Evaluation of liver fibrosis is important for treatment decisions, complications and to predict prognosis in patients with chronic hepatitis B (CHB). Our aim was to develop a new non-invasive fibrosis scoring method and prove its accuracy in the differentiation of no/low grade and advanced fibrosis in patients with CHB.
Patients and methodsOur study included 273 chronic hepatitis B patients who underwent liver biopsy from February, 2007 to February, 2019 with medical records retrospectively reviewed. Preparations of these patients were divided into two groups as ≤ 3 no-low grade fibrosis (n=236) and ≥ 4 advanced fibrosis (n=37) according to histological ISHAK fibrosis scoring system.
ResultsThe newly developed AGAP score and other non-invasive fibrosis scores; Fibrosis-4 index, Aspartate aminotransferase to platelets ratio, Gamma glutamyl transpeptidase to platelet ratio, Goteborg University Cirrhosis Index, King's score, Albumin-bilirubin index, Fibrosis cirrhosis index, Fibrosis index, Fibrosis quotient, Lok score and mean and/or median values of Fibroindex were significantly higher in the advanced fibrosis group compared to the no/low grade fibrosis group (p<0.001). However, there was no significant difference in AAR score among the groups (p=0.265). With cut-off value of 4.038, AUROC value of 0.803, sensitivity of 75.7%, specificity of 73.7% and accuracy of 0.740, AGAP score showed the best performance in advanced fibrosis differentiation compared to 12 other non-invasive fibrosis scoring methods.
ConclusionsThe newly developed AGAP score showed better performance in patients with CHB compared to 12 other non-invasive fibrosis scores in differentiation of no/low grade fibrosis and advanced fibrosis.
Hepatitis B virus (HBV) infection is a serious health problem occurring in different geographical regions in the world with different frequencies despite effective vaccine and antiviral drugs. The global estimated prevalence of HBV infection is 3.9% and affects 291 million individuals, and is more commonly seen in Africa and the Western Pacific [1]. Chronic HBV infection can cause complications ranging from no/low grade fibrosis in the liver to decompensated liver cirrhosis and hepatocellular cancer. Approximately 30-40% of all deaths due to complications from cirrhosis and hepatocellular carcinoma develop as a result of chronic HBV infection. These developing complications are the cause of higher costs in health systems [2]. Evaluation of liver fibrosis is very important for both prognosis and treatment because many complications such as advanced fibrosis cirrhosis and hepatocellular carcinoma are quite common [3]. Invasive or non-invasive methods are used in order to evaluate liver fibrosis, and liver biopsy is the gold standard for evaluating fibrosis. However, as liver biopsy is performed invasively with percutaneous, transjugular or endoscopic ultrasound, it can increase the cost and may cause many complications such as pain, bleeding, infection, perforation, and even death. In addition, sampling error, inconsistency in histological evaluation, and limited and contraindicated cases in dynamic liver fibrosis follow-up are major disadvantages for biopsy [4]. Of the non-invasive methods, transient elastography performed radiologically is the most widely used. However, this is a costly method used in limited centers, and this method has a limited diagnostic defined as patients with chronic hepatitis B infection. Serum markers, another common method among non-invasive methods, are simple, useful and inexpensive. Serum markers, which have been used especially in recent years, were initially limited to hepatitis C, and then they began to be used extensively to evaluate fibrosis in other liver diseases such as HBV and non-alcoholic fatty liver disease [5]. In recent years, an increasing number of non-invasive fibrosis scores have been used and new scores have been developed to evaluate inflammation, fibrosis and treatment response in patients with CHB. There are many studies regarding liver fibrosis evaluation, treatment and follow-up and aspartate aminotransferase-to-platelet ratio index (APRI) and Fibrosis-4 index (Fib-4) in the literature [6–8]. In a study conducted by Teshale et al. it was shown that APRI and Fib-4 markers distinguished F2–F4 from F0 with higher sensitivity and specificity compared to F1 and are beneficial in following the progression of fibrosis [8]. Gamma-glutamyl transpeptidase to platelet ratio (GPR), a recently used non-invasive fibrosis score, was found to be more accurate in evaluating liver fibrosis in chronic HBV infection compared to APRI and FIB-4 [9]. In a study conducted by Dong et al. GPR and King's scores were found to be the most successful scores in distinguishing significant fibrosis in patients with chronic HBV infection [10]. Although there are many studies regarding non-invasive fibrosis scores used in the evaluation of fibrosis in chronic HBV infection, various discussions still continue [11]. New non-invasive scores are needed in order to evaluate advanced fibrosis, since the diagnostic performances of APRI, Fib-4, GPR and others, which are among the non-invasive fibrosis scoring methods, are not completely satisfactory. In this study, our aim was to evaluate the clinical importance of non-invasive scoring methods used in the diagnosis of liver fibrosis and to determine the new non-invasive fibrosis scoring method with high accuracy.
