36 | 0.69±0.34 |
| RMS | 1.38±0.68 | 1.37±0.89 | 1.85±1.06 | 1.37±0.88 | 0.89±0.57 | 0.99±0.56 | 1.36±0.53 | 0.81±0.37 | 0.83±0.43 | 1.81±0.95 | 1.28±0.87 | 1.02±0.66 |
| RSS | 2.02±1.48 | 1.91±1.33 | 2.11±1.42 | 1.84±1.28 | 1.40±0.69 | 1.40±0.91 | 1.77±0.79 | 1.19±0.57 | 1.17±0.78 | 1.94±1.04 | 1.59±1.14 | 1.33±1.03 |
| FEF25–75% | 91.70±12.8 | 91.00±19.4 | 94.50±15.0 | 91.00±16.4 | 88.80±14.0 | 90.00±14.8 | 83.40±10.6 | 86.80±10.3 | 89.80±13.2 | 79.30±7.0 | 90.00±12.8 | 95.40±14.3 |
| PEF | 89.70±9.7 | 87.40±7.6 | 87.10±9.5 | 87.40±8.8 | 89.40±11.4 | 91.20±11.3 | 84.60±11.5 | 89.60±9.3 | 90.60±8.9 | 83.20±9.0 | 89.50±9.4 | 92.20±9.1 |
| Variability in PEF | 9.98±3.3 | 9.48±2.9 | 8.31±3.0 | 8.60±3.5 | 8.74±3.1 | 9.22±4.1 | 11.70±5.2 | 10.00±4.3 | 9.10±4.4 | 11.80±5.9 | 10.20±5.5 | 8.50±4.0 |
| Meteorological data and Alternaria spore concentration of the city during the study period | ||||||||||||
| Alternaria spp. (spores/m3) | 115.00 | 24.00 | 294.00 | 466.00 | 819.00 | 1386.00 | 91910.00 | 45946.00 | 13901.00 | 110405.0 | 21727.00 | 422.00 |
| Temperature (°C) | 13.20 | 9.30 | 8.70 | 11.20 | 14.20 | 16.60 | 23.60 | 26.60 | 29.70 | 29.50 | 26.70 | 23.00 |
| Relative humidity (%) | 65.10 | 57.70 | 62.60 | 72.40 | 69.50 | 63.70 | 69.80 | 69.10 | 68.20 | 72.00 | 65.90 | 61.70 |
| Precipitation (kg/m2) | 91.50 | 0.00 | 34.10 | 127.00 | 75.70 | 115.40 | 32.00 | 24.80 | 1.20 | 0.00 | 0.50 | 18.20 |
| Wind speed (m/s) | 0.90 | 1.20 | 1.10 | 1.10 | 1.20 | 1.30 | 1.10 | 1.00 | 1.30 | 1.10 | 0.90 | 1.00 |
| Barometric pressure (hpa) | 1016.30 | 1021.00 | 1020.70 | 1012.60 | 1011.30 | 1008.90 | 1006.30 | 1003.30 | 1001.20 | 1002.00 | 1006.20 | 1011 |
Asthma medication scores (AMS), Asthma symptom scores (ASS), Rhinitis medication scores (RMS), Rhinitis symptom scores (RSS).
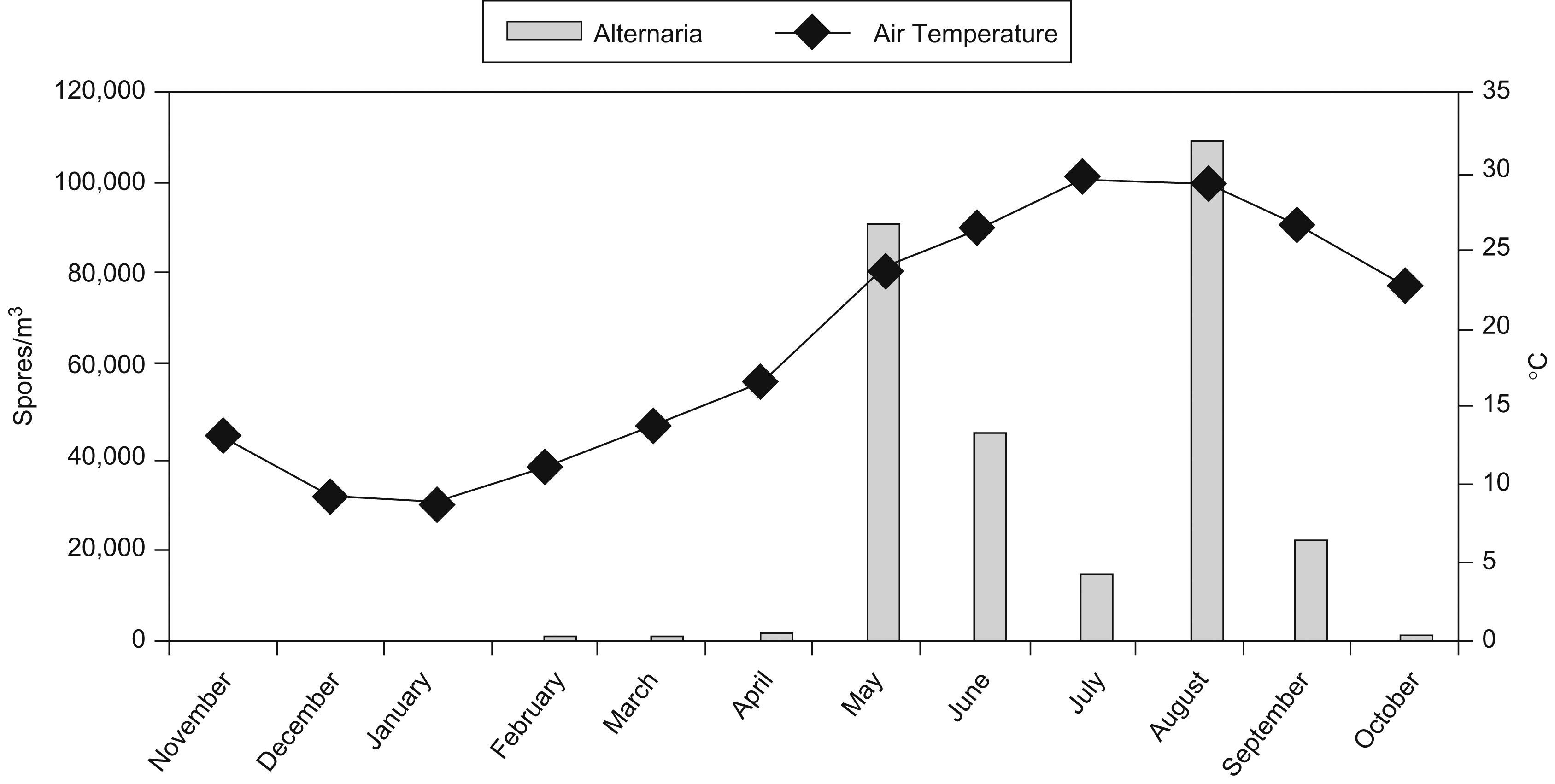
Alternaria spore concentrations were highest in May (91910spores/m3) and August (110405spores/m3), while the lowest value were detected in November (115spores/m3) and December (24spores/m3). The outdoor Alternaria spore concentrations were significantly correlated with the monthly average air temperature (r=0.626, p=0.03) (Figure 2), monthly average barometric pressure (r=−0.613, p=0.03) (Table 2). The air temperatures were highest in July (29.7°C) and August (29.5°C), while the lowest values were detected in December (9.3°C) and January (8.7°C). Additionally, the barometric pressure was highest in December (1021hpa) and January (1020.7hpa), while the lowest values were detected in July (1001.2hpa) and August (1002hpa). Summary of meteorological data and Alternaria spore count are given in Table 3.
