Hepatitis A virus (HAV) is the most common cause of acute viral hepatitis in the world. Rarely, acute infection may persist for a long time. Autoimmune hepatitis (AIH) may provide anti-HAV IgM positivity detection for a prolonged time. On the other hand, HAV as an infectious agent may also trigger AIH. Here we presented a case which seemed like a simple acute viral hepatitis A infection at the beginning but turned out to be an AIH according to the International Autoimmune Hepatitis Group’s system. A 21-year-old female was diagnosed as symptomatic acute HAV infection with anti-HAV IgM positivity and elevated aminotransferase levels. The other viral serological tests were negative. On the 6th, 12th and 18th months of the follow up, her anti-HAV IgM positivity still continued and transaminase levels were also 3 to 7 times high of the upper limit of normal. In addition, antinuclear antibody was positive. However, on the 19th month anti-HAV IgM could be detected as negative. Liver histology was prominent. The patient had a score of 16 according to the International Autoimmune Hepatitis Group’s system. She was given prednisolone (10 mg/day) and azathioprine (100 mg/day). The aminotransferase levels were detected within normal ranges at the end of the first month of therapy. She was in remission during follow up for 6 years. In conclusion, prolonged HAV infection and AIH may not only trigger each other but also deteriorate the liver histology. AIH should be investigated in cases of long-lasting HAV infection in order to begin the treatment earlier. On the other hand, AIH patients should also be vaccinated for both HBV and HAV to avoid more severe diseases.
Hepatitis A virus (HAV) is an enteric transmitting virus and is the most common cause of acute viral hepatitis worldwide.1 Generally, in childhood, the infection is asymptomatic or unicteric but in adults, it is often more severe. Acute hepatitis can be diagnosed by the detection of the immunoglobulin M antibody against HAV (Anti-HAV IgM) in patients who have the clinical features of hepatitis. It is reported that, in male patients, anti-HAV IgM persists significantly longer in acute phase of disease.2 Autoimmune hepatitis (AIH) is another factor that causes prolonged stage of anti-HAV IgM positivity. In the literature, there are only a few AIH cases with prolonged anti-HAV IgM positivity.3-7
AIH is a rare disease with unknown etiology which causes chronic necroinflammatory changes in the liver. The exact molecular, cellular, pathologic and physiological mechanisms leading to autoimmunity are still incompletely explained. Infectious agents like hepatitis viruses, on the other hand, have often been named as triggers of autoimmune diseases. Hepatitis C virus has existed with AIH more than other hepatitis viruses.8 Viral proteins of the viruses may be similar to the amino acid chain of different autoantigens in the liver. Therefore, cross immune reactions to viral proteins may also cause the damage in liver tissue at the same time.9,10 Here we presented a case of AIH following acute HAV infection with prolonged anti-HAV IgM positivity.
CaseA 21-year-old female was admitted with fever, weakness, myalgia, and jaundice. She had no prior history of alcohol or substance abuse. She has no family history of liver disease. Her physical examination revealed jaundice and a tender hepatomegaly of 2 cm below costal margin. Her laboratory findings were as follows: Hct 37%, Hb 12.2 g/dl, WBC 9,200/mm3, platelets 170,000/mm3, ESR 90 mm/h, AST 435 U/L, ALT 948 U/L, alkaline phosphatase (ALP) 469 U/L, total bilirubin 4.1 mg/dL, direct bilirubin 2.5 mg/dL, albumin 3.5 g/dL, globulin 4.8 g/dL, PT 11.6 sec, INR 1.02, serum iron 57 • g/dL (N: 60-150), iron binding capacity 434 • g/dL (N: 250400), ferritin 38 ng/dL (N: 5-96). Serum anti-HAV IgM was positive. HBsAg, anti-HBs, anti-HBc IgM, anti-HCV and anti-HAV IgG were negative. An upper transabdominal ultrasound examination revealed hepatomegaly and a hilar lymph node (9.5 mm). After a symptomatical treatment the patient was discharged on the 6th hospitalization day with AST: 51 U/L, ALT: 115 U/L and her PT and bilirubin levels were normal.
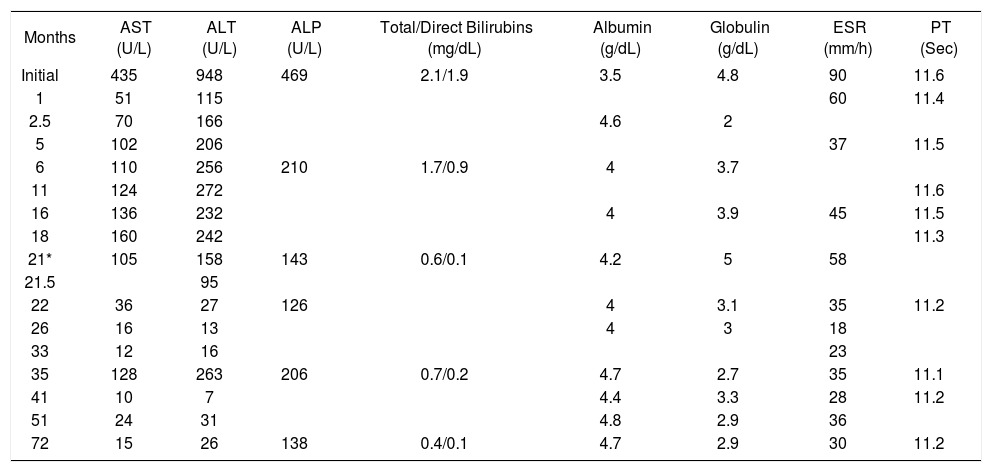
On the 6th, 12th and 18th months of the follow up, her serum anti-HAV IgM persisted as still positive. Her transaminase levels were also 3 to 7 times high of the upper limit of normal (Table I). Her antinuclear antibody was positive while anti-smooth muscle antibody and anti-liver kidney microsomal antibody tests were negative. Ceruloplasmin and ferritin levels were within normal limits. An abdominal computed tomography was normal except for mild hepatomegaly. On the 19th month of follow up, she was hospitalized again for weakness and arthralgias. Anti-HAV IgM could be detected negative, serum aminotransferase levels were still high (AST: 105 U/L, ALT: 158 U/L) and virological tests for hepatitis B and C were negative again. A liver biopsy was performed and indicated chronic hepatitis with HAI: 9 (Lobular degeneration and necrosis: 3, periportal piece meal necrosis: 3, and portal mononuclear cell infiltration: 3) and fibrosis: 3 scores. The patient had a score of 16 according to the International Autoimmune Hepatitis Group’s system. As a result, the patient was diagnosed as AIH. Her HLA analysis revealed the following results: A1 A24(9) B8B35 DR1DR11(5)DQ6(1)DQ7(3). She was given prednisolone (10 mg/day) and azathio-prine (100 mg/day). The liver aminotransferase levels were detected within normal ranges at the end of the first month of therapy. Because of the acne and hirsutism, prednisolone dose was decreased to 5 mg/day on the 5th month of the therapy. The patient’s last relapse was detected 2 years ago. She has been followed up in remission for 7 years.