2Materials and methods2.1Study design and patientsThe patients who had positive hepatitis B surface antigen (HBsAg) and underwent liver biopsy from February, 2007 to February, 2019 were determined retrospectively from the medical records of our hospital. Of these patients, those who had at least 6 months of HBsAg positivity and whose HBV-DNA was higher than 2000 IU/ml were defined as patients with chronic hepatitis B infection. Patients who had received hepatitis B treatment, patients who had acute viral infection, other chronic viral infections other than hepatitis B [hepatitis C virus (HCV), hepatitis D virus (HDV), human immunodeficiency virus (HIV)], hepatocellular cancer, chronic liver disease (autoimmune, genetic, drug-induced, and nonalcoholic fatty) and patients with a history of alcohol use (20 grams of alcohol each day) were excluded from this study. A total of 273 patients who complied with these criteria were included in the study. The study was conducted in accordance with the 1975 Helsinki Declaration guidelines and was approved by Ethics Committee of Cumhuriyet University Faculty of Medicine, Turkey (dated: 07/04/2019, issue no: 2019-07/49).
2.2Liver biopsy and histological evaluationLiver biopsy was performed using a 16-gauge needle under ultrasound. These specimens were fixed with 10% formalin, embedded in paraffin and then stained with hematoxylin-eosin. These biopsy materials were stained with histochemical Masson's trichrome and reticular fiber dyes. These preparations were evaluated by two liver pathologists and concluded by a joint decision. Histological necroinflammatory activity and fibrosis staging were performed in biopsy samples according to ISHAK scoring system. ISHAK staging according to fibrosis severity is as follows: F0, absence of fibrosis; F1, Fibrous expansion of some portal areas, with or without short fibrous septa; F2, Fibrous expansion of most portal areas, with or without short fibrous septa; F3, Fibrous expansion of most portal areas with occasional portal to portal bridging; F4, Fibrous expansion of portal areas with marked bridging as well as portal to central; F5, marked bridging with occasional nodules (incomplete cirrhosis); F6, cirrhosis, probable or definite [12]. According to ISHAK fibrosis scoring, fibrosis was evaluated in two groups as F0-3 no/low grade fibrosis (=METAVIR F0-2) and F4-6 advanced fibrosis (=METAVIR F3-4) [13].
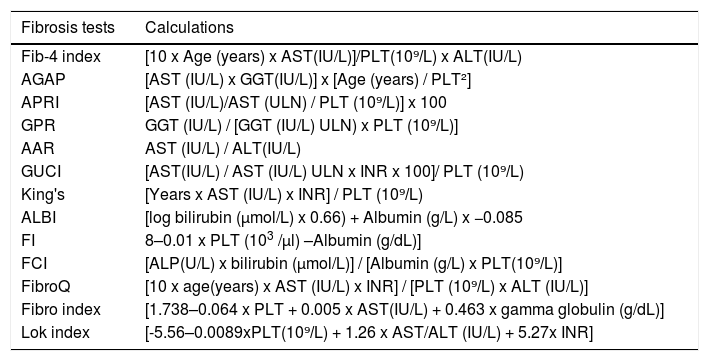
2.3Serum markers, new non-invasive fibrosis scoring method AGAP and othersWhen biopsy was performed, age, sex, alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma glutamyl transpeptidase (GGT), alkaline phosphatase (ALP), total bilirubin (TB), albumin, gamma globulin, platelet count (PLT), prothrombin time (PT), and international normalized ratio (INR) values of the patients were recorded. In addition, hepatitis B serological markers and serum HBV DNA were measured using COBAS AmpliPrep/COBAS TaqMan (CAP-CTM; Roche, Branchburg, NJ, USA) and the lower limit value was considered to be 20 IU/mL. In many studies, especially AST, GGT and PLT were widely used in non-invasive fibrosis scoring formulas. The formula of AGAP = [AST (IU/L) x GGT(IU/L)] x [Age (years) / PLT²] was developed by using these parameters. In this formula, a non-invasive scoring method, and compare it with other non-invasive fibrosis scores in patients with no/low grade and advanced fibrosis (Table 1).
Non invasive scores (14-17).
AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; GGT: Gamma glutamyl transpeptidase; ALP: Alkaline phosphatase; PLT: Platelet; INR: International normalized ratio; Fib-4: Fibrosis-4 index; APRI: AST/PLT ratio index; GPR: Gamma-glutamyl transpeptidase to platelet ratio; AAR: aspartate alanine aminotransferase ratio; AST/PLT ratio; GUCI:Goteborg University Cirrhosis Index; ALBI: Albumin-bilirubin score; FI: Fibrosis index; FCI: Fibrosis cirrhosis index; FibroQ: Fibroquotient; ULN; upper limit of normal.
