Children with IgE-mediated cow's milk allergy (IgE-CMA) with gastrointestinal symptoms tolerate yogurt at 100%. Yogurt tolerance in children with IgE-CMA with urticaria and anaphylaxis was 7%.
MethodsWe enrolled children with IgE-CMA with cutaneous, respiratory, gastrointestinal and anaphylactic symptoms. All performed prick by prick (PbP) and oral food challenge (OFC) with yogurt. Some children performed also an OFC with CM mixed with wheat flour and baked, baked liquid CM, parmesan.
Results34 children were enrolled, 31/34 (91%) with systemic adverse reaction after ingestion of CM (systemic CMA), 3/34 (9%) with isolated contact urticaria (ICU CMA). PbP with yogurt was negative only in one patient. OFC with yogurt was passed (that is, the OFC was negative) by 20/31 (64%) of the children with systemic CMA. 10/11 (91%) of the patients who failed OFC (that is, the OFC was positive) with yogurt were positive to SPT with casein vs. 8/20 (40%) of the patients who passed it (p=0.018). None of the 19 children who passed OFC with yogurt failed all OFC with processed CM forms other than yogurt that tested vs. 4/8 among those who failed OFC with yogurt (p=0.006). The rub test with yogurt was negative in 1/3 (33%) of the patients with ICU CMA.
ConclusionsThe results of our study are placed alongside others already present in the literature and concerning other methods of processing CM proteins and help to reduce the dietary restrictions of the majority of children with systemic IgE-CMA.
For about a decade it has been known that a significant proportion of children with IgE-mediated cow's milk allergy (IgE-CMA) and IgE-mediated egg allergy can tolerate the culprit food if it is cooked at high temperatures for a sufficiently long time and baked in a matrix of wheat.1,2 These studies showed that the 60%–70% of the children with these two allergies can eat bakery products containing CM or egg proteins, such as muffin or waffle. Subsequently, it has been demonstrated that 60% of children with IgE-CMA tolerate parmesan aged for 36 months.3 In reality, any type of processing can potentially modify CM proteins and, consequently, alter its allergenic capacity, for example the lactic fermentation at the basis of yogurt production.
The lactic fermentation is an enzymatic process caused by bacterial microorganisms: during the fermentation, proteases digest the proteins reducing them in peptides, the lactose is transformed into lactic acid, so the pH is reduced and milk proteins coagulate. The hydrolysis of CM obtained by lactic fermentation probably modifies its allergenic capacity. Some in vitro studies demonstrated that CM proteins are profoundly modified by lactic fermentation with consequently reduction of the binding capacity of the IgE.4 Yogurt is obtained by lactic fermentation operated by two microorganisms: the Lactobacillus delbrueckii subspecies bulgaricus and the Streptococcus salivarius subspecies thermophilus.5 The two microorganisms have a proteolytic action on the CM sieroproteins and this action is demonstrable by electrophoresis and high-performance liquid chromatography.6 Pescuma et al.7 demonstrated that Lactobacillus delbrueckii subsp. bulgaricus is able to degrade the beta-lactoglobulin (BLG) epitopes more than other microorganisms, reducing consequently its ability to be recognized by the specific IgE of the allergic subjects.
Poza-Guedes et al.8 reported that 25/25 children with IgE-CMA tolerated yogurt. The limitation of that study is that it only included children with gastrointestinal symptoms (abdominal pain, diarrhea, constipation). The results of their study are not transferable to all children with IgE-CMA because the organ most frequently involved in the IgE-CMA is cutis (with urticaria and/or angioedema). In fact, Uncuoglu et al.9 have observed that among children with other phenotypes of IgE-CMA (urticaria, anaphylaxis) 15 out of 16 subjects (93%) also reacted to yogurt.
Because of these different results, we have performed a study to evaluate the prevalence of yogurt tolerance in children with IgE-CMA with every type of manifestations, included anaphylaxis.
Methods and patientsAll the pediatric patients with a history of IgE-CMA with every type of manifestations (cutaneous, respiratory, gastrointestinal, anaphylactic), evaluated prospectively and consecutively in the pediatric allergy unit of the Policlinico Gemelli of Rome and of the Civil Hospital of Senigallia in the period between 1st April, 2016 and 30th March, 2018 were considered eligible for the study.
Exclusion criteria were: (a) presence of chronic pathologies or chronic therapies conditioning the immune system's response; (b) impossibility to suspend systemic antihistamine and steroid therapies; (c) consent to be enrolled in the study denied.