DiscussionAlternaria is the most important fungal species belonging to the class Deuteromycetes which causes allergic respiratory diseases.2,12 Threshold concentrations for triggering allergic symptoms are estimated to be 100spores/m3 for Alternaria species.13 Its concentration in the air is 500–1000spor/m3.2 Fungus pattern often shows a pronounced seasonal periodicity and fluctuations related to meteorological conditions. Different authors have found a pattern variation in total or general fungal concentration which relates to meteorological conditions.14–16 In effect, increases in temperature, humidity, cumulative rainfall increments, and the hours of sunlight all positively influence the levels of spores detected in the air (particularly as refers to Alternaria).17
In our study a positive correlation was found between atmospheric concentration of Alternaria spores and air temperature, while a negative correlation was detected with barometric pressure. However we could not find any correlation between concentration of Alternaria spores and meteorological parameters such as humidity, rainfall, mean and maximum wind speed. Alternaria spores are isolated frequently during hot, dry and windy weather conditions towards the end of summer and in the beginning of autumn.2 In our study we also obtained similar results. We detected maximal concentration of Alternaria spores during August, and then secondly in May. Especially in May, a marked increase in the concentration of Alternaria spores was observed together with an increase in the atmospheric temperature. Similarly, in studies performed in Ankara18 (Turkey), Zagrep19 (Croatia) and Stockholm20 (Sweden) maximal atmospheric spore concentrations of Alternaria were detected in August. Although these studies were performed in different geographic locations and climates, maximal atmospheric spore concentrations were observed in August, which is the hottest month of the year. These results indicate that air temperature is the most influential meteorological parameter effecting atmospheric concentrations of Alternaria spores.