The data obtained in our study was loaded to the SPSS 22.0 statistical program (SPSS Inc. Chicago, IL, USA) for the statistical analysis, and Kolmogorov-Smirnov Z test was used in order to select the correct test regarding the numerical data in the evaluation. The comparison of the two categories in the variables suitable for normal distribution found as a result of the test was carried out with Independent Sample t Test, and the comparison of the two categories in variables that were not suitable for normal distribution as a result of the test was performed with the Mann-Whitney U Test. The cutoff values of non-invasive fibrosis markers in the determined groups were calculated by ROC Analysis. The superiority of non-invasive fibrosis markers over each other was demonstrated by calculating Accuracy, LR +, LR-, PPV and NPV statistics with the values obtained as a result of the analysis. The examination of the differences of categorical variables was performed with the help of Chi-Square test. All analyzes were interpreted at p<0.05 significance level.
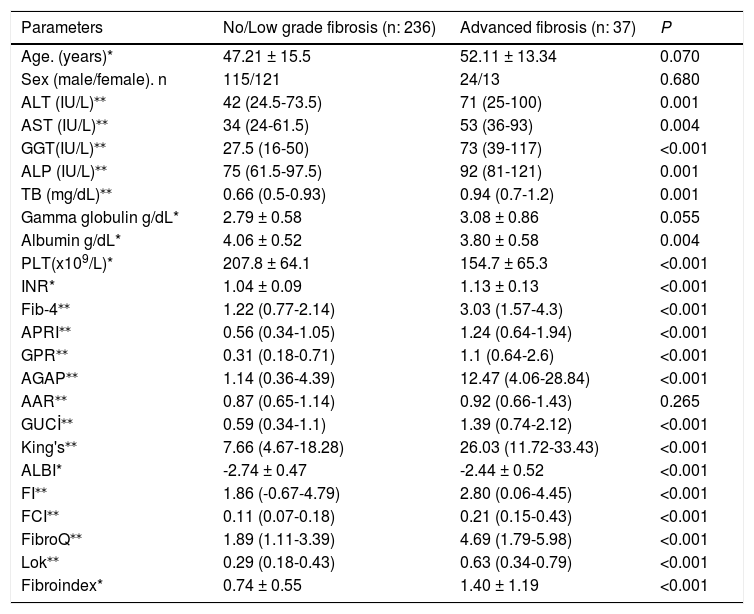
3Results3.1Patients characteristicA total number of 273 patients who underwent liver biopsy from February, 2007 to February, 2019 were included in our study. Histologically, liver biopsies of these patients were divided into two groups as no/low grade and advanced fibrosis. Of the patients, 134 (49.1%) were female and 139 (50.9%) were male and there was no difference between the fibrosis groups in terms of sex (p=0.680). In addition, the mean age of the patients was 48.7±15.2. It was 47.2±15.5 and 52.1±13.3 in no/low grade and advanced fibrosis group, respectively. The mean age was no difference between the fibrosis groups in terms of age (p=0.07) (Table 2).
Demographic and clinical data and fibrosis score values between no/low grade and advanced fibrosis groups.
| Parameters | No/Low grade fibrosis (n: 236) | Advanced fibrosis (n: 37) | P |
|---|---|---|---|
| Age. (years)* | 47.21 ± 15.5 | 52.11 ± 13.34 | 0.070 |
| Sex (male/female). n | 115/121 | 24/13 | 0.680 |
| ALT (IU/L)⁎⁎ | 42 (24.5-73.5) | 71 (25-100) | 0.001 |
| AST (IU/L)⁎⁎ | 34 (24-61.5) | 53 (36-93) | 0.004 |
| GGT(IU/L)⁎⁎ | 27.5 (16-50) | 73 (39-117) | <0.001 |
| ALP (IU/L)⁎⁎ | 75 (61.5-97.5) | 92 (81-121) | 0.001 |
| TB (mg/dL)⁎⁎ | 0.66 (0.5-0.93) | 0.94 (0.7-1.2) | 0.001 |
| Gamma globulin g/dL* | 2.79 ± 0.58 | 3.08 ± 0.86 | 0.055 |
| Albumin g/dL* | 4.06 ± 0.52 | 3.80 ± 0.58 | 0.004 |
| PLT(x109/L)* | 207.8 ± 64.1 | 154.7 ± 65.3 | <0.001 |
| INR* | 1.04 ± 0.09 | 1.13 ± 0.13 | <0.001 |
| Fib-4⁎⁎ | 1.22 (0.77-2.14) | 3.03 (1.57-4.3) | <0.001 |
| APRI⁎⁎ | 0.56 (0.34-1.05) | 1.24 (0.64-1.94) | <0.001 |
| GPR⁎⁎ | 0.31 (0.18-0.71) | 1.1 (0.64-2.6) | <0.001 |
| AGAP⁎⁎ | 1.14 (0.36-4.39) | 12.47 (4.06-28.84) | <0.001 |
| AAR⁎⁎ | 0.87 (0.65-1.14) | 0.92 (0.66-1.43) | 0.265 |
| GUCİ⁎⁎ | 0.59 (0.34-1.1) | 1.39 (0.74-2.12) | <0.001 |
| King's⁎⁎ | 7.66 (4.67-18.28) | 26.03 (11.72-33.43) | <0.001 |
| ALBI* | -2.74 ± 0.47 | -2.44 ± 0.52 | <0.001 |
| FI⁎⁎ | 1.86 (-0.67-4.79) | 2.80 (0.06-4.45) | <0.001 |
| FCI⁎⁎ | 0.11 (0.07-0.18) | 0.21 (0.15-0.43) | <0.001 |
| FibroQ⁎⁎ | 1.89 (1.11-3.39) | 4.69 (1.79-5.98) | <0.001 |
| Lok⁎⁎ | 0.29 (0.18-0.43) | 0.63 (0.34-0.79) | <0.001 |
| Fibroindex* | 0.74 ± 0.55 | 1.40 ± 1.19 | <0.001 |
ALT: Alanine aminotransferase. AST: Aspartate aminotransferase. GGT: Gamma-glutamyl transpeptidase. ALP: Alkaline phosphatase. TB: total biluribin. PLT:platelet. INR: International normalised ratio. Fib-4: Fibrosis-4 index. APRI: Aspartate aminotransferase to platelets ratio. GPR: Gamma-glutamyl transpeptidase to platelet ratio; AAR: Aspartate alanine aminotransferase ratio. GUCI: Goteborg University Cirrhosis Index. ALBI: Albumin. bilirubin index. FibroQ: Fibrosis quotient. FI: Fibrosis index. FCİ: Fibrosis cirrhosis index.