All the patients underwent prick by prick (PbP) with pasteurized CM and skin prick test (SPT) with saline solution and histamine (Lofarma, Italy); the procedures were carried out according to the standard international methodology.10 Children with positive PbP for CM (wheal mean diameter≥3mm) were subjected to open OFC 11 and to rub test with CM. Children with a history of anaphylaxis in the 12 months prior to our evaluation were excluded from the OFC (but not from the rub test); anaphylaxis was defined according to Sampson et al.12
Among the eligible patients, we enrolled: (a) children with history of anaphylaxis after ingestion of CM proteins in the 12 months prior to our evaluation and with positive PbP for CM; (b) children with suggestive history of non-anaphylactic manifestations after ingestion of CM proteins or with history of anaphylaxis occurring more than 12 months prior to our evaluation, with positive PbP for CM and failed (i.e. positive) OFC with CM; (c) children with suggestive history of non-anaphylactic manifestations after ingestion of CM proteins or with history of anaphylaxis occurring more than 12 months prior to our evaluation, positive PbP for CM, passed (i.e. negative) OFC with CM and failed rub test.
Enrolled children underwent PbP with yogurt (Yomo, Granarolo, Italy), SPT with extract of casein, BLG, alpha-lactoalbumin, saline solution and histamine (Lofarma, Milan, Italy), and rub test with yogurt. The PbP with yogurt was carried out by placing a drop of yogurt on the fly face of the forearm and pricking through the drop. The rub test was carried out soaking a wad of cotton wool in CM or yogurt and rubbing it gently on the cheeks, the perioral region (excluding the mouth), the neck, the chest, the abdomen and the back of the child. The test was considered failed after the appearance, in the 15min following the execution, of wheal in the rubbed region.
All enrolled children underwent OFC with yogurt within two months of the diagnosis of IgE-CMA. The protocol of OFC with yogurt was identical to that of OFC with CM. The OFC with yogurt were considered passed in the absence of adverse reactions after the ingestion of a total dose of 200g of yogurt.
Some children, whose parents have consented to these further procedures, underwent an OFC with other types of processed CM: (a) CM mixed with wheat flour and cooked at 180°C for 30min (an Italian cake named “ciambellone”); liquid CM baked at 180°C for 30min; (c) parmesan aged 36 months. The methodology of food preparation and the execution of the OFC with these three types of processed CM was previously described.13
The study was approved by each hospital ethics committee. Written informed parental consent was obtained before enrollment.
Statistical analysisDemographic and clinical characteristics of the patients are reported as means, medians and standard deviations for the continuous variables and as frequencies and percentages for the categorical variables. Chi squared test was used for the comparison between percentages. A p value <0.05 was considered statistically significant. Statistical analysis was run by Stanton A. Glanz software for medical analysis, version 5.0.
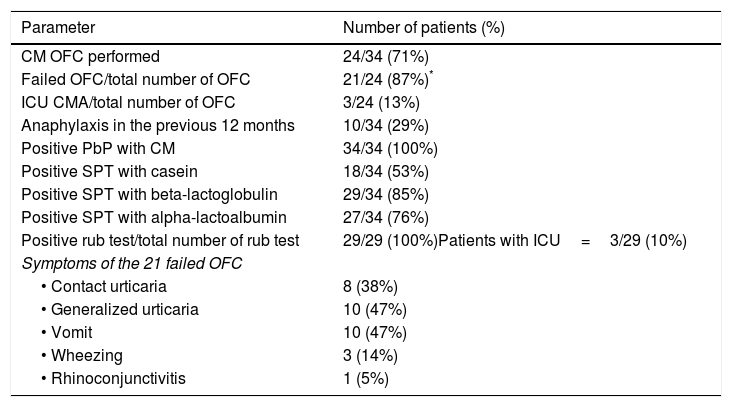
ResultsThirty-four children were enrolled, 31/34 (91%) of whom presented systemic adverse reaction after ingestion of CM (systemic CMA) and 3/34 (9%) presented only cutaneous reaction compatible with the diagnosis of isolated contact urticaria (ICU CMA). On the basis of their history, 97% of them reported mucocutaneous symptoms, 50% gastrointestinal symptoms (vomiting), 29% bronchial symptoms (wheezing), 12% rhinoconjunctival symptoms. There were 22 (65%) male patients, mean age±standard deviation was 17±21 months, median was 10 months and range 3–96 months. 21/34 (62%) received diagnosis of IgE-CMA on the basis of positive PbP with CM and failed OFC with CM; 10/34 (29%) presented a history of anaphylaxis caused by CM in the 12 months prior to our evaluation and positive PbP for CM. The diagnosis of anaphylaxis was always determined by the presence of involvement of respiratory system (wheezing). 3/34 (9%) children received diagnosis of IgE-mediated ICU CMA because of positive PbP with CM, passed OFC with CM and failed rub test with CM. 14/34 (41%) reported other food allergies, 5/34 (15%) asthma and 11/34 (32%) atopic dermatitis. Table 1 shows results of PbP, OFC and rub test with cow's milk.
