Beta-lactam antibiotics are the most frequent cause of antibiotic hypersensitivity reactions. The study of all cases of suspected beta-lactam hypersensitivity is highly important, to avoid the use of less efficient or more expensive alternatives, for fear of a reaction.
Materials and methodsSixty-seven consecutive patients with suspected beta-lactam hypersensitivity reactions were studied. Skin prick tests (SPT), intradermal tests (IDT) and specific IgE determination were performed. In non-immediate reactions, epicutaneous testing was also done. If all were negative, a drug challenge was performed.
ResultsSixty-seven patients (54 ♀), with a mean age±SD of 36.6±19.3 years (4–78 years) were studied. The self-reported antibiotics were amoxicillin and amoxicillin/clavulanic acid in 30 (45%), penicillin in 24 (36%), cephalosporins in 11 (16%) and flucloxacillin in 2 (3%). SPT and IDT were positive in 6 patients (9%) and specific IgE in 11 (16%). Only one patient had both positive specific IgE and skin tests. Of the remaining 51 cases, 33 underwent a drug challenge with the culprit antibiotic, with a positive reaction in 2 (6%). In all positive cases and when a drug challenge with the suspected antibiotic was not indicated, a challenge with an alternative drug was done, all with negative results.
ConclusionsOf the 67 studied cases with history of beta-lactam hypersensitivity reactions, 18 (27%) were confirmed after testing. A combination of skin testing, specific IgE determination and drug challenge is necessary since none has sufficient sensitivity to be used alone.
Beta-lactam antibiotics, such as penicillin, amoxicillin and cephalosporins are the most commonly used antibiotics, accounting for two thirds of those available on the market.1 They are also the most frequent cause of antibiotic hypersensitivity reactions. According to a recent study, adverse drug reactions affect 10–20% of hospitalised patients and more than 7% of the general population,2 and may be immediate or take several days to present. The most frequent clinical presentations are maculopapular or urticarial rashes and angio-oedema, but severe reactions such as anaphylaxis can also occur. The avoidance of beta-lactams based only on the clinical history, to prevent a theoretical hypersensitivity reaction, result in the use of less efficient or more expensive alternatives. This can lead to high socioeconomic costs, possible treatment failure, increased toxicity of the alternative antibiotic, as well as an increase in drug resistant bacteria strains.3,4 For these reasons, the study of all suspected cases of beta-lactam hypersensitivity reactions is highly important and cost-effective.
A consistent diagnosis should always be based on a combination of: 1) skin tests (prick, intradermal and epicutaneous); 2) specific IgE determination; 3) drug challenge, when the previous two are both negative and the reaction is not life-threatening.5,6 The sensitivity of skin tests for diagnosing beta-lactam hypersensitivity reactions seem to be approximately 70%, with a specificity of 97%.7 As for specific IgE, a recent study showed that the specificity determined by fluoroenzymeimmunoassay (FEIA CAP-System®, Phadia, Uppsala, Sweden) ranged from 83.3% to 100% and sensitivity from 0% to 25%.8 It should be noted, however, that skin tests do not replace specific IgE determination. It has been shown that up to 14% of patients with immediate allergic reaction to beta-lactams can be specific IgE-positive but have negative skin tests.9 In another study, determination of specific IgE to penicillin or amoxicillin was positive in 42% of patients with negative skin tests and positive drug provocation challenge to the culprit beta-lactam.10 Additionally, as shown by Torres et al.11, in patients with a clear positive history of immediate allergic reaction to penicillins, a significant proportion can have both negative skin tests and negative specific IgE determination, but positive drug challenge.
AimTo evaluate the need for a combined strategy for the study of patients with history of beta-lactam hypersensitivity reactions, and its results.
Materials and methodsThe authors included in this evaluation a group of 67 consecutive patients who were referred to our Drug Allergy Division with a history of beta-lactam hypersensitivity reactions, between January 2005 and July 2007.
After completing the standardised European Network for Drug Allergy (ENDA) questionnaire12 and signing the informed consent form, patients underwent skin tests, in vitro tests for specific IgE determination and drug challenge.
