Cigarette consumption among teenagers is one of the most critical health-related risk behaviors.
MethodProspective study carried out in seven sites of five Latin American countries (Argentina [Cordoba, N=958, Corrientes, N=1013], Brazil [Curitiba, N=650; Uruguaiana, N=997], Cuba [Havana, N=1004], Mexico [Veracruz, N=991] and Paraguay [Ciudad del Este, N=868]) with public-school adolescents (aged 12–19 years). Respondents were asked to answer the California Student Tobacco Survey.
Results6550 adolescents took part in the survey (average age: 14 years). 38.5% (N=2517) “tried smoking” and 37.5% started smoking before the age of 12. Sixty-one percent of adolescents think that cigarettes are easily accessible; 41.7% considered that smokers have more friends; 88% indicated knowledge of the harms of smoking one to five cigarettes per day; 58.9% would smoke new cigarette types with less harmful substances; 27.8% have already used e-cigarettes; 28% have smoked hookah. Fifty-seven point five percent have been, in the past seven days, in the same room with someone who was smoking a cigarette; and 30.5% indicated that there were not any no-smoking rules inside their homes. Identifiable risk factors were (logistic regression analysis): smoking cigarettes offered by friends, smoking cigarettes with less harmful substances, knowing what a hookah is, being in the same room with a smoker in the past week. Identifiable protective factors against tobacco use were: knowing the health risks caused by smoking hookah and to have their own room.
ConclusionYouth tobacco use in Latin America is a major public health concern, and tobacco control measures are highly needed.
Tobacco use is the world's leading preventable cause of illness and death. It is the number one independent risk factor for chronic diseases. It is estimated to cause 70% of lung, bronchus and trachea cancer, and 11% of deaths from coronary artery disease.1
Cardiovascular diseases kill 18 million people each year and account for 44% of deaths from noncommunicable diseases (NCDs). Three million of these deaths are caused by tobacco use and secondhand smoking.2 It is estimated that most of these deaths will occur in low- and middle-income countries, with a significant impact on morbidity and mortality rates, direct health-care expenditures, and tobacco use productivity losses.3
Tobacco-control measures require effective and systematic monitoring to assess tendencies related to the use of tobacco and tobacco-derived products. Studies show that 50% of young men and 10% of young women start smoking very early,5,6 and three out of five youths who smoke cigarettes will grow up to become adult smokers.7,8
Adolescence is recognizably a key period of social vulnerability to the adoption of risk behaviors.7 Even though teenagers are aware of these risk situations, they end up adopting behaviors and attitudes likely to compromise their health,9,10 and most habits acquired during this life stage are carried on well into adulthood, being extremely hard to break.11
During the past years, different theories and models had been proposed to explain the influence that social context and environment have on youth behavior and tobacco use initiation,12 such as individual factors (age, low self-esteem, perception of risk),13,14 family factors (parental smoking, educational level, parental attitude toward tobacco),15,16 social factors (peer groups),17 school environment (debates, smoking prevention programs, lack of school-based anti-tobacco policies),18,19 environmental factors (advertising, availability),20 and tobacco industry promotional and advertising activities.21,22
Moreover, adolescent smokers consume three times more alcohol, use eight times more marijuana, and 22 times more cocaine than their non-smoking peers. Smoking youths also display other risk behaviors like unsafe sex and physical aggression, factors that together contribute to an increase in health-related differences between the two groups.13
Therefore, special efforts have been made in the past few years to influence adolescent behavior through appropriate interventions to help them avoid tobacco use in the early stages of their lives.19
Cigarette consumption among adolescents is one of the most important health-related risk behaviors, and it is, therefore, necessary to know tobacco consumption data and tobacco-related factors, as well as the impact of new forms of tobacco use linked to other illegal drugs to establish public health policies tailored toward each specific reality.
Casuistic and methodsProspective study carried out between March 2016 and June 2017 in seven cities of five Latin American countries (Argentina [Cordoba, N=958, Corrientes, N=1013], Brazil [Curitiba, N=650; Uruguaiana, N=997], Cuba [Havana, N=1004], Mexico [Veracruz, N=991] and Paraguay [Ciudad del Este, N=868]). Adolescent students aged between 12 and 19 years and attending local public schools participated in the study. Participating schools had been previously identified by state departments of education and drawn by lottery to participate in the study.