Results concerning prick by prick, oral food challenge and rub test with cow's milk.
| Parameter | Number of patients (%) |
|---|---|
| CM OFC performed | 24/34 (71%) |
| Failed OFC/total number of OFC | 21/24 (87%)* |
| ICU CMA/total number of OFC | 3/24 (13%) |
| Anaphylaxis in the previous 12 months | 10/34 (29%) |
| Positive PbP with CM | 34/34 (100%) |
| Positive SPT with casein | 18/34 (53%) |
| Positive SPT with beta-lactoglobulin | 29/34 (85%) |
| Positive SPT with alpha-lactoalbumin | 27/34 (76%) |
| Positive rub test/total number of rub test | 29/29 (100%)Patients with ICU=3/29 (10%) |
| Symptoms of the 21 failed OFC | |
| • Contact urticaria | 8 (38%) |
| • Generalized urticaria | 10 (47%) |
| • Vomit | 10 (47%) |
| • Wheezing | 3 (14%) |
| • Rhinoconjunctivitis | 1 (5%) |
OFC, Oral Food Challenge; CM, cow's milk; SPT, skin prick test; ICU CMA, isolated contact urticaria by cow's milk allergy.
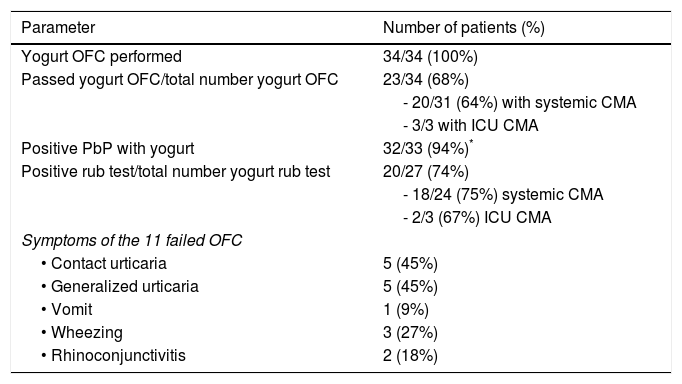
Table 2 shows results concerning PbP, OFC and rub test with yogurt. 23/34 (68%) of the patients ingested yogurt without presenting any adverse reactions. In particular, they were 20/31 (64%) of the children with systemic CMA. PbP with yogurt was negative (wheal mean diameter <3mm) only in one patient, who had failed OFC with CM and negative rub test with yogurt. PbP with yogurt was not performed in one patient with ICU CMA; this patient had a negative rub test with yogurt.
Results concerning prick by prick, oral food challenge and rub test with yogurt.
| Parameter | Number of patients (%) |
|---|---|
| Yogurt OFC performed | 34/34 (100%) |
| Passed yogurt OFC/total number yogurt OFC | 23/34 (68%) |
| - 20/31 (64%) with systemic CMA | |
| - 3/3 with ICU CMA | |
| Positive PbP with yogurt | 32/33 (94%)* |
| Positive rub test/total number yogurt rub test | 20/27 (74%) |
| - 18/24 (75%) systemic CMA | |
| - 2/3 (67%) ICU CMA | |
| Symptoms of the 11 failed OFC | |
| • Contact urticaria | 5 (45%) |
| • Generalized urticaria | 5 (45%) |
| • Vomit | 1 (9%) |
| • Wheezing | 3 (27%) |
| • Rhinoconjunctivitis | 2 (18%) |
OFC, oral food challenge; CMA, cow's milk allergy; ICU CMA, isolated contact urticaria by cow's milk allergy; PbP, prick by prick.
Among the 31 children with systemic CMA: (a) those with mean wheal diameter of yogurt PbP≤3mm (6/31, 19%) always passed OFC with yogurt; and (b) those with mean wheal diameter of yogurt PbP≥11mm (3/31, 10%) always failed OFC with yogurt.
3/11 children with systemic CMA who have failed OFC with yogurt manifested anaphylaxis during this OFC. None of these three children had a history of CM anaphylaxis before the enrollment, but one of them had anaphylaxis during OFC with parmesan. Conversely, of the 10 children with a history of CM anaphylaxis, 70% passed OFC with yogurt; among the remaining 30% who instead failed OFC with yogurt, none failed it with symptoms of anaphylaxis (two presented cutaneous symptoms, and one gastrointestinal symptoms).
The rub test with yogurt was positive in 18/24 (75%) children with systemic CMA who underwent the test. In particular, it was administered in the 11 patients who failed OFC with yogurt and was positive in 10/11 of them. The rub test with yogurt was negative in 1/3 (33%) of the patients with ICU CMA.
Sensitization patterns and tolerance of yogurtAll three of the patients with ICU CMA were sensitized toward BLG and one was also sensitized toward alpha-lactoalbumin, none toward casein. The rub test with yogurt was negative in one of the two patients monosensitized toward BLG.
Among the 31 patients with systemic CMA, 26 (84%) were sensitized toward BLG. 3/26 (11.6%) were monosensitized and all of them passed OFC with yogurt. 9/11 (82%) of the patients who failed OFC with yogurt were positive to SPT with BLG vs. 17/20 (85%) of the patients who had passed it (p=0.78).
Among the 31 patients with systemic CMA, 26 (84%) were sensitized toward alpha-lactoalbumin. 3/26 (11.6%) of them were monosensitized and all of them passed the OFC with yogurt. 10/11 (91%) of the patients who failed OFC with yogurt were positive to SPT with alpha-lactoalbumin vs. 16/20 (80%) of the patients who passed it (p=0.78).
Among the 31 patients with systemic CMA, 18 (58%) were sensitized toward casein. 1/18 (5.5%) was monosensitized and failed the OFC with yogurt. 10/11 (91%) of the patients who failed OFC with yogurt were positive to SPT with casein vs. 8/20 (40%) of the patients who passed it (p=0.018).
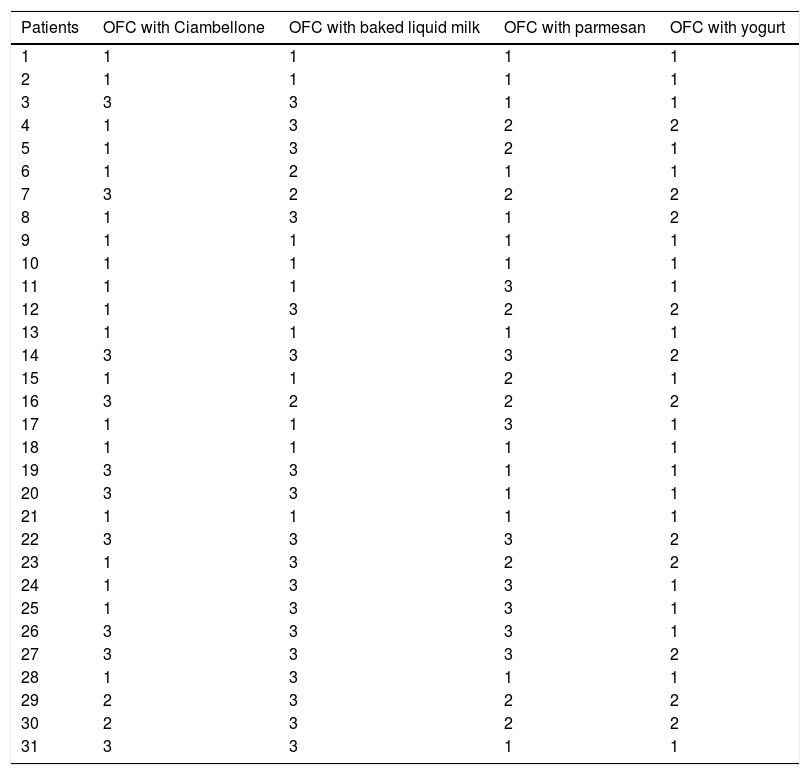
OFC with other forms of processed CMSome patients underwent OFC with parmesan aged 36 months (25 patients), and/or baked milk in wheat matrix (“ciambellone”) (15 patients), and/or baked liquid milk (15 patients) (see Table 3). Parmesan was the form of processing of CM less easily tolerated, “only” 64% of the patients tolerated it. Instead, “ciambellone” and baked liquid milk were tolerated respectively by 87% and 80% of the patients who underwent the OFC with them, with a small matrix effect13 in favor of the “ciambellone”.