Among the laboratory values, ALT, AST, GGT, ALP, TB, PLT, INR, gamma globulin and albumin were significantly higher in the advanced fibrosis group compared to no/low grade fibrosis group (p<0.05) (Table 2). Non-invasive fibrosis scores; Fib-4, APRI, GPR, GUCI, King's, ALBI, FCI, FI, FibroQ, Lok and Fibroindex values that are evaluated in many studies in the literature were found to be significantly higher in the advanced fibrosis group compared to the no/low grade fibrosis group (p<0.001), however, there was no significant difference between the groups in terms of AAR values (p=0.265) The AGAP score that we developed was significantly higher in the advanced fibrosis group compared to no/low grade fibrosis group (p<0.001) (Table 2).
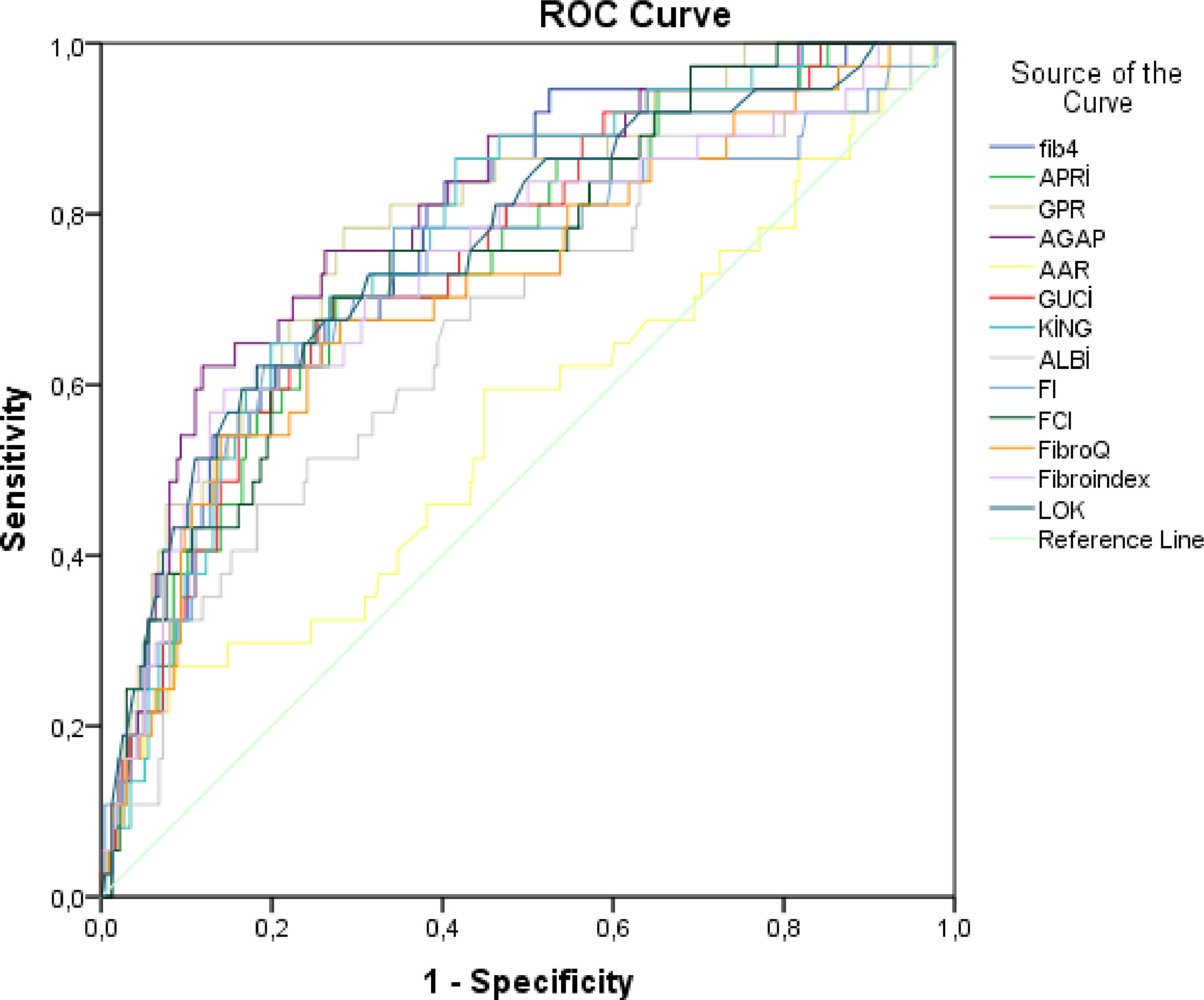
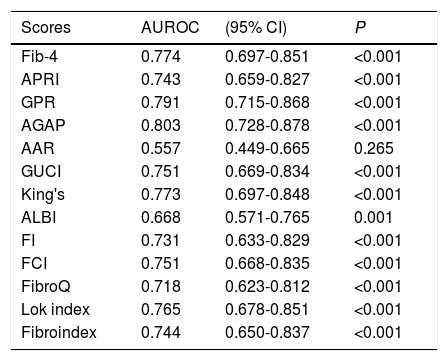
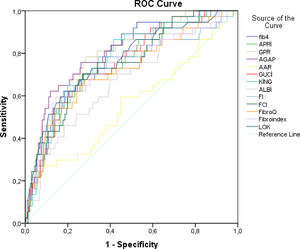
3.3Comparison of AUROC values between no/low grade and advanced Fibrosis groupsAGAP, a non-invasive fibrosis score, that we developed was found to have the highest AUROC value in ROC analysis compared to other scores [AUROC=0.803 (95% CI: 0.728-0.878); P<0.001]. After the AGAP score, GPR, Fib-4 and King's (0.791, 0.774 and 0.773, respectively; P <0.001) scores were detected to have the best AUROC values. Other non-invasive scores; APRI, GUCI, ALBI, FI, FCI, FibroQ, Lok and Fibroindex were statistically significant to predict advanced fibrosis (p<0.001). However, there was no significant difference between AAR score in no/low grade fibrosis and advanced fibrosis groups (p=0.265) (Table 3). Comparison of ROC curves has been shown for the diagnostic precision of Fib-4, APRI, GPR, AGAP, AAR, GUCI, King's, ALBI, FI, FCI, FibroQ, Lok and Fibroindex between no/low grade fibrosis and advanced fibrosis groups in chronic hepatitis B patients (Figure 1).