Laboratory parameters of the patient on follow up.
| Months | AST (U/L) | ALT (U/L) | ALP (U/L) | Total/Direct Bilirubins (mg/dL) | Albumin (g/dL) | Globulin (g/dL) | ESR (mm/h) | PT (Sec) |
|---|---|---|---|---|---|---|---|---|
| Initial | 435 | 948 | 469 | 2.1/1.9 | 3.5 | 4.8 | 90 | 11.6 |
| 1 | 51 | 115 | 60 | 11.4 | ||||
| 2.5 | 70 | 166 | 4.6 | 2 | ||||
| 5 | 102 | 206 | 37 | 11.5 | ||||
| 6 | 110 | 256 | 210 | 1.7/0.9 | 4 | 3.7 | ||
| 11 | 124 | 272 | 11.6 | |||||
| 16 | 136 | 232 | 4 | 3.9 | 45 | 11.5 | ||
| 18 | 160 | 242 | 11.3 | |||||
| 21* | 105 | 158 | 143 | 0.6/0.1 | 4.2 | 5 | 58 | |
| 21.5 | 95 | |||||||
| 22 | 36 | 27 | 126 | 4 | 3.1 | 35 | 11.2 | |
| 26 | 16 | 13 | 4 | 3 | 18 | |||
| 33 | 12 | 16 | 23 | |||||
| 35 | 128 | 263 | 206 | 0.7/0.2 | 4.7 | 2.7 | 35 | 11.1 |
| 41 | 10 | 7 | 4.4 | 3.3 | 28 | 11.2 | ||
| 51 | 24 | 31 | 4.8 | 2.9 | 36 | |||
| 72 | 15 | 26 | 138 | 0.4/0.1 | 4.7 | 2.9 | 30 | 11.2 |
ALP: alkaline phosphatase, ESR: erythrocyte sedimentation rate, PT: prothrombin time. 12/8/2001*: The date, she was given 10 mg/day prednisolone and 100 mg/day azathioprine.
Hepatitis A virus infection is mostly a self-limited disease with patients having a complete recovery nearly after 3 months. Some atypical manifestations of HAV such as hemolysis, acalculous cholecystitis, prolonged cholestasis and acute renal failure were noted.11 However, prolonged anti-HAV IgM positivity with a high aminotransferase activity is a very rare clinical condition and especially seen in men.2 On the other hand, AIH is a rare disease with unknown etiology with a strong female predominance.12 In rare patients with chronic liver disease following acute hepatitis A, the disease in fact is AIH type 1 and it strongly indicates that HAV infection can act as trigger for this organ-specific autoimmune disease in predisposed individuals.12
In our case, whether AIH is triggered by HAV infection or previous AIH caused a prolonged stage of the HAV infection is a dilemma.
There have not been enough series of observed patients for a certain decision, so we can speculate both of the assumptions. HAV infection is probably one of the several triggers that may induce autoimmune hepatitis. Even, our patient did not recover within 18 moths which means that her prolonged HAV infection may have powered the triggering of autoimmune hepatitis. Some reported cases support the possibility of the former assumption.3-7
On the other hand, if the patient had AIH before the HAV infection, HAV would have worsened the liver histology dramatically. Our patient had a stage 3 fibrosis that makes the latter assumption also logical. In this respect, we may speculate that autoimmune hepatitis worsens the HAV infection progression and HAV may cause a chronic, deteriorating active hepatitis in AIH patients.
Vaccination of HAV is recommended worldwide for patients with chronic liver disease to prevent decompensation due to superinfection with HAV. In addition to that, combined hepatitis A/B vaccination is both safe and highly immunogenic against HAV and HBV in HCV-infected patients with well compensated liver disease.13 Patients with AIH are also a group at risk for disease exacerbation or relapse of the hepatitis A or B. Therefore, this group of people should be protected against both HAV and HBV by vaccination.
Among South American children, HLA DR13 allele is a risk factor for protracted liver damage after HAV infection (14). Because our patient has lack of HLA DR13, any of her HLA allele may be in charge in the prolonged disease survey.
In conclusion, our case is an example for a HAV vs AIH relationship. Since this association deteriorates the liver histology, we recommend that AIH should be investigated in cases of long-lasting liver disease after HAV infection to start the treatment earlier. With another perspective, AIH patients should also be vaccinated for not alone HBV but HAV to avoid more severe disease.