Abbreviations
CVCoefficient of variation.
FEFForced expiratory flow.
FEF 50Forced expiratory flow at 50 % of expired volume.
FEF 75Forced expiratory flow at 75 % of expired volume.
FEF 25-75Forced expiratory flow between 25 and 75 % of expired volume.
FEVtTimed forced expiratory volume.
FEV 0.5Forced expiratory volume in the initial 0.5s.
FVCForced vital capacity.
RVResidual volume.
RVRTC Raised volume rapid thoracic compression.
TLCTotal lung capacity.
VmaxFRCForced expiratory flow at functional residual capacity.
V30Lung volume reached with a driving airway pressure of 30 cm H2O.
INTRODUCTION
Pulmonary function testing in infants has demonstrated to be useful to better understand physiological changes related to lung disease and lung growth in infancy. Recently, the method of raised volume which allows to measure forced expiratory flows over a significantly extended volume range (close to total lung capacity), has been reported to be a promissory advance over its predecessor the partial flow volume curve1-5. In partial flow volume curves forced flow measured at functional residual capacity (VmaxFRC) is obtained by initiating a rapid thoracic-abdominal compression at the end of inspiration during tidal breathing. In the raised volume rapid thoracic-abdominal compression (RVRTC) technique lungs are inflated to a pressure of 30 cm H2O (which is called V30 and would approximates to total lung capacity) and forced expiratory maneuvers are proceeded to residual volume (RV). This new method for measuring pulmonary function in infants and young children should approximate the voluntary maneuvers done by older children and adults in spirometry.
One of the more important characteristic of a new technique is to prove to be reproducible enough as to warrant reliable comparison either for intra-subject measurements as for inter-subject evolution of their pulmonary function, in health and disease. There is a limited number of publications describing the variability of the RVRTC technique, either in normal infants as in those with lower respiratory disease2,5-8 and figures are similar to what reported using maximal expiratory maneuvers in older children and adults9-11. The reported intra-subject variability for the different forced flow parameters obtained by means of RVRTC varies according to different laboratories, but are in general low with FEVt ranging from 3,7 to 7,6 % and FEF from 5,2 to 10,9 %2,5-8 and the mean intra-subject variability of RVRTC is notoriously lower than for VmaxFRC which would range between 9-17 %2,6,8,12-17.
In older children and adults the most useful characteristic of spirometric determination is its low variability what makes this test one of the most valuables tools for studying lung function under therapeutic interventions or physiological research.
Despite of the increasing number of publications with the RVRTC, there is a limited number of studies describing their within-subject variability and seldom mentioning the method employed for its assessment. These studies vary on the number of infants involved (generally low), their clinical condition and the modality of the technique to get raised lung volume and with only 2 of them that have studied infants suffering from recurrent wheezing2,8. In these infants, the variability of the technique to assess lung function is critical to properly interpreting the changes occurred after administering inhaled broncho-active agents as bronchodilators or steroids.
This study was done to determine the intra-subject variability of spirometric-like parameters obtained with the technique of RVRTC in infants with recurrent wheezing.
METHODS
Subjects
One hundred and fifteen infants with recurrent wheezing defined as 3 or more episodes in the last 12 months or in their life if aged less than one year, who were recruited from our outpatient clinic, participated in this study. The group had a mean age of 62 weeks (range 16.7 to 110.4); a mean length of 75.7 cm (range 63 to 91.5) and a mean weight of 10.2 kg (range 6.3 to 15.3). Infants with low birth weight, chronic neonatal respiratory disease and with others known metabolic, gastrointestinal or cardiac diseases were excluded from the study.
They were all measured while asymptomatic and free of respiratory infections for at least 3 weeks. All of them were in treatment with bronchodilators on an as-needed basis, which were withheld for 12 hours prior to lung function testing; inhaled anti-inflammatory medications were maintained.