Areas under the curve of noninvasive scoring.
Fib-4: Fibrosis-4 index. APRI: Aspartate aminotransferase to platelets ratio. GPR: Gamma-glutamyl transpeptidase to platelet ratio; AAR: Aspartate aminotransferase. GUCI: Goteborg University Cirrhosis Index. ALBI: Albumin. bilirubin index. FibroQ: Fibrosis quotient. FI: Fibrosis index. FCİ: Fibrosis cirrhosis index.
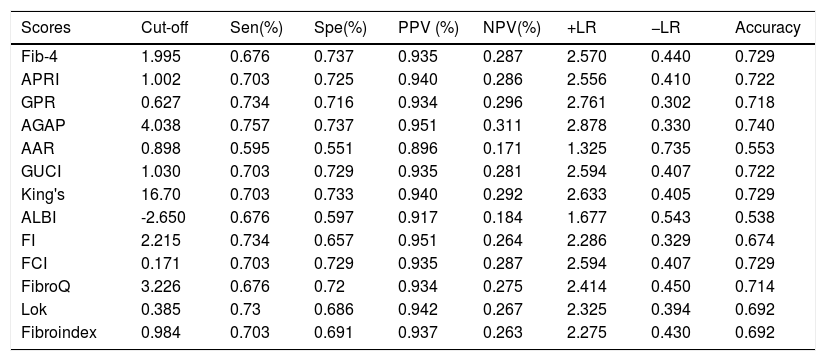
Threshold values for non-invasive fibrosis scores are presented in Table 4. Cut-off values for Fib-4, APRI, GPR, AGAP, AAR, GUCI, King's, ALBI, FI, FCI, FibroQ, Lok and Fibroindex scoring methods were found to be 1.995, 1.002, 0.627, 4.038, 0.898, 1.030, 16.700, -2.650, 2.215, 0.171, 3.226, 0.385 and 0.984, respectively. In our study, AGAP, which is a new scoring method, had the highest sensitivity and specificity (75.7% and 73.7%), whereas, the AAR score was the lowest (59.5% and 55.1%). The sensitivity and specificity of the other non-invasive fibrosis scoring methods such as Fib-4, APRI, GPR, GUCI, King's, ALBI, FI, FCI, FibroQ, Lok and Fibroindex were found to be (67.6% and 73.7%), (70.3% and 72.5%), (73.4% and 71.6%), (70.3% and 72.9%), (70.3% and 73.3%), (67.6% and 59.7%), (73.4% and 65.7%), (70.3% and 72.9%), (67.6% and 72%), (73% and 68.6%) and (70.3% and 69.1%), respectively. After this new AGAP score, the GPR, King's and Fib-4 scores were observed to perform well. When the positive and negative predictive values of non-invasive fibrosis scores were examined, the AGAP score had the highest (95.1% and 31.1%, respectively), while the AAR score had the lowest value (89.6% and 17.1%, respectively). In addition, among these scoring methods, the AGAP score had the highest diagnostic accuracy rate with a value of 0.740. This accuracy rate was followed by Fib-4, FCI and APRI scores (0.729, 0.729 and 0.722, respectively).