Skin prick tests (SPT) were carried out first and, if negative, intradermal tests (IDT) were also performed. In all patients, testing was performed using major (PPL) and minor determinants (MDM) of penicillin, penicillin G, amoxicillin, ampicillin and other beta-lactams besides the previously mentioned, according to clinical history.13 The maximum concentrations used for both prick and intradermal tests were: PPL 5×10−5mmol/L, MDM 2×10−2mmol/L, amoxicillin 20–25mg/mL, ampicillin 20–25mg/mL and for most cephalosporins 1–2mg/mL5. The SPT were performed using the antibiotic with the referred maximal concentration and the IDT were performed using 1/100, 1/10 and 1/1 concentrations. Reactions with a wheal at least 3mm in diameter with a negative response to the negative control for SPT and a 3mm increase in the diameter of the initial wheal associated with a flare for IDT were considered positive.5,13 Evaluation was assessed after 20min and again after 24–48h, should any delayed reaction occurred. Both immediate and non-immediate skin reactions were recorded.
In non-immediate hypersensitivity reactions, epicutaneous testing was also done, using the same antibiotics.14,15
Total and specific IgE to penicillin G and V, ampicillin and amoxicillin were also determined using CAP-System® (Phadia, Uppsala, Sweden). Cut-off was considered to be 0.35kU/L, with values above or equal to 0.35kU/L considered positive and those below 0.35kU/L considered negative.
When skin tests and specific IgE were both negative, drug challenge with the suspected beta-lactam was performed according to ENDA guidelines,6 under strict medical surveillance. Increasing doses of the suspected drug were administered each 30min until the therapeutic dose was achieved. The symptoms and signs were monitored during the challenge, as well as pulse, blood pressure and PEF measurements if bronchospasm was referred in the clinical history. Drug challenge was considered positive if symptoms and/or signs suggestive of hypersensitivity or an anaphylaxis occurred.
As this is a descriptive study, qualitative variables such as sex, drug, symptoms, as well as results of provocation tests are described in frequency and percentage. Quantitative variables, such as age, are expressed with means and standard deviations.
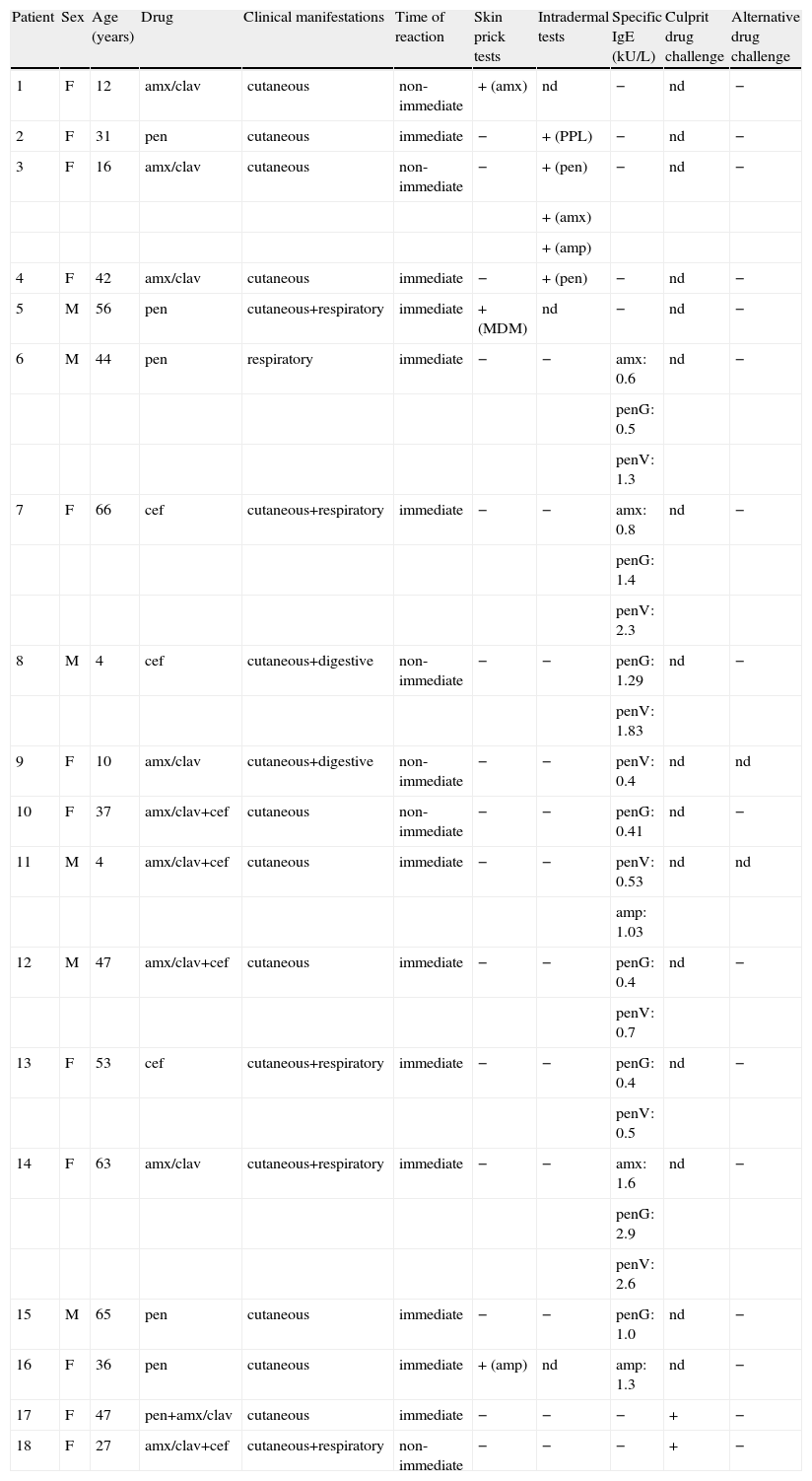
