Not only is asthma one of the leading causes of hospitalisation in children under 15 years and one of the main reasons for primary care outpatient visits, it also accounts for 13 million lost days of school annually, which can affect children's learning, integration at school and overall academic achievements.
Material and methodsThis review article highlights the important role of the school in helping children and adolescents to control and manage their asthma through integrated and coordinated actions of health professionals, school staff, family, and the community.
ResultsWe recommended key elements for a multidisciplinary team asthma school programme that can be replicated and implemented especially in developing countries where children and adolescents are in a more disadvantaged environment.
ConclusionThis multidisciplinary asthma school intervention when demonstrated with efficacy can be applied in the context of the real world, where many children and families who need care the most currently do not receive it.
Allergic diseases are a public health concern due to their high prevalence and adverse impact on quality of life. Overall, allergic diseases account for a third of chronic diseases in children and was ranked sixth among the most common childhood diseases by the World Health Organisation (WHO). Today, one in five school-age children has an allergic disease.1
Among allergic diseases, asthma is one of the most common reasons for medical assistance when it comes to primary care, as more than five million school-age children have physician-diagnosed asthma.2,3 In addition to being a major cause of hospitalisation in children under 15 years of age, asthma also accounts for 13 million lost days of school annually.4 This level of school absenteeism can affect children's learning, integration at school and their overall academic achievements.5–7
Because children spend many hours at school, it is essential to have good knowledge of the environment that they are exposed to. This is especially important for children with asthma as it is suggested that the exposure to micro-particles in the classroom is high. To lower the concentration of allergens and irritants in the school indoor environment, it is necessary to ensure proper cleaning procedures of the classrooms and that ventilation is adequate. This will help make the school an extension of the family environment for children and an important part of the proper management and control of asthma.8,9
In this paper, we evaluated the role of schools in helping to control asthma in children and adolescents. We recommended key elements for a multidisciplinary team asthma school programme that can be replicated and implemented especially in developing countries where children and adolescents are in a more disadvantaged environment.
MethodFor a better recognition, monitoring and care of children with asthma in schools, we conducted this review. In selecting articles, the PubMed database was used having the last 20 years as the search period. They following search terms were used: asthma, asthma programmes, school. Among the studies found, review and consensus articles with a high level of evidence for clinical decisions related to paediatric asthma and its impact on school health were selected. The articles were screened and selected in a three-phase step process. In the first step we analysed the articles which fitted the key words. The second step was to thoroughly read each article that met the criteria and finally in the third step, the most relevant articles for this review's objectives were chosen and included in the reference lists of the article.
Professionals working at school and asthmaIn order to establish proper management of asthma in schools, it is necessary to have an integrated and coordinated action amongst health professionals, school personnel, family, and government officials who are in charge of the legal framework.7
A recent systematic review conducted by Jaramillo and Reznik suggested that professionals working in schools have insufficient knowledge about the negative impact of allergic diseases on children's lives and their families.10 Teachers interact with children on a daily basis and being the “front-liners” are considered by many to be health promoters. They should be in a position to identify early allergic conditions especially in those that can be a life threat. In order for teachers to fully share the responsibility in disseminating asthma knowledge and raising awareness of asthma and serious allergic reactions with local health teams,11–14 this should be included in their professional training.15
To carry out an interdisciplinary effort among school, family and the healthcare team, guided and trained teachers would need to recognise the child with asthma through a medical report. With adequate and up-to-date information, the teacher could support the child participating in school activities when symptoms are well controlled.16
Integrated actionFamilies and teachers: When parents of children with asthma do not have good knowledge of asthma or proper management of the disease, their children could be at a higher risk for asthma exacerbations. In this regard, the role of the family in establishing good control of their child's asthma at home and at school is important. Parents should inform the teachers about their child's disease and its severity. More importantly, they should provide the school with an asthma action plan that was written by the child's doctor with information on triggers of asthma exacerbations and specific medications (with dose) to take in an emergency situation.8–17
The healthcare team: The healthcare team should maintain an effective and active communication with the family and school, confirm the diagnosis of asthma in the child, its severity, educate the patient and family, and establish an individual asthma action plan for each child with asthma if he or she does not have one. The healthcare team will help educate and raise the awareness of asthma amongst the families and teachers. With this strengthened “doctor–nurse–patient–family–school” relationship, the adverse impact of asthma in children's school activities may be reduced.18
It should be noted that the care of children with asthma is not limited to the responsibility of the child's family or restricted to the home environment. The “doctor–nurse–patient–family–school” team will ensure that the asthma is properly recognised and diagnosed, adequately treated and well controlled. The ultimate goal is to minimise school absenteeism and to improve quality of life.
