A 69-year-old man with hypertension, mild (stage II) chronic kidney disease and uncomplicated type B aortic dissection presented to the emergency service with a 2-week history of colicky upper abdominal pain and nausea. His symptoms had progressively worsened with shortness of breath that was exacerbated with activity.
At presentation, he denied fever, vomiting or weight loss. The patient appeared uncomfortable. Upon physical examination, his abdomen was distended, the right hypochondrium revealed mild tenderness with tympanic percussion tones. Laboratory investigations were noncontributory with the exception of a mild leukocytosis of 10,900/iT and elevated ESR of 23 mm/h.
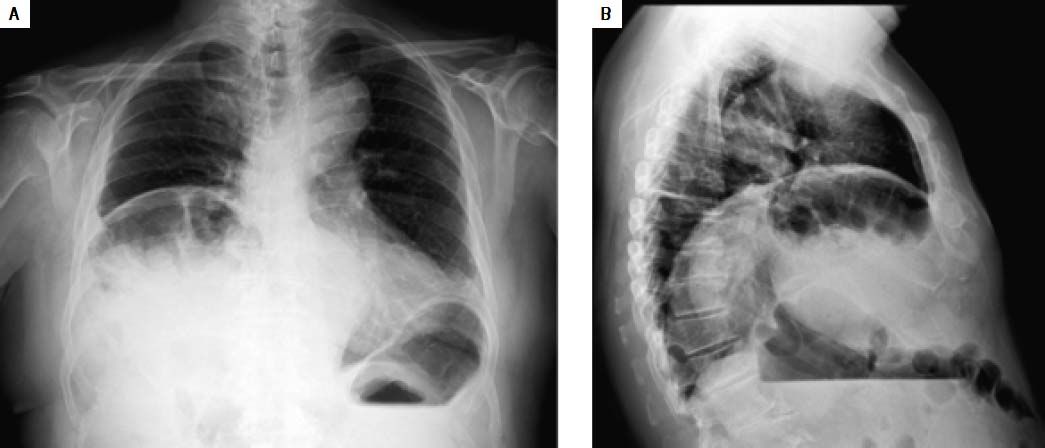
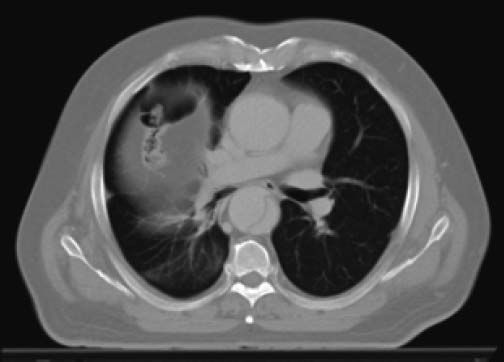
A chest radiograph was obtained (Figure 1). It suggested the presence of an air-filled distended bowel tract within the right subphrenic space, with the superior liver profile depressed below the level of the left hemidiaphragm (Figure 1, panel