ResultsA total of 67 patients (54 ♀, 13 ♂), with a mean age±SD of 36.6±19.3 years (4–78 years) with a history of suspected beta-lactam hypersensitivity were studied. The most frequent self-reported antibiotics were amoxicillin and amoxicillin/clavulanic acid in 30 cases (45%), penicillin in 24 (36%), cephalosporins in 11 (16%) and flucloxacillin in 2 (3%). The clinical presentations were cutaneous in 43 patients (64%), respiratory in 3 (4%), gastrointestinal in 2 (3%), cutaneous+respiratory in 8 (12%), cutaneous+gastrointestinal in 7 (10%) and others in 4 (6%) (Table 1).
Patients with positive skin tests, specific IgE or drug challenges
| Patient | Sex | Age (years) | Drug | Clinical manifestations | Time of reaction | Skin prick tests | Intradermal tests | Specific IgE (kU/L) | Culprit drug challenge | Alternative drug challenge |
| 1 | F | 12 | amx/clav | cutaneous | non-immediate | + (amx) | nd | − | nd | − |
| 2 | F | 31 | pen | cutaneous | immediate | − | + (PPL) | − | nd | − |
| 3 | F | 16 | amx/clav | cutaneous | non-immediate | − | + (pen) | − | nd | − |
| + (amx) | ||||||||||
| + (amp) | ||||||||||
| 4 | F | 42 | amx/clav | cutaneous | immediate | − | + (pen) | − | nd | − |
| 5 | M | 56 | pen | cutaneous+respiratory | immediate | + (MDM) | nd | − | nd | − |
| 6 | M | 44 | pen | respiratory | immediate | − | − | amx: 0.6 | nd | − |
| penG: 0.5 | ||||||||||
| penV: 1.3 | ||||||||||
| 7 | F | 66 | cef | cutaneous+respiratory | immediate | − | − | amx: 0.8 | nd | − |
| penG: 1.4 | ||||||||||
| penV: 2.3 | ||||||||||
| 8 | M | 4 | cef | cutaneous+digestive | non-immediate | − | − | penG: 1.29 | nd | − |
| penV: 1.83 | ||||||||||
| 9 | F | 10 | amx/clav | cutaneous+digestive | non-immediate | − | − | penV: 0.4 | nd | nd |
| 10 | F | 37 | amx/clav+cef | cutaneous | non-immediate | − | − | penG: 0.41 | nd | − |
| 11 | M | 4 | amx/clav+cef | cutaneous | immediate | − | − | penV: 0.53 | nd | nd |
| amp: 1.03 | ||||||||||
| 12 | M | 47 | amx/clav+cef | cutaneous | immediate | − | − | penG: 0.4 | nd | − |
| penV: 0.7 | ||||||||||
| 13 | F | 53 | cef | cutaneous+respiratory | immediate | − | − | penG: 0.4 | nd | − |
| penV: 0.5 | ||||||||||
| 14 | F | 63 | amx/clav | cutaneous+respiratory | immediate | − | − | amx: 1.6 | nd | − |
| penG: 2.9 | ||||||||||
| penV: 2.6 | ||||||||||
| 15 | M | 65 | pen | cutaneous | immediate | − | − | penG: 1.0 | nd | − |
| 16 | F | 36 | pen | cutaneous | immediate | + (amp) | nd | amp: 1.3 | nd | − |
| 17 | F | 47 | pen+amx/clav | cutaneous | immediate | − | − | − | + | − |
| 18 | F | 27 | amx/clav+cef | cutaneous+respiratory | non-immediate | − | − | − | + | − |
Abbreviations: amp: ampicillin; amx: amoxicillin; amx/clav: amoxicillin/clavulanate; cef: cephalosporin; pen: penicillin; nd: not done; −: negative result; +: positive result.