On the other hand, studies performed have also demonstrated that together with air temperature, meteorological factors such as humidity, wind speed, and amount of rainfall could affect atmospheric concentrations of Cladosporium and Alternaria spores. The relative humidity rate was found to affect atmospheric concentrations of Alternaria spores more prominently than those of Cladosporium.21 However in our study, we detected that meteorological parameters like humidity, rainfall, and wind speed are not statistically significant factors effecting atmospheric spore concentrations. Failure to detect any significant correlation between wind speed and concentration of Alternaria spores could be attributed to the characteristic geographic features of Adana where the study was performed and relatively lower impact of wind speed on the atmospheric conditions of this region. However, in the literature the association of increase in the incidence of acute asthmatic episodes and storms was first mentioned by Packe and Ayes in 1985.22 Since then asthmatic episodes related to storms have been reported in various parts of the world. The prevalent hypothesis is that the increase in relative humidity secondary to higher wind speeds triggers production and spread of spores. Storm asthma was correlated with a two-fold increase in the number of fungal spores in the air.12,23 On the contrary, previous studies carried out by Timmer et al.24 and Katial et al.25 found no significant relationship between Alternaria and meteorological factors.
During the time interval of the study, the predominant fungal spores in the atmosphere in our city were detected to be Cladosporium and Alternaria spores. These are known to be the most severe allergy-inducing fungal species.1,2 Some epidemiologic studies suggested that sensitisation to Alternaria is associated with asthma, particularly with severe asthma and life-threatening exacerbations.6,26 Huang et al.27 and Su et al.28 in their epidemiological studies indicated that fungal spores of ambient air are associated with many health effects, such as increased respiratory symptoms, decreased lung function, increased hospital emergency admissions and respiratory and cardiovascular mortality. As most time (70–90%) is spend indoors, information on the indoor and outdoor relationships of airborne fungal concentrations is important. The main source of airborne fungi in indoor air is usually outdoor air. Most patients with fungal allergy have perennial symptoms, though in our geographical setting the maximum concentration of Alternaria spores in the environment, and thus in theory the peak in symptoms among affected patients, corresponds to the summer and autumn months.29
In monthly pulmonary function tests performed, negative correlations between PEF and FEF25–75% with atmospheric concentrations of Alternaria spores were detected, while a positive correlation was found with respect to monthly variability in PEF. In contrast, any statistically significant correlation with FVC and FEV1 was absent. We thought that PEF and especially FEF 25–75% were relatively more sensitive than other lung function parameters to airway obstruction developed as a result of exposure to allergens and they could be implicated for these correlations. FEV1 values generally reflect air flow rates through large airways, and do not indicate obstruction of smaller airways during early stages of the asthma. However, FEF25–75% reflects air flow through intermediate and small airways, and decreases during the earliest stages of the obstructive respiratory diseases.30 The sizes of fungal spores vary greatly between 2–20mm in diameter. Especially particles less than 5mm in diameter, descend into lower respiratory airways and lead to allergic reactions and symptoms of an asthmatic episode.1,2 The variability in PEF values demonstrate the presence of a significant correlation with respiratory symptoms and airway hypersensitivity. Moreover, the magnitude of variability in PEF is directly correlated with the severity of asthmatic episodes.30 Similarly, in our study in May and August when atmospheric spore concentrations of Alternaria spp. were at their peak, variability in PEF were observably of higher amplitude relative to other months.
Evaluation of symptom and medication scores in patients with asthma and rhinitis is considered to be important for clinical parameters in the follow-up of these types of diseases. When our study population was evaluated as for monthly AMS, ASS, RMS vs RSS and concentration of Alternaria spores, only AMS demonstrated a statistically significant correlation. Environmental factors (viral and bacterial infections, cold weather, air pollution, smoke, living in the community and crowded places) which trigger symptoms of allergic diseases such as asthma and rhinitis become more influential in winter months rather than in the summer.31 As inclusion criteria we requested from our patients not to write down their symptoms and drug usages related to upper respiratory tract infections in their medical file cards. Since symptoms arising from exposure to allergens and upper respiratory tract infections are identical, we have thought that our patients might find it difficult to make this discrimination. Higher symptom and medication scores obtained during winter months when atmospheric concentrations of Alternaria spores are lower, supporting our point of view.
In conclusion, the atmospheric concentration of Alternaria spores is markedly effected by meteorological factors such as air temperatures and barometric pressures. In hypersensitive patients, Alternaria spores can induce decreased respiratory functions and development of allergic symptoms between May and September, being especially more influential in August. Therefore, sensitised people ought to keep themselves away from such activities, keep their doors and windows closed and use filtered air conditions during the risky months.