Performances of non-invasive fibrosis scores according to threshold values.
Fib-4: Fibrosis-4 index. APRI: Aspartate aminotransferase to platelets ratio. GPR: Gamma-glutamyl transpeptidase to platelet ratio; AAR: Aspartate aminotransferase. GUCI: Goteborg University Cirrhosis Index. ALBI: Albumin. bilirubin index. FibroQ: Fibrosis quotient. FI: Fibrosis index. FCI: Fibrosis cirrhosis index. Sen: sensitivity. Spe: specificity. PPV: positive predictive value. NPV: negative predictive value. +LR: positive likelihood ratio. −LR: negative likelihood ratio.
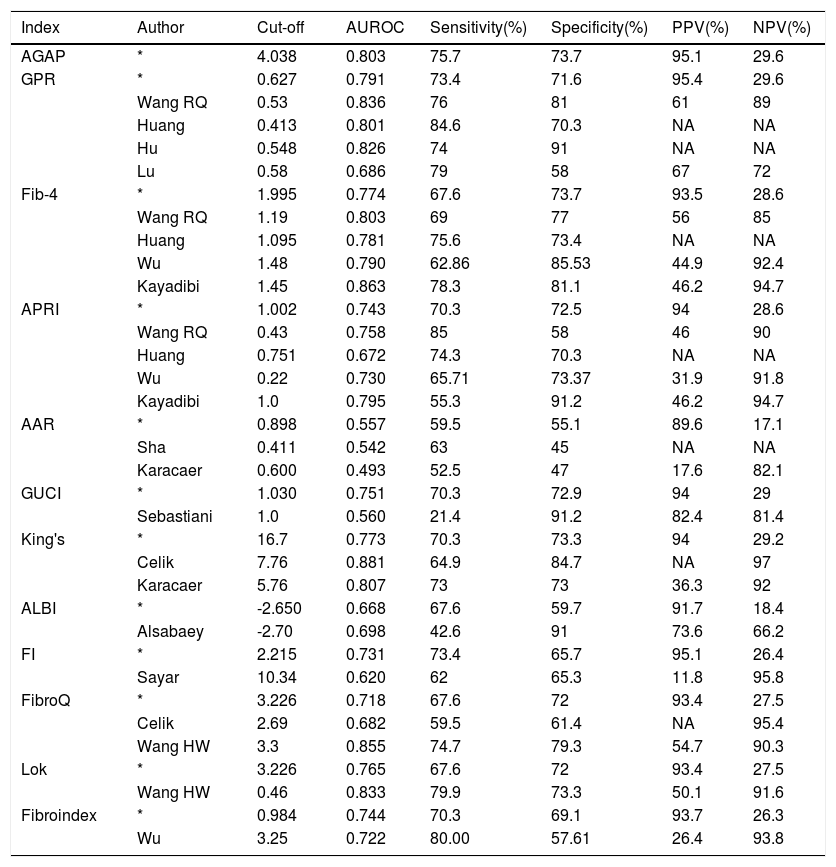
The comparison of the AUROC, cut-off, sensitivity, specificity, PPV and NPV values of the noninvasive fibrosis scores evaluated in our study with the current studies in the literature are presented in Table 5.