SPT were positive in 3 patients (4%): one to MDM, one to amoxicillin and the other one to ampicillin. IDT were positive in 3 patients (4%): one to PPL (concentration 1/10), one to penicillin (concentration 1/100) and one to penicillin, amoxicillin and ampicillin (concentration 1/100 for all three drugs).
Specific IgE was positive in 11 patients (16%), with values ranging from 0.40 to 2.90kU/L. Only one patient had both positive specific IgE and skin testing.
Of the remaining 51 patients with negative skin tests and specific IgE, 33 were submitted to drug challenge with the culprit antibiotic. This resulted in a positive reaction to amoxicillin in 2 cases (6%). Eighteen patients did not perform the drug challenge, either due to the severity of the previous reaction or because they refused it.
In all cases with confirmed allergy diagnosis to the culprit beta-lactam a drug challenge with an alternative drug was done, with negative results in all patients.
DiscussionOf the 67 studied cases with history of beta-lactam hypersensitivity reactions, 18 (27%) were confirmed as being allergic after complete study. A final diagnosis was based on a positive history as well as positive skin tests (9%) and/or positive specific IgE determination (15%) and/or positive drug challenge tests (3%). Similar results were published by Bousquet et al.16, in a paper with 1218 cases of suspected beta-lactam allergy, where 21.1% were confirmed after skin tests and oral drug challenges.
Considering only the 18 patients in whom diagnosis was confirmed after full work-up, the authors emphasize that in 11% with both negative skin tests and specific IgE, the diagnosis would not be possible without a provocation test. Similarly, in a paper by Torres et al.11, a very significant proportion of cases with a clear positive history of immediate allergic reaction, with both negative skin tests and specific IgE, were confirmed as allergic by a positive drug challenge. Also, in the paper by Bousquet et al.16 mentioned above, 30.7% of cases of beta-lactam allergy were confirmed by drug challenge (and by skin tests in the remaining 69.3%). In our study, a significant number of drug challenges were avoided by determination of the specific IgE in all patients (with positive results in nine). This explains the lower proportion of cases diagnosed by drug challenge, as compared to the previously mentioned study. This hypothesis is supported by the results of a study by Blanca et al.10, which showed that in patients with negative skin tests and a positive drug provocation challenge to the culprit beta-lactam, the determination of specific IgE to penicillin or amoxicillin was positive in 42% of cases.
Therefore, a combination of skin testing, specific IgE determination and drug challenge is necessary since none has sufficient sensitivity to be used alone.
As discussed by Blanca et al.17 and Torres et al.11, several factors may be responsible for negative skin tests in patients with confirmed allergy, such as: 1) a selective IgE response to an untested beta-lactam; 2) skin test negative but specific IgE positive; 3) loss of skin sensitivity due to the natural evolution of beta-lactam allergy.
In our study, a major proportion of so-called “allergic” patients (73%) were in fact confirmed as non-allergic, and can safely take the suspected antibiotic, without the need to use a more expensive and/or less adequate alternative. In cases of confirmed beta-lactam allergy, a drug challenge with an alternative antibiotic is indicated, in order to determine a safe alternative.
Some limitations of this study cannot be overruled such as: 1) a small sample size; 2) variable time between the hypersensitivity reactions and work-up; 3) absence of available antibodies for detection of specific IgE for most cephalosporins; 4) patients who refused to undergo drug challenge.
Final CommentsConsidering the 16 patients with positive skin tests or positive specific IgE, the authors wish to stress the fact that only one patient had both positive skin tests and specific IgE, to emphasize that skin tests cannot replace specific IgE determination, nor vice versa.
Also, considering only the patients in whom diagnosis was confirmed after full work-up, the authors point out that a significant proportion (11%) had both negative skin tests and specific IgE, and the diagnosis would not be possible without a provocation test.
Therefore, a combination of skin testing, specific IgE determination and drug challenge is necessary in the diagnosis of beta-lactam allergy since none has sufficient sensitivity to be used alone.
The complete work-up of patients with suspected beta-lactam hypersensitivity reactions, in our study, allowed the removal of the “allergic” label in a major proportion of patients (approximately three quarters) who were in fact confirmed as non-allergic. This avoids the need to use a less adequate and/or more expensive alternative.