Initiatives – asthma-friendly schoolThere are several successful initiatives of “asthma-friendly schools” implemented by various groups and in different countries. Examples include: Australia,19 the American Lung Association,20 Maryland,21 and the Centres for Disease Control and Prevention (CDC) (Asthma – Friendly schools Initiative).22 In Brazil, the Children's Asthma Prevention Programme (Programa Infantil de Prevenção de Asma – PIPA)23 uses a manual to teach how to manage the asthma programme in the school environment.24 The University of Bahia team demonstrated that at school and through a clear, simple and playful way, nurses can effectively stimulate the interest in children and adolescents and raise their awareness of asthma and the respiratory system.25
Implementation of asthma programme at the schoolTo implement an asthma care programme at school effectively, one must clearly define goals for success. Examples are outlined below:
- •
Decrease the frequency of acute asthma exacerbations in the place where the programme is implemented.
- •
Reduce the economic impact of childhood asthma.
- •
Decrease the frequency of under-diagnosed or poorly controlled asthma
- •
Reduce school absenteeism.
- •
Improve the knowledge of the disease in children with asthma.
- •
Improve communication among families, schools and health care providers to reduce health disparities in the management of childhood asthma.
- •
Improve the quality of life of children with asthma and their families.
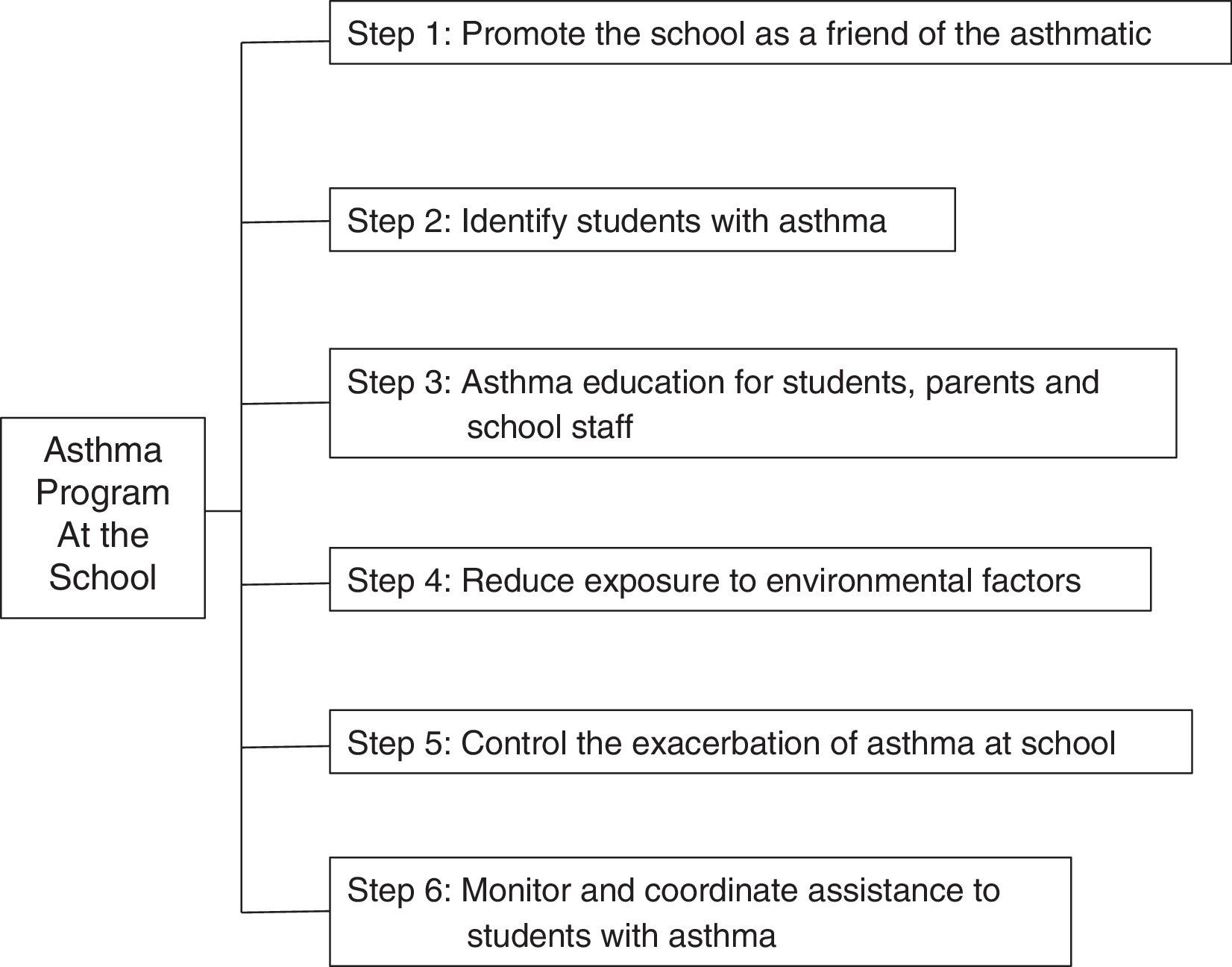
To achieve the above goals, we recommend to observe public policies for implementing asthma programmes at school, including: Asthma–Friendly Schools Initiative,22 American Lung Association20 and consensus such as the Global Initiative for Asthma (GINA).26 We recommend the successive steps below (Fig. 1) to achieve full implementation:
- •
Select the people who will work on the project as collaborators within the school community
- •
Base policies on management guides20,22,26
- •
Encourage children and their parents to notify the school that their children have asthma
- •
Encourage the school to recognise and identify students with asthma
- •
Evaluate, through written questionnaires, the knowledge of parents and teachers about asthma
- •
Promote the individual education of patients and their families about asthma, focusing on triggering factors, medication, use of Peak Expiratory Flow (PEF) and asthma action plan
- •
Promote asthma education at school and in the community
- •
Highlight the importance of every student with asthma having their own Written Asthma Action Plan, updated and filed with the school