Equipment: A pneumotachometer (Hans Rudolph 3700) and a differential pressure transducer (Validyne MP45-871, ± 2 cm H20, USA.) were used to measure flow. Differential pressure transducers were also used to measure airway opening pressure (Validyne MP 45-871, ± 50 cm H2O) and jacket pressure (Validyne MP 45-871, ± 100 cm H2O). The analog signals of flow and pressure were amplified and filtered above 50 Hz (Validyne CD 19-A) and digitized at 100 samples per second. Volume was obtained by digital integration of the flow signal.
The squeezejacket consisted of a rapidly inflatable and expandable inner layer within a rigid outer layer, which was wrapped around the infant's chest and abdomen, with the arms kept out of jacket. An electronic solenoid valve between the jacket and a 50L pressure reservoir controlled jacket inflation.
Calibration for zero flow, jacket and mouth pressure at the amplifier, as well as for pressure (water manometer) and flow-volume (300 ml calibration syringe, Hans Rudolf), were made every day and when necessary, between measurements.
RVRTC Technique: Forced expiratory maneuvers from elevated lung volumes were performed using multiple inflations and the rapid thoracic compression technique, as described by Feher et al18, according to the last ATS/ERS workshop specifications4 for this technique. Oxygen saturation, heart rate, and respiratory rate were continuously monitored during the test. Parents were invited to be present during testing.
The lung function maneuvers were performed while infants were sleeping, sedated with oral chloral hydrate (60-90 mg/kg), in the supine position with their necks slightly extended. They breathed spontaneously through a face mask that covered their nose and mouth. The inspiratory circuit has an adjustable continuous flow of fresh air (15 to 20 L/min) and a built-in pressure relief valve set at 30 cm H2O. A pressure of 30 cm H2O was applied to the airway by a software-controlled valve several times prior to the forced expiratory maneuver, until a pause at the end of a passive expiration was detected (Hering-Breuer reflex). As soon as the pause was noted, the lung was inflated to the volume achieved by applying an airway pressure of 30 cm H20 (V30) and then forced expiration was produced by rapidly pressurizing the inflatable jacket, which was proceeded until expiratory flow ceased at a lung volume that was defined as RV. Immediately after that, the compressive pressure was released and spontaneous breathing re-assumed within a few seconds. The volume between V30 and RV was defined as forced vital capacity (FVC). The maneuvers were repeated with increasing jacket pressure until the curve with the highest volume and flow was obtained (no further increase in forced flows despite increasing jacket pressure) then 3 to 5 technically acceptable curves were obtained and the intra-subject variability for CVF, FEV0.5, FEF 50 %, FEF 75 % and FEF25-75 % was calculated. Predicted values employed were those from Jones et al19. The same operators performed all tests.
Statistical Analysis
The intra-subject coefficient of variation (CV) was calculated as a percentage of standard deviation divided by mean for each patient and expressed as mean group CV (%) and confidence interval at 95 %. The relationship of intra-subject CVs to subject lengths and ages was analyzed using correlation tests. A p value less than 0.05 was accepted as statistically significant.
The study was approved by the Ethics Committee of the Hospital CRS El Pino and written full informed consent was obtained from all parents.