Adapted and validated Portuguese or Spanish versions of the California Tobacco Survey23 were completed by the students during regular class hours with no interference from the researcher. One day before survey completion, students were informed about the study and handed Parental Informed Consent Forms to be signed by their parents or legal guardians. Students with parental authorization also signed an Assent Form at the moment of survey completion. The Research and Ethics Committee of each participating site approved the study.
For confidentiality reasons, adolescent participation in the survey was anonymous, with no personal identification apart from gender, age, weight, and height. The researcher responsible for each participating site had previously trained the professionals who supervised the completion of the surveys.
In this study, a “ever tried smoking” was the youth who reported ever smoking a cigarette in their lifetime (Have you ever tried a cigarette, even if only one or two puffs?). Adolescents that smoke cigarettes on one or more days during the past 30 days are considered “current smokers.” Both definitions meet the recommendations by the World Health Organization (WHO), the US Centers for Disease Control and Prevention (CDC), and the Global Youth Tobacco Survey (GYTS).4,8,24
Statistical analysisAfter review of the survey booklets, those adequately completed were entered in double-entry form into an Excel spreadsheet for statistical analysis. Tobacco use (tried smoking) was employed as the dependent variable. Results were presented in relation to exposure or non-exposure to smoking. Non-parametric tests were used: The Chi-square test or the Fisher exact test, with rejection of the null hypothesis at a five percent level. Identifiable significant variables (p<0.05) were included in a logistic regression model (stepwise backward), with identification of Odd Ratio (OR) values as well as confidence intervals of 95% (95% CI).
ResultsSix-thousand-five-hundred-fifty (6550) questionnaires completed by adolescents from seven Latin American sites were included in the study. The average age of participant students was 14 years, with equal distribution of male and female participants.
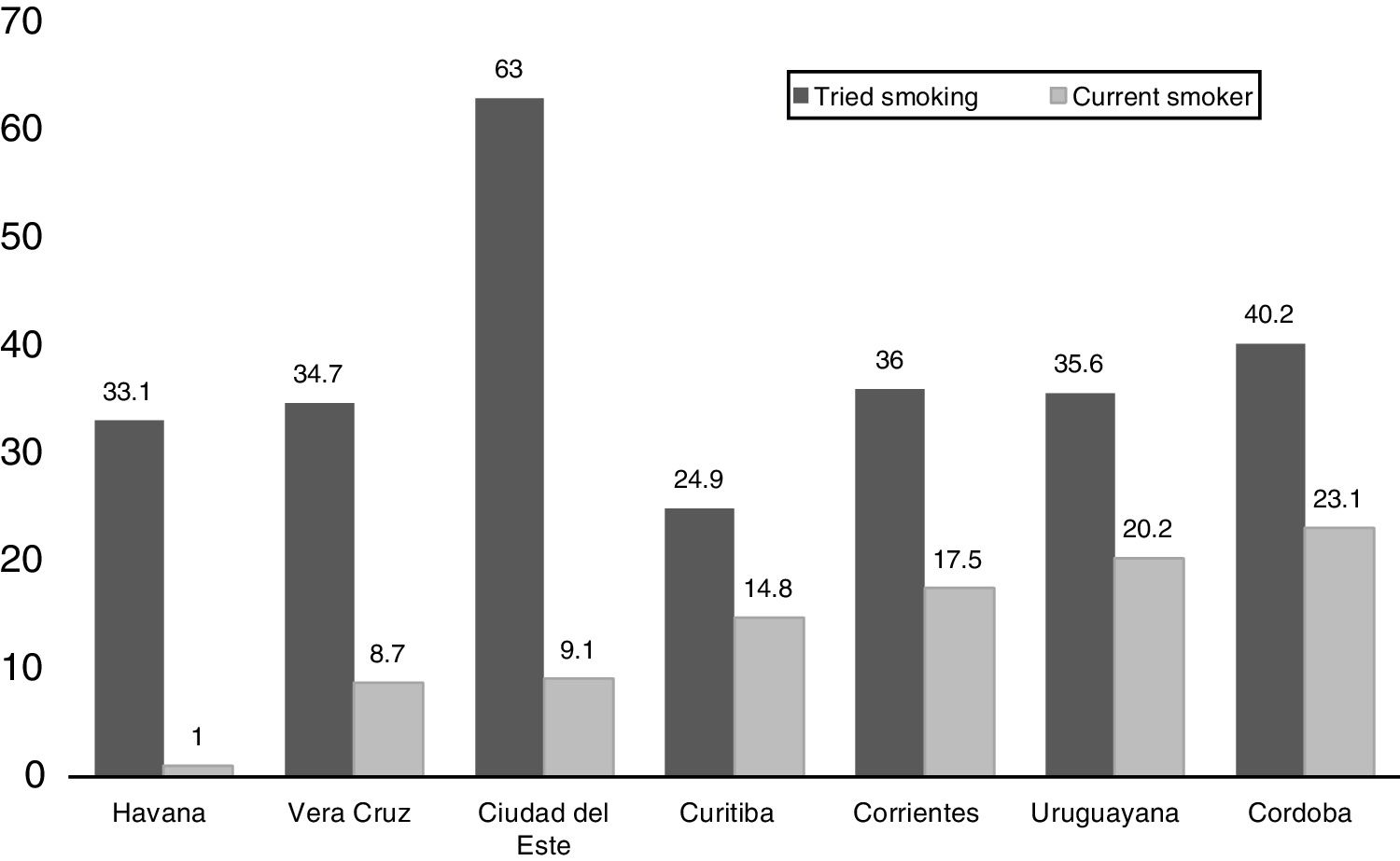
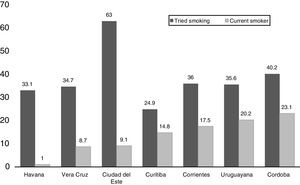
Fig. 1 shows the distribution of adolescents who ever tried smoking in each site (percentage in relation to the total number of surveyed adolescents). A heterogeneous distribution could be verified, ranging between 24.9% in Curitiba and 63.0% in Ciudad del Este, with a mean value of 38.5%. Nevertheless, the percentage of current smokers among those who ever tried smoking did not correspond to these rates, ranging from 1% in Havana to 23.1% in Cordoba.
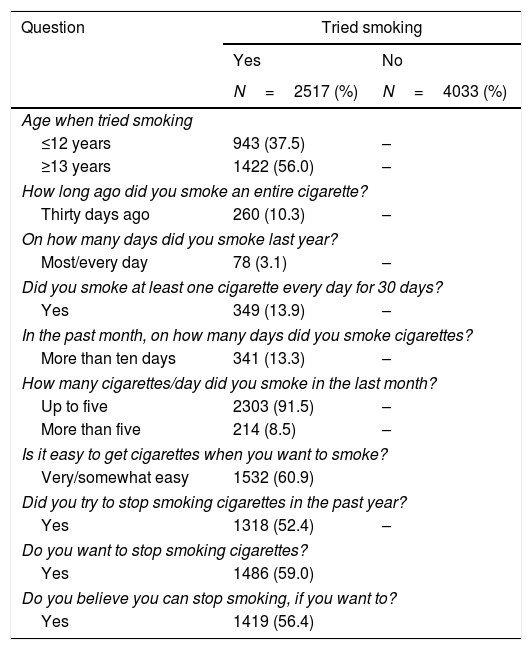
The overall sample can be found in Table 1, distributed under the categories “ever tried smoking” (n=2517 or 38.5%, where 48% are female) and those who answered no, as in “never smoked” (n=4033 or 61.5%, where 55% are female).
Adolescents’ answers regarding tobacco use.
| Question | Tried smoking | |
|---|---|---|
| Yes | No | |
| N=2517 (%) | N=4033 (%) | |
| Age when tried smoking | ||
| ≤12 years | 943 (37.5) | – |
| ≥13 years | 1422 (56.0) | – |
| How long ago did you smoke an entire cigarette? | ||
| Thirty days ago | 260 (10.3) | – |
| On how many days did you smoke last year? | ||
| Most/every day | 78 (3.1) | – |
| Did you smoke at least one cigarette every day for 30 days? | ||
| Yes | 349 (13.9) | – |
| In the past month, on how many days did you smoke cigarettes? | ||
| More than ten days | 341 (13.3) | – |
| How many cigarettes/day did you smoke in the last month? | ||
| Up to five | 2303 (91.5) | – |
| More than five | 214 (8.5) | – |
| Is it easy to get cigarettes when you want to smoke? | ||
| Very/somewhat easy | 1532 (60.9) | |
| Did you try to stop smoking cigarettes in the past year? | ||
| Yes | 1318 (52.4) | – |
| Do you want to stop smoking cigarettes? | ||
| Yes | 1486 (59.0) | |
| Do you believe you can stop smoking, if you want to? | ||
| Yes | 1419 (56.4) | |
Among those who “ever tried smoking”, 37.5% smoked their first cigarette before age 12 years, whereas 56% smoked their first cigarette after age 13 years. 3% of adolescents reported smoking most days or every day in the past year; 13.9% reported smoking at least one cigarette per day in the past 30 days; 8.5% indicated smoking more than five cigarettes per day in the past month; 61% of adolescents indicated easy accessibility to cigarettes whenever they felt like smoking; 59% indicated wanting to quit smoking; 52% reported trying to quit smoking in the past year; and only 56% of participant adolescents believe they would quit smoking if they wanted (Table 1).
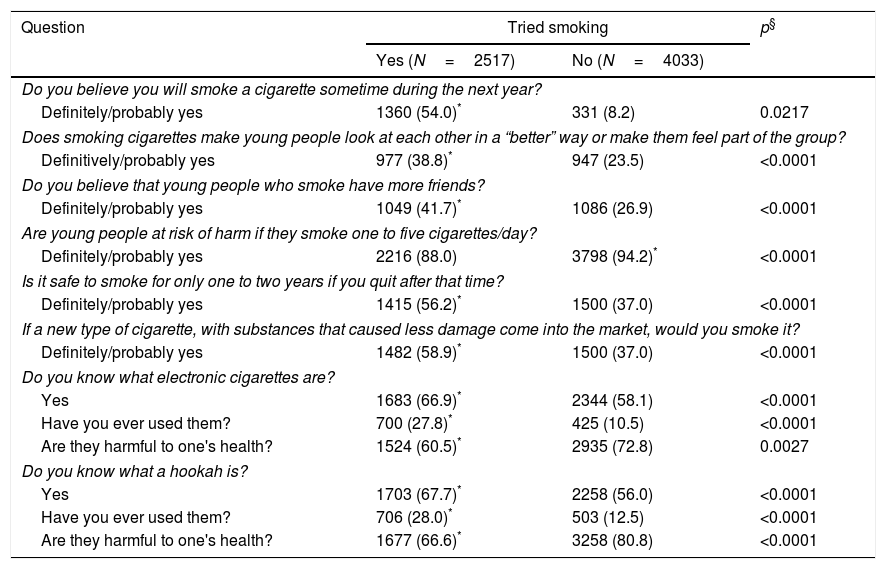
As to their attitude toward tobacco consumption, 54% of the surveyed adolescents believe they will continue smoking in the next year, 38.8% believe smoking makes them more accepted by their friends, and 41.7% think that youth smokers have more friends. Even with 88% of the youth reporting awareness of the health risks associated with smoking one to five cigarettes per day, 56.2% of them think that it is safe to smoke for a period of one year or two, and then quit smoking after this time (Table 2).
Adolescents’ answers regarding thoughts about tobacco use.
| Question | Tried smoking | p§ | |
|---|---|---|---|
| Yes (N=2517) | No (N=4033) | ||
| Do you believe you will smoke a cigarette sometime during the next year? | |||
| Definitely/probably yes | 1360 (54.0)* | 331 (8.2) | 0.0217 |
| Does smoking cigarettes make young people look at each other in a “better” way or make them feel part of the group? | |||
| Definitively/probably yes | 977 (38.8)* | 947 (23.5) | <0.0001 |
| Do you believe that young people who smoke have more friends? | |||
| Definitely/probably yes | 1049 (41.7)* | 1086 (26.9) | <0.0001 |
| Are young people at risk of harm if they smoke one to five cigarettes/day? | |||
| Definitely/probably yes | 2216 (88.0) | 3798 (94.2)* | <0.0001 |
| Is it safe to smoke for only one to two years if you quit after that time? | |||
| Definitely/probably yes | 1415 (56.2)* | 1500 (37.0) | <0.0001 |
| If a new type of cigarette, with substances that caused less damage come into the market, would you smoke it? | |||
| Definitely/probably yes | 1482 (58.9)* | 1500 (37.0) | <0.0001 |
| Do you know what electronic cigarettes are? | |||
| Yes | 1683 (66.9)* | 2344 (58.1) | <0.0001 |
| Have you ever used them? | 700 (27.8)* | 425 (10.5) | <0.0001 |
| Are they harmful to one's health? | 1524 (60.5)* | 2935 (72.8) | 0.0027 |
| Do you know what a hookah is? | |||
| Yes | 1703 (67.7)* | 2258 (56.0) | <0.0001 |
| Have you ever used them? | 706 (28.0)* | 503 (12.5) | <0.0001 |
| Are they harmful to one's health? | 1677 (66.6)* | 3258 (80.8) | <0.0001 |
58.9% of participants reported smoking new types of cigarette with substances that cause less health-related harm; 66.9% of surveyed youths reported knowing electronic cigarettes; 27.8% reported having used e-cigarettes before, although 60.5% of them think e-cigarettes cause health-related issues. As to hookahs, 67.7% of surveyed youth know them, 28% have tried smoking hookah before, and 66.6% of youth are aware that hookah smoking is harmful to their health (Table 2).
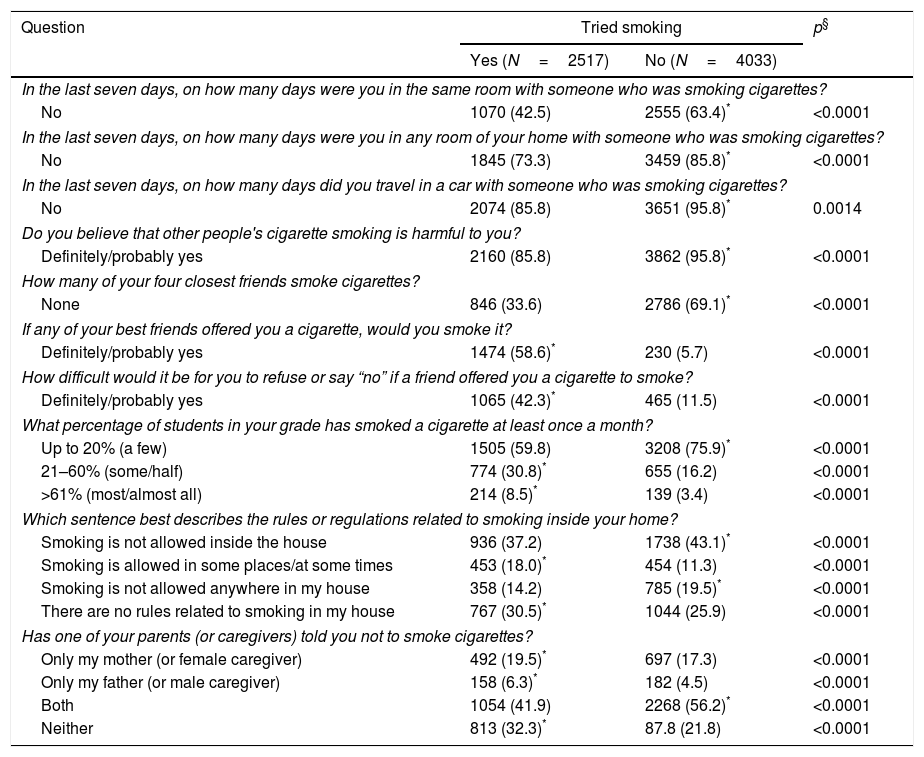
As to exposure to other people's smoke (secondhand or passive smoking), 57.5% of youths were, over the past seven days, in the same room with someone who was smoking a cigarette; 85.8% believe that other people's smoke damages their health; only 34% of respondents do not have a smoker among their four best friends; 58.6% indicated they would accept a cigarette from their best friends. Among non-smokers, only 5.7% indicated they would do so (Table 3).
Adolescents’ answers related to exposure to other people's smoking.
| Question | Tried smoking | p§ | |
|---|---|---|---|
| Yes (N=2517) | No (N=4033) | ||
| In the last seven days, on how many days were you in the same room with someone who was smoking cigarettes? | |||
| No | 1070 (42.5) | 2555 (63.4)* | <0.0001 |
| In the last seven days, on how many days were you in any room of your home with someone who was smoking cigarettes? | |||
| No | 1845 (73.3) | 3459 (85.8)* | <0.0001 |
| In the last seven days, on how many days did you travel in a car with someone who was smoking cigarettes? | |||
| No | 2074 (85.8) | 3651 (95.8)* | 0.0014 |
| Do you believe that other people's cigarette smoking is harmful to you? | |||
| Definitely/probably yes | 2160 (85.8) | 3862 (95.8)* | <0.0001 |
| How many of your four closest friends smoke cigarettes? | |||
| None | 846 (33.6) | 2786 (69.1)* | <0.0001 |
| If any of your best friends offered you a cigarette, would you smoke it? | |||
| Definitely/probably yes | 1474 (58.6)* | 230 (5.7) | <0.0001 |
| How difficult would it be for you to refuse or say “no” if a friend offered you a cigarette to smoke? | |||
| Definitely/probably yes | 1065 (42.3)* | 465 (11.5) | <0.0001 |
| What percentage of students in your grade has smoked a cigarette at least once a month? | |||
| Up to 20% (a few) | 1505 (59.8) | 3208 (75.9)* | <0.0001 |
| 21–60% (some/half) | 774 (30.8)* | 655 (16.2) | <0.0001 |
| >61% (most/almost all) | 214 (8.5)* | 139 (3.4) | <0.0001 |
| Which sentence best describes the rules or regulations related to smoking inside your home? | |||
| Smoking is not allowed inside the house | 936 (37.2) | 1738 (43.1)* | <0.0001 |
| Smoking is allowed in some places/at some times | 453 (18.0)* | 454 (11.3) | <0.0001 |
| Smoking is not allowed anywhere in my house | 358 (14.2) | 785 (19.5)* | <0.0001 |
| There are no rules related to smoking in my house | 767 (30.5)* | 1044 (25.9) | <0.0001 |
| Has one of your parents (or caregivers) told you not to smoke cigarettes? | |||
| Only my mother (or female caregiver) | 492 (19.5)* | 697 (17.3) | <0.0001 |
| Only my father (or male caregiver) | 158 (6.3)* | 182 (4.5) | <0.0001 |
| Both | 1054 (41.9) | 2268 (56.2)* | <0.0001 |
| Neither | 813 (32.3)* | 87.8 (21.8) | <0.0001 |
As to smoking rules at their homes, 30.5% of the surveyed students reported absence of smoking-related household rules, even though 41.9% of them indicated that both parents had advised them not to smoke, and 32.3% had been warned by their parents about the dangers of cigarette use (Table 3).
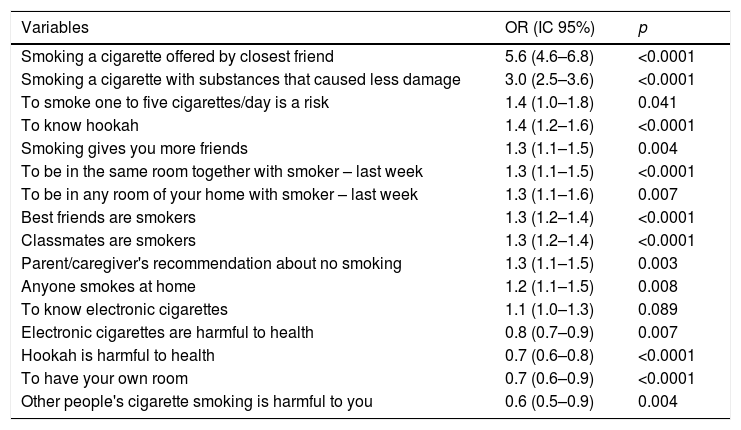
Table 4 shows risk/protective factors associated with tobacco use identified by bivariate analysis and verified by logistic regression analysis. Major identifiable risks were: smoking cigarettes offered by friends, smoking cigarettes with less harmful substances, knowing what a hookah is, being in the same room with smokers in the past week. The identifiable protective factors were knowing the health risks caused by smoking hookah and having their own room (Table 4).
Factors identified as associated as related to smoking in adolescence after logistic regression analysis.
| Variables | OR (IC 95%) | p |
|---|---|---|
| Smoking a cigarette offered by closest friend | 5.6 (4.6–6.8) | <0.0001 |
| Smoking a cigarette with substances that caused less damage | 3.0 (2.5–3.6) | <0.0001 |
| To smoke one to five cigarettes/day is a risk | 1.4 (1.0–1.8) | 0.041 |
| To know hookah | 1.4 (1.2–1.6) | <0.0001 |
| Smoking gives you more friends | 1.3 (1.1–1.5) | 0.004 |
| To be in the same room together with smoker – last week | 1.3 (1.1–1.5) | <0.0001 |
| To be in any room of your home with smoker – last week | 1.3 (1.1–1.6) | 0.007 |
| Best friends are smokers | 1.3 (1.2–1.4) | <0.0001 |
| Classmates are smokers | 1.3 (1.2–1.4) | <0.0001 |
| Parent/caregiver's recommendation about no smoking | 1.3 (1.1–1.5) | 0.003 |
| Anyone smokes at home | 1.2 (1.1–1.5) | 0.008 |
| To know electronic cigarettes | 1.1 (1.0–1.3) | 0.089 |
| Electronic cigarettes are harmful to health | 0.8 (0.7–0.9) | 0.007 |
| Hookah is harmful to health | 0.7 (0.6–0.8) | <0.0001 |
| To have your own room | 0.7 (0.6–0.9) | <0.0001 |
| Other people's cigarette smoking is harmful to you | 0.6 (0.5–0.9) | 0.004 |
OR – odds ratio; 95% CI – 95% confidence interval.
Tobacco use is one of the leading causes of health inequities worldwide, and adolescence is the life stage when young people are particularly vulnerable to experiment with and to reproduce behaviors due to their great socialization needs and acquisition of new values and attitudes. For these reasons, this study sought to assess the prevalence and factors associated with tobacco consumption among Latin American adolescents.
The study of data collected within the same period and using the same research protocol allowed for a more accurate assessment of the real interference of smoking habits among youth, for establishing comparisons and especially for a temporal analysis of smoking rates in Latin America, as opposed to other studies carried out in the same region that were limited by their methodological scope.25
The latest World Health Organization (WHO) report on tobacco use control policies worldwide highlights the difficulties in objectively assessing and comparing tendencies and projections since some of the regions that failed to implement tobacco control measures tend to provide less robust data on their current situation.2 This report points to considerable differences between countries and regions. While 62 million smokers in high-income countries quit smoking between 2000 and 2015, the number of smokers in low and middle-income countries increased by 33 million. Efforts to reduce tobacco use in these countries have been hampered by the relentless lobbying of the tobacco industry, which has hindered governments from introducing stronger policies.2,21,22
This regrettable situation has been confirmed by our study that shows a high prevalence of tobacco use among students in the participating countries (38.5%). This fact serves as a warning. It shows that the problem remains even after the introduction of the MPOWER program through the WHO Tobacco Free Initiative, based on measures stated in the Framework Convention on Tobacco Control (FCTC) to reduce tobacco use prevalence, signed by 168 countries in 2005, 29 of them in the Americas. Very few of these countries were able to execute FCTC measures for a full implementation of effective tobacco control and prevention policies.26,27
As demonstrated in other studies,14 our study shows that overall tobacco consumption prevalence is higher among male students. It is worth noting that 37.5% of participant students started smoking cigarettes before the age of 12, as reported by other authors,12,25 but differently from the late initiation age (13 years) provided by the WHO report data and by other authors.2,28,29 The early initiation of tobacco use verified in our study constitutes an important prognostic factor for smoking-related diseases and as such it should be prevented at a very early stage.3
It is very concerning that 54% of the surveyed adolescents believe they will continue smoking in the next year, thus exposing themselves to the risks of becoming adult smokers.5 Moreover, the fact that 60.9% of the students reported finding very easy to get cigarettes when they wanted to smoke sends a clear warning that authorities have the responsibility to continue imposing limitations to tobacco use, raising tobacco-related taxes as recommended by the MPOWER program,7 and not ignoring the possibility of illegal selling of cigarettes to minors, as pointed out by other studies.30,31
Even though 88% of the youths were aware of the health consequences of smoking 1 to 5 cigarettes per day, we found out that more than half of them (56.2%) believe that it is safe to smoke for one or two years, and then quit smoking after this time. This demonstrates that continuous and permanent warning measures must be implemented as the consequences of tobacco use will only appear in adulthood.11 Moreover, there is also the possibility of exposure to other illegal drugs or tobacco products.32
Smoking cigarettes with less harmful substances and knowing what hookahs are were identified as risk factors for youth smoking. The most recent WHO report estimates that 13.4 million (3.6%) of the world's population aged 13–15 years use smokeless tobacco products.2 The high use of new tobacco forms among adolescents is in part due to lack of knowledge about the real health risks associated with tobacco products such as electronic cigarettes.33
Studies show that among youth cigarette experimenters, the use of electronic cigarettes is independently associated with current conventional tobacco initiation. This suggests that electronic cigarette use does not divert from conventional cigarette use but can drive cigarette consumption in the sampled group.34
Another new form of tobacco use is smoking hookah. An average hookah session lasts 20–80min, with smokers taking between 50 and 200 puffs per session, the same smoke amount they would have inhaled if smoking 100 or more cigarettes.35 Education of youth about new tobacco products is essential since knowing the health risks associated with hookah smoking appears in our study as a protective factor for smoking among youth.
There are multiple factors leading to youth smoking and for continued use of tobacco. Among the social factors, the role of the family must be highlighted. Adolescents are less susceptible to tobacco consumption especially if the family does not allow smoking in the house, if the family is constantly monitoring them and is actively protective against smoking habits, stimulating youth self-care and responsibility.15,16
Our findings show that 32.3% of the adolescents were not warned by their parents about the risks of cigarette smoking. For 30.5% of them, there are no rules for cigarette use in their households. A significant part of the surveyed youths (73.3%) has been exposed to a smoker in a room inside their houses. This is a surprising fact, considering that this situation has been identified in our study as an independent risk factor for youth tobacco use. Scientific evidence indicates that there are no safe levels of secondhand or passive exposure to cigarette smoke.36 This fact was substantiated by our study in that we identified having their own room as a protective factor against tobacco use among adolescents.
Peer pressure plays a vital role in this study since smoking cigarettes offered by friends, having smoking best friends and classmates figured as independent risk factors for youth smoking, a fact already confirmed by other studies.17,30 Therefore, peer selection and peer influence are fundamental in shaping smoking behaviors, and both play a role in smoking initiation and maintenance of adolescent smoking habits.37,38
School-based smoking prevention programs should take both types of influence networks into consideration, not only providing information but also conveying skills for youths to interact with their peers.10,18,19 Schools must also recognize the important role of these programs in contributing for smoking cessation among youth. In our study, 59% of respondents indicated they wanted to stop smoking, 52% reported trying to quit smoking in the past year, and 54% believe they will continue smoking in the next year. This situation deserves consideration by schools and families.39
Our study has some limitations since it was carried out with schooling adolescents, therefore excluding out-of-school youths. This limits the scope and a broader application of the results. Out-of-school youths in Latin America normally come from lower socioeconomic backgrounds, and there is much variation between the countries studied. Moreover, the possibility of bias should also be considered since the survey, even if anonymous, was completed under supervision and students might have felt the need to please or hide inadequate behaviors. Because of the cross-sectional approach of this study, where outcome and risk factors have been observed at a fixed point in time, reverse causality biases cannot be ruled out. However, taking the uniformity of our research method into account, we believe to have delivered an accurate and actual portrayal of tobacco consumption and tobacco-related risk factors among adolescents in Latin America.
As a conclusion, our data show that it is highly unlikely that Latin-American countries will meet the Global Target of 30% relative reduction in prevalence of current tobacco use established in the Global Action Plan for NDCs. However, our data can contribute as a warning for planning future tobacco control actions to promote the health and wellbeing of populations everywhere, but especially where the data was collected, and this harsh reality be apprehended.
Conflict of interestThe authors have no conflict of interest to declare.