- •
Establish procedures for the administration of medication at school28
- •
Emphasise the need for immediate access to short-acting beta2 agonists for administration to students having asthma attacks
- •
Document the suitability for use of the patient's own bronchodilator, if so required
- •
Drug administration can be performed by the nurse, if the school has one, or other trained and/or designated employees
- •
Encourage parents to notify the school when their children have episodes of asthma at school or at home
- •
Authorise in writing, i.e. sending and receiving school information to parents
- •
Develop a system for receiving information from the school nurse or school personnel responsible for monitoring the student with asthma
- •
Monitor and coordinate the students, especially those with difficult to control asthma
As outlined earlier, it is crucial for the healthcare team to maintain effective and active communication with the families and the school. The healthcare team is responsible for making an accurate and timely diagnosis of asthma, identifying its severity, educating the child and his or her family, and establishing an individual asthma action plan for each child with asthma, if he or she does not already have one. Thus, the healthcare team will have the opportunity to contribute to educating the children and families about asthma, raising the awareness of asthma, and promoting the doctor–nurse–multidisciplinary team–patient–family–school relationship. When successfully implemented, the asthma programme at school would be as successful as the integrated care pathways for airway diseases (AIRWAYS-ICPs)29 in reducing the impact of asthma in children.8
To enable an asthma programme to be implemented optimally at school, several professionals who have direct contact with children must be involved and they include: paediatricians,23 primary care physician,30 school nurse,31 physiotherapist,32 gym teacher,33 pharmacist,34 music teacher,35 the dance teacher,36 psychologist, and arts teacher,37 and even the school's janitorial staff. This new integrated approach to tackle respiratory problems has an important role in improving the health of patients with chronic respiratory diseases. In addition, by using drawing as a playful activity for children, the real feelings of the child with asthma can be revealed regarding his or her disease, treatment, limitations of daily living, as well as his or her feelings about the multidisciplinary team that works with him or her. Findings can be used to individualise the approach to meet each child's specific needs.