Comparison of the noninvasive fibrosis scores in detecting advanced fibrosis.
| Index | Author | Cut-off | AUROC | Sensitivity(%) | Specificity(%) | PPV(%) | NPV(%) |
|---|---|---|---|---|---|---|---|
| AGAP | * | 4.038 | 0.803 | 75.7 | 73.7 | 95.1 | 29.6 |
| GPR | * | 0.627 | 0.791 | 73.4 | 71.6 | 95.4 | 29.6 |
| Wang RQ | 0.53 | 0.836 | 76 | 81 | 61 | 89 | |
| Huang | 0.413 | 0.801 | 84.6 | 70.3 | NA | NA | |
| Hu | 0.548 | 0.826 | 74 | 91 | NA | NA | |
| Lu | 0.58 | 0.686 | 79 | 58 | 67 | 72 | |
| Fib-4 | * | 1.995 | 0.774 | 67.6 | 73.7 | 93.5 | 28.6 |
| Wang RQ | 1.19 | 0.803 | 69 | 77 | 56 | 85 | |
| Huang | 1.095 | 0.781 | 75.6 | 73.4 | NA | NA | |
| Wu | 1.48 | 0.790 | 62.86 | 85.53 | 44.9 | 92.4 | |
| Kayadibi | 1.45 | 0.863 | 78.3 | 81.1 | 46.2 | 94.7 | |
| APRI | * | 1.002 | 0.743 | 70.3 | 72.5 | 94 | 28.6 |
| Wang RQ | 0.43 | 0.758 | 85 | 58 | 46 | 90 | |
| Huang | 0.751 | 0.672 | 74.3 | 70.3 | NA | NA | |
| Wu | 0.22 | 0.730 | 65.71 | 73.37 | 31.9 | 91.8 | |
| Kayadibi | 1.0 | 0.795 | 55.3 | 91.2 | 46.2 | 94.7 | |
| AAR | * | 0.898 | 0.557 | 59.5 | 55.1 | 89.6 | 17.1 |
| Sha | 0.411 | 0.542 | 63 | 45 | NA | NA | |
| Karacaer | 0.600 | 0.493 | 52.5 | 47 | 17.6 | 82.1 | |
| GUCI | * | 1.030 | 0.751 | 70.3 | 72.9 | 94 | 29 |
| Sebastiani | 1.0 | 0.560 | 21.4 | 91.2 | 82.4 | 81.4 | |
| King's | * | 16.7 | 0.773 | 70.3 | 73.3 | 94 | 29.2 |
| Celik | 7.76 | 0.881 | 64.9 | 84.7 | NA | 97 | |
| Karacaer | 5.76 | 0.807 | 73 | 73 | 36.3 | 92 | |
| ALBI | * | -2.650 | 0.668 | 67.6 | 59.7 | 91.7 | 18.4 |
| Alsabaey | -2.70 | 0.698 | 42.6 | 91 | 73.6 | 66.2 | |
| FI | * | 2.215 | 0.731 | 73.4 | 65.7 | 95.1 | 26.4 |
| Sayar | 10.34 | 0.620 | 62 | 65.3 | 11.8 | 95.8 | |
| FibroQ | * | 3.226 | 0.718 | 67.6 | 72 | 93.4 | 27.5 |
| Celik | 2.69 | 0.682 | 59.5 | 61.4 | NA | 95.4 | |
| Wang HW | 3.3 | 0.855 | 74.7 | 79.3 | 54.7 | 90.3 | |
| Lok | * | 3.226 | 0.765 | 67.6 | 72 | 93.4 | 27.5 |
| Wang HW | 0.46 | 0.833 | 79.9 | 73.3 | 50.1 | 91.6 | |
| Fibroindex | * | 0.984 | 0.744 | 70.3 | 69.1 | 93.7 | 26.3 |
| Wu | 3.25 | 0.722 | 80.00 | 57.61 | 26.4 | 93.8 |
Results of the present study. Fib-4: Fibrosis-4 index. APRI: Aspartate aminotransferase to platelets ratio. GPR: Gamma-glutamyl transpeptidase to platelet ratio; AAR: Aspartate alanine aminotransferase ratio. GUCI: Goteborg University Cirrhosis Index. ALBI: Albumin bilirubin index. FibroQ: Fibrosis quotient. FI: Fibrosis index. Se: sensitivity. Sp: specificity. PPV: positive predictive value. NPV: negative predictive value. +LR: positive likelihood ratio. −LR: negative likelihood ratio. NA: not available.
Liver fibrosis is extremely important in treatment and in terms of complications in patients with CHB. Although liver biopsy is the gold standard for evaluating liver fibrosis, invasive intervention that may cause serious complications, high cost and limitations such as the heterogeneous distribution of histopathological changes within the parenchyma have led to the search for alternative methods. Therefore, non-invasive, simple and inexpensive scoring methods have been developed to evaluate fibrosis in patients with CHB. The 2015 WHO guideline recommends some non-invasive fibrosis markers such as APRI and Fib-4 in the evaluation of fibrosis in patients with CHB, however, their diagnostic values are still controversial [14]. In our study, we divided 273 patients with CHB who underwent liver biopsy into no/low grade and advanced fibrosis groups in order to determine a new scoring method for advanced fibrosis detection. For this purpose, we planned a retrospective study comparing 12 non-invasive serum markers used practically in the evaluation of liver fibrosis in patients with CHB and the new AGAP score that we developed.