RESULTS
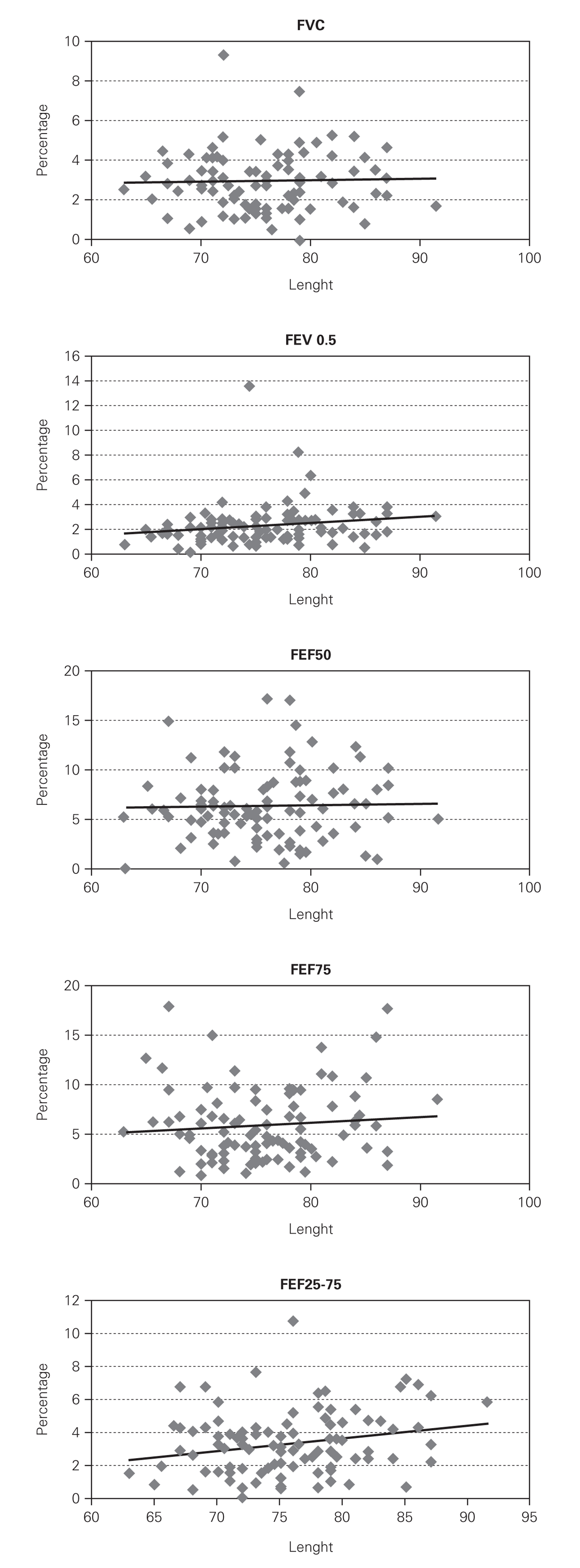
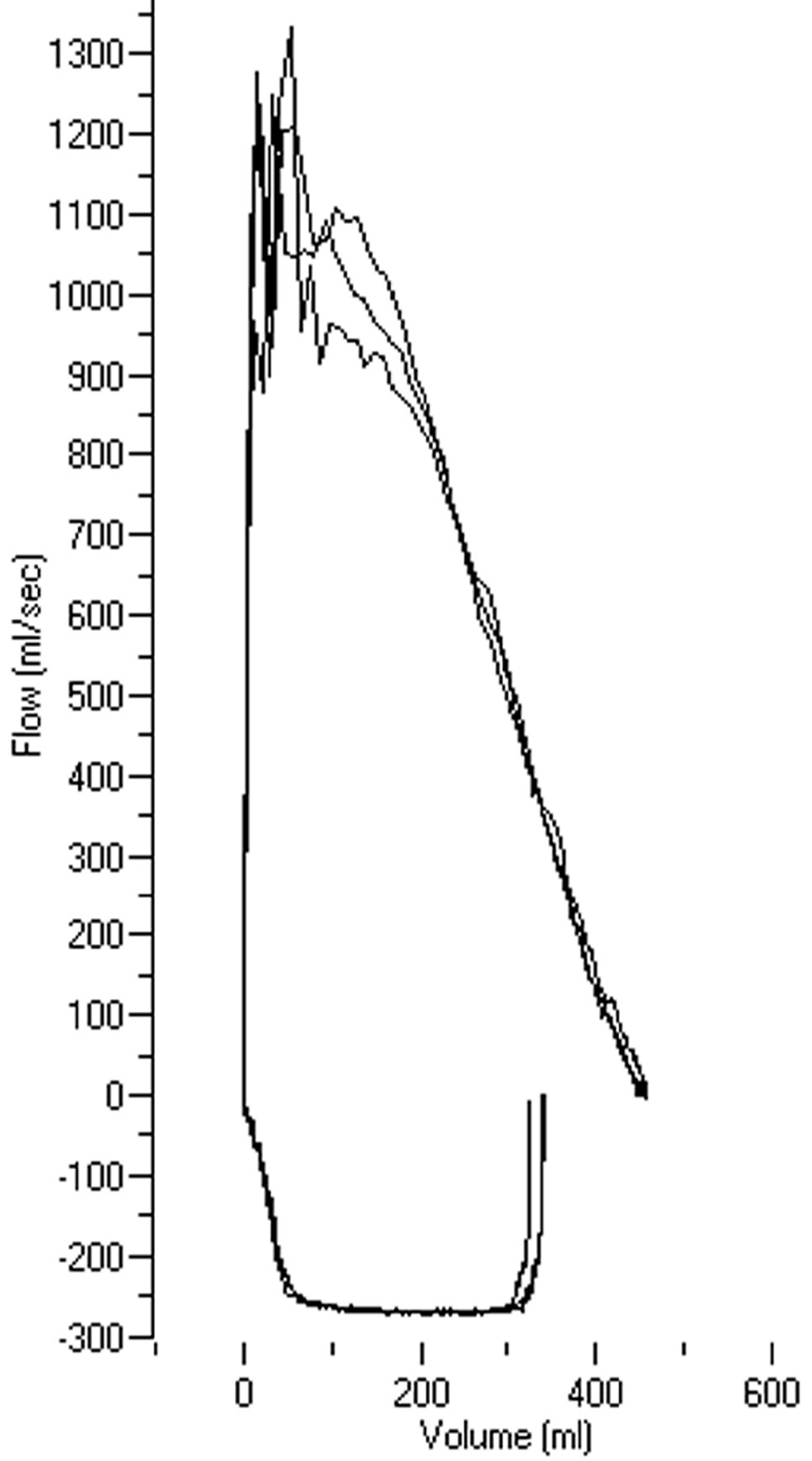
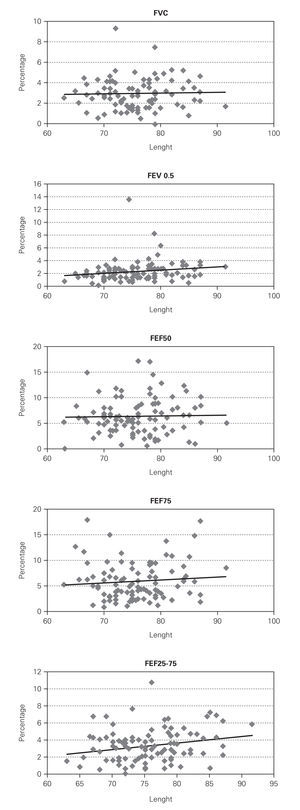
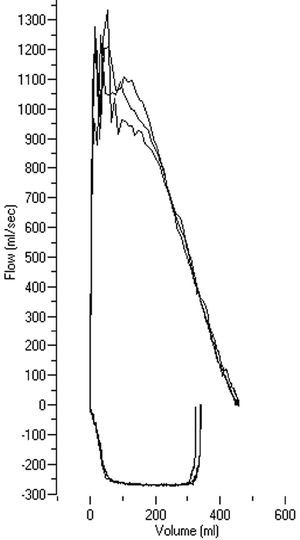
Of the 115 infants with recurrent wheezing initially recruited for the study, 13 infants woke up during the measurements, and were excluded from the study. Thus, 102 infants (73 boys and 29 girls) completed the study. Individual CVs for FVC, FEV 0.5 and FEF50, FEF75 and FEF 25-75 are plotted on figure 1. The mean group intra-subject CV for each spirometric parameter (CI 95 %) was as follows: FVC = 2.9 % (2.6-3.2); FEV0.5 = 2.2 % (1.9-2.5); FEF50 = 3.7 % (3.3-4.1); FEF75 = 5.9 % (5.2-6.6) and FEF25-75 = 3.3 % (2.9-3.7). The high reproducibility of measurements done with the RVRTC technique in a similar range of jacket pressure, can be seen in figure 2 where three consecutive flow-volume from the same patient have been displayed. It is worth to note they are very similar in shape and values of measured parameters.
Figure 1.--Individual coefficient of variation (CVs) for FVC, FEV0.5, FEF50, FEF75 and FEF 25-75 in 102 infants with recurrent wheezing while asymptomatic.