Future perspectivesThe Asthma Programme at School is designed to support/enhance asthma management,16 improve school performance in children with asthma and thereby reduce the global burden of asthma.
The school environment is a place where an asthma attack can occur such that appropriate and immediate intervention of teachers and school staff is paramount to prevent an adverse outcome from happening to the child.6 This can be achieved through establishing joint and complementary actions of the child, family, teachers, healthcare staff, community and relevant authorities. This is in keeping with the commitment to the rights of children.17
We understand and recognise that there are barriers to the implementation of asthma programmes at schools. For example, despite there being great experiences, such as the Denver Public Schools (Building Bridges)38 which relied on external sources of funding, faced the challenge to sustain. Limited funding renders even demonstrated successful programmes unsustainable. This may lead to suboptimal and a heterogeneous level of services and care that were provided to students with asthma39. Moreover, even for simple interventions that were externally funded may often have to compete with the many demands that schools face due to frequent restructuring of personnel and shifts of priorities, etc.39
Thus, to combat these challenges and to give the care of asthma in schools a priority, public policies may be the most effective and efficient avenue. Changing public policies to improve the management of asthma and other chronic diseases is not a new concept. The International Conference on Primary Health Care, in Alma-Ata in 1978, expressed the need for urgent action from all governments, healthcare teams and communities to promote the health of all peoples of the world, declaring health a fundamental human right, reducing inequalities in health status, particularly between developed and developing countries, thereby being the duty of all to individually and collectively participate in the planning and implementation of health care.40 This declaration also considers that primary health care requires community participation in the planning, organisation and control, making full use of available resources, both local and national, and that governments must develop national policies, strategies and action plans to support primary health care in coordination with other sectors.40
World leaders are interested in expanding public policies related to the school-based asthma care programme, such as those generated by the American Lung Association (ALA)20 the Allergy and Asthma Foundation of America (AAFA),41 the Centres for Disease Control and Prevention (CDC),22 and the Global Alliance against Chronic Respiratory Diseases (GARD/WHO),42 which identified ways of how schools can and should engage and encourage community support, take advantage of the school's appropriate health services, identify the types of education that students and employees need, and ensure physical activity and safe and pleasant quality of life for students with asthma. However, these policy recommendations will not solve the problem of unequal access to asthma services in schools because they are not always adapted or applied equally in all countries. Public policy interventions with all levels of government involved present a real opportunity to address these inequalities. Only changes in policies at the federal, state and municipal levels in schools can improve a number of problems such as inadequate access to medication for both preventive and rescue asthma, the need for an asthma written action plan for the student with asthma in school, training for school professionals for the best care of children with asthma, improvement of awareness and knowledge about asthma among parents, school staff and students, and improvement of the school's indoor and outdoor air quality.6,17,39
Changes in health policies to solve these problems can take time and will require coordinated efforts among experts in asthma and support from children and families. They will have to become more active participants in the political process of the schools, thus enhancing their credibility and access to information on how to improve the results of asthma in children where programmes are implemented, and demonstrating that interventions of asthma management are proven to be effective and can be applied in the context of the real world, where many children and families who need care the most do not receive it.39
Ethical disclosuresConfidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Conflict of interestThe authors have no conflict of interest to declare.