According to the results of ROC analysis in our study, while non-invasive fibrosis scoring methods; Fib-4, APRI, GPR, AGAP, GUCI, King's, ALBI, FI, FCI, FibroQ, Lok and Fibroindex were successful in the differentiation of advanced and no/low grade fibrosis, the AAR score was unsuccessful. In our study, the highest AUROC value was observed in the AGAP score (0.803, P<0.001) and then in GPR, Fib-4 and APRI scores (0.791, 0.774, and 0.743 respectively P<0.001) and the lowest value was observed in AAR score (0.557, P=0.265). In the study carried out by Wang et al., the AUROC values of GPR, Fib4 and APRI scores between the groups of METAVIR F0-2 and F3-4 were 0.836, 0.803 and 0.758, respectively (P<0.001) [15]. The AUROC values of GPR, Fib-4 and APRI scores in previous studies are similar to those of our study, and the highest AUROC value among these is that of GPR [15-18]. There was no significant difference in AUROC value compared to the AAR score, advanced fibrosis, no / low grade fibrosis group as in our study [19,20]. According to our study, GUCI and King's scores could be used in the differentiation of advanced fibrosis and mild fibrosis in chronic hepatitis B patients and were found to be significant (AUROC values were 0.751 and 0.773 respectively). In the studies conducted, there was a significant difference in GUCI and King's scores in terms of AUROC value compared to advanced fibrosis and no / low grade fibrosis group [20-22]. In our study, the AUROC values of ALBI, FI, FibroQ and Lok scores were found 0.668, 0.731, 0.718 and 0.765, respectively. In studies published, ALBI, FI, FibroQ and Lok scores were found to be significant and to have AUROC values similar to our study compared to advanced fibrosis, no / low grade fibrosis group [22-26]. In our study, the AUROC values of Fibro index was found to be 0.7644, and the AUROC value was 0.722 (p<0.001) in the study by Wu et al [16].
According to our study, the AGAP score with cut-off value of 4.038, and sensitivity, specificity and accuracy values of 75.7%, 73.7% and 0.740, respectively, was the scoring method with the highest sensitivity among the non-invasive fibrosis scores. Cut-off values for non-invasive fibrosis scores; Fib-4, APRI and GPR were 1.995, 1.002 and 0.627, respectively and their sensitivity, specificity and accuracy values were (67.6%, 73.7%, 72.9%), (70.3%, 72.5%, 72.2%) and (73.4%, 71.6%, 71.8%), respectively. In the studies published, cut-off values for Fib-4, APRI ve GPR were similar to the values that we found in our study, with alternating rates of 1.48 - 1.45, 0.75-1.0 and 0.41-0.53 respectively. In addition, the values of sensitivity and specifity are similar to our study [15-17,27]. In our study, the cut-off values for GUCI, ALBI and FibroQ scores were 1.030, -2.650 and 3.226, respectively, and the sensitivity and specificity were found to be 70.3% and 72.9%, 67.6% and 59.7%, and 67.6% and 72%, respectively. In previous studies, the cut-off values of 1.0, -2.7, 2.69-3.3 for the GUCI, ALBI and FibroQ scores were similar to the values in our study, but the sensitivity values were low [21-23,26]. In our study, the cut-off values of King's and Lok scores were 16.7 and 0.385. In the studies conducted, the cut-off values for both King's and Lok scores were 5.76-7.76 and 0.46, respectively, and were lower compared to the results of our study. However, the sensitivity and specificity values of these scores were similar to our study [20,22,26]. The cut-off values for FI and Fibroindex in our study were 2.215 and 0.984. The cut-off values were 10.34 and 3.25 in previous studies and were higher than our study, but their sensitivity and specificity values were similar [16,25]. In our study, from non-invasive fibrosis scores, FCI AUROC value was 0.751, cut-off values were 0.171 and the sensitivity and specificity were 70.3% and 72.9%, respectively. There was a significant difference between the advanced fibrosis and no/low grade fibrosis group.
In our study, the AUROC values of FCI score was 0.751 and the cut-off value, sensitivity and specificity were 0.171, 70.3%, 72.9%, respectively, but in the literature, there was no study comparing advanced fibrosis and no/low grade fibrosis groups in patients with chronic hepatitis B. Instead, there was a significant difference in the literature on patients with chronic hepatitis C compared to the advanced fibrosis and no/low grade fibrosis group [28].
5ConclusionIn our study, non-invasive fibrosis markers; Fib-4, APRI, GPR, AGAP, GUCI, KING, ALBI, FI, FCI, FibroQ, Lok and Fibroindex were shown to be successful in the differentiation of advanced fibrosis in patients with CHB. However, the other score, AAR, was found to be unsuccessful in detecting fibrosis. In our study, the most successful of the 12 scores used in the differentiation of fibrosis was the AGAP score that we developed. The AUROC value, sensitivity and specificity, positive predictive and negative predictive values and accuracy rates of this score were very successful compared to other scores. However, more extensive and detailed studies are needed regarding these scores. This AGAP score that we developed is quite sensitive, simple and has a low-cost in differentiation of advanced fibrosis in patients with CHB.
Author contributionsAll authors have contributed to the reporting of the work described in the article.