Figure 2.--Three consecutive flow-volume curves obtained with the RVRTC technique in the same patient at the flow-limitation jacket pressure range as can be seen on the monitor screen during lung function testing.
The lower variability was found to occur for FVC, FEV 0.5 and FEF 25-75 whereas FEF 75 had the highest variability. Intra-subject CV showed a slight increase with age and length for all parameters, but it was significant only for FEF 25-75.
No complications secondary to the test or sedation occurred in the infants who participated in this study.
DISCUSSION
This study demonstrated that in infants with recurrent wheezing, the RVRTC technique employed to generated forced expiratory flows from elevated lung volumes has low variability of timed volume and forced flow parameters as reported for older children and adults.
We only found 5 studies with RVRTC technique where the variability is described2,5-8. They have marked differences according to the number of infants involved, the modality of the technique employed, the presence or not of respiratory disease and the parameters analyzed; those studies are resumed on table I.
We found very similar CV in asymptomatic recurrent wheezing infants than those reported by Castile et al5 for normal infants. The latter may be explained because our study and Castile's used the same technique inflating the lungs several times to V30 until a respiratory pause was evoked to achieve measurements without the influence of respiratory muscles and that certainly contributes to standardize the technique and probably results in more reproducible measurements. To facilitate comparisons between different laboratories using RVRTC, it would be highly recommendable to have a more standardized technique, as suggested by a recent ATS/ERS workshop4; we also recommend that studies using RVRTC, or other techniques to measure lung function in infants, should also provide complete information on the intra-subject variability of their measurements.
The variability of RVRTC whatever be the procedure or technique employed has been reported to be lower than 6 %, which is much better than what reported in the past for other forced expiratory flow techniques, as VmaxFRC2,6,8,12-17.
The present study found that the more reproducible parameters were FEV 0.5 and FEF 25-75 suggesting that they may be better to compare airways response to broncho-active agents, lung growth and development in infants with recurrent wheezing than FEF50 and FEF75 even when the variability of these parameters was also found to be low.
For most of parameters there was no significant correlation between CV and height, suggesting that this technique measures infants lung function in this length range (60-90 cm) with similar and high reproducibility. In older children the variability of spirometric parameters seems to decrease with age and length8, reflecting the effect on test variability determined by the ability to collaborate and correctly execute the forced vital capacity maneuver. The latter is not expected to occur for RVRTC technique because the infant is sedated and both, lung inflation and chest compression pressures, are standardized and always performed with a relaxed respiratory system. Thus, for spirometric-like parameters in infants, the variability is likely to depend, among others, on the degree of sedation, the position of mask, supporting cheeks and soft part of the neck and the intensity of the Hering-Breuer inflation reflex to generate the relaxation of respiratory muscles.
In 259 normal children, aged 3 to 6 years, it was recently reported that the group mean coefficients of variation for replicated measurements of FVC, FEV 1, and FEF 25-75 were 2.5 %, 2.7 %, and 8.3 %, respectively9. In our infants we found similar variability for FVC (2.9 %) and FEV 0.5 (2.2 %) with a lower variability for FEF 25-75 (3.3 %).
The low variability of RVRTC reported here would allow for comparisons of forced flows from raised lung volume in infancy with those obtained in older children giving the possibility to track lung function in health and disease with similar and reproducible lung function tests. This would provide important lacking information on physiological progress and age-dependent changes of pulmonary function in this critical early stage of life.
Conclusion: The results of the present study demonstrate that the intra-subject variability of spirometric parameters as those obtained by the RVRTC is consistently low. Our findings are related to a group of infants with moderate episodes of recurrent wheezing, which is by far the group of infants that receives more therapeutic interventions, usually with inhaled bronchodilators and corticosteroids. In this group of infants, when objectively assessing the response to different broncho-active agents it would be desirable to employ a technique exhibiting a very low variability in order to detect true changes determined by such interventions. This study, performed in 102 recurrent wheezing infants, contributes to support the high reproducibility of measurements from spirometry-like infant lung function testing (RVRTC) at this early age.