OFC with other forms of processed CM.
| Patients | OFC with Ciambellone | OFC with baked liquid milk | OFC with parmesan | OFC with yogurt |
|---|---|---|---|---|
| 1 | 1 | 1 | 1 | 1 |
| 2 | 1 | 1 | 1 | 1 |
| 3 | 3 | 3 | 1 | 1 |
| 4 | 1 | 3 | 2 | 2 |
| 5 | 1 | 3 | 2 | 1 |
| 6 | 1 | 2 | 1 | 1 |
| 7 | 3 | 2 | 2 | 2 |
| 8 | 1 | 3 | 1 | 2 |
| 9 | 1 | 1 | 1 | 1 |
| 10 | 1 | 1 | 1 | 1 |
| 11 | 1 | 1 | 3 | 1 |
| 12 | 1 | 3 | 2 | 2 |
| 13 | 1 | 1 | 1 | 1 |
| 14 | 3 | 3 | 3 | 2 |
| 15 | 1 | 1 | 2 | 1 |
| 16 | 3 | 2 | 2 | 2 |
| 17 | 1 | 1 | 3 | 1 |
| 18 | 1 | 1 | 1 | 1 |
| 19 | 3 | 3 | 1 | 1 |
| 20 | 3 | 3 | 1 | 1 |
| 21 | 1 | 1 | 1 | 1 |
| 22 | 3 | 3 | 3 | 2 |
| 23 | 1 | 3 | 2 | 2 |
| 24 | 1 | 3 | 3 | 1 |
| 25 | 1 | 3 | 3 | 1 |
| 26 | 3 | 3 | 3 | 1 |
| 27 | 3 | 3 | 3 | 2 |
| 28 | 1 | 3 | 1 | 1 |
| 29 | 2 | 3 | 2 | 2 |
| 30 | 2 | 3 | 2 | 2 |
| 31 | 3 | 3 | 1 | 1 |
OFC, oral food challenge. For OFC columns: 1=OFC passed; 2=OFC failed; 3=OFC not performed.
Among the 31 patients with systemic CMA, 27 (87%) carried out at least one OFC with processed CM different from yogurt, that is to say with “ciambellone” and/or baked liquid milk and/or parmesan (Table 3). Of these 27 patients, 19 passed OFC with yogurt. Among these 19, 16 (84%) tolerated all the tested forms of processed CM vs. 1/8 (12.5%) of the children who failed OFC with yogurt (p=0.001). None of the 19 (0%) children who passed OFC with yogurt failed all OFC with the tested forms of processed CM vs. 4/8 (50%) among those who failed OFC with yogurt (p=0.006).
Follow upWe have not performed a regular and methodical follow up on all 23 patients who have passed yogurt OFC. However, we have information regarding 14/23 (61%) patients, of which 11/14 had systemic CMA and 3/14 had ICU CMA. The latter regularly ate yogurt at home without adverse reactions (except for perioral erythema). Of the 11 children with systemic CMA, three reported an adverse reaction: (1) one child reported frequent regurgitation following ingestion of yogurt and did not eat it anymore; (2) another presented angioedema to the auricles and facial erythema three minutes after eating a different brand of yogurt from the one she had tolerated during the OFC; (3) the last child presented generalized rush on the same day of the OFC, four hours after its end, and no longer presented it on the following days while continuing to eat yogurt regularly.
DiscussionThe most relevant result of this study is the demonstration that yogurt is tolerated by 64% of the children with systemic CMA, independently from the types of adverse reaction they presented after CM ingestion. In fact, among the 20 children with systemic CMA who tolerated the yogurt, 7/20 had an history of anaphylaxis during 12 months prior to our evaluation. In any case, the variety of adverse reactions, reported or presented during the course of the OFC with CM, involved multiple organs. This completes the study of Poza-Guedes et al.8 that reported that 25 children with IgE-CMA and gastrointestinal symptoms tolerated yogurt. The results of the study of Poza-Guedes et al.8 were not transferable to all the children with IgE-CMA, and not even to most of them, because the most frequent involved organ in IgE-CMA is cutis. In fact, the same authors have advocated new studies on different phenotypes of IgE-CMA and our study responds to this actual need. We believe that the difference in phenotypes between our study and that of Poza-Guedes et al.8 can justify the difference of percentage of patients who tolerate the yogurt: in our study it is 64%, in Poza-Guedes et al.8 it was 100%. The largest variety of phenotypes enrolled in our study should make our result more transferable to other populations of children with systemic IgE-CMA. In truth, Uncuoglu et al.9 reported much less optimistic results than ours. These authors have observed that 15/16 (93%) children with IgE-CMA, and with urticaria or anaphylaxis as clinical manifestations, reacted to fermented milk.9 The authors9 do not specify the type of fermented milk they used for the OFCs. It is possible that they used a type of fermented milk different from that used by us and that this justifies the difference in the results. The term “yogurt” is intended for a particular product, it must contain two microorganisms: the Lactobacillus delbrueckii Subspecies bulgaricus and the Streptococcus salivarius Subspecies thermophilus.5 Our results are likely to be transferable only to fermented milk that can be called “yogurt”, and perhaps only to the same brand, if we consider the results of our follow up.
Regarding the possibility of predicting the outcome of the OFC with yogurt, we observed two cut-offs about the mean diameter of the wheal evoked by PbP with yogurt: if ≤3mm we have 100% of probability to have a passed OFC with yogurt; if ≥11mm we have 100% of probability to have a failed OFC with yogurt. Moreover, we have also observed that monosensitization to BLG or alpha-lactoalbumin can predict a tolerance of the yogurt of 100%. However, these results were obtained on a very small number of children and this limits reproducibility on more consistent numbers. The results concerning the sensitization to casein were obtained on a larger sample of patients. 10/11 (91%) patients who had failed OFC with yogurt were positive to SPT with casein vs. 8/20 (40%) patients who passed it (p=0.018). Thus, casein sensitization is a negative risk factor toward yogurt tolerance. This is a result similar, as an immunopathogenetic hypothesis, to that reported by Alessandri et al.3 who reported that the absence of IgE for BLG is a marker of tolerance to parmesan. That is, if a patient has specific IgE against a protein that is present in unmodified form in a type of CM processed product it is less likely that this patient will tolerate that type of CM processed product. In fact, BLG is almost unmodified in parmesan, casein is almost unmodified in yogurt. Also, it is interesting that some children sensitized to casein tolerate yogurt and some not, we have no explanation for this.
The tolerance toward yogurt was not less frequent in patients with a history of anaphylaxis: if in the entire population of children with systemic CMA it was equal to 64%, in the 10 children with a recent history of anaphylaxis was equal to 70%. Thus, the severity of the adverse reaction to CM is not predictive of tolerance or not to yogurt.
Even in the three children with ICU CMA we observed a “tolerance” to yogurt, although in this case it can be expressed only at the cutaneous level: 1/3 (33%) did not have skin adverse reactions to the rub test with yogurt. It is also interesting to note that the rub test with yogurt was positive in 18/24 of children with systemic CMA. Since 11/31 children with systemic CMA have failed the OFC with yogurt, it is evident that the children who have passed OFC with yogurt have also presented a positive rub test. In short, and hypothetically, the lactic fermentation, which should have destroyed the epitopes responsible for systemic symptoms in these children (meaning those with passed OFC with yogurt and positive rub test with yogurt), has not destroyed another guilty epitope, which must be at least gastrolabile, which is able to induce skin symptoms to the rub test but not to induce systemic symptoms as a result of ingestion of yogurt.
Finally, yogurt tolerance is a marker of tolerance toward other forms of processed CM. Children who tolerated yogurt passed OFCs with other forms of processed CM significantly more frequently than those who failed them.
Author contributionsSerena Monaco and Stefano Miceli Sopo conceived the design of the study and drafting the article. Serena Monaco, Giovanna Russo and Lucia Liotti acquired the data. Alberto Romano and Maria Carmela Verga analyzed the data and interpreted them. All authors revised the article and have given final approval of the version to be published.
FundingDeclaration of all sources of funding for the research reported in the manuscript: none. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
We declare that the work described has not been published previously, that it is not under consideration for publication elsewhere, that its publication is approved by all authors and tacitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder.
Conflict of interestThe authors have no conflict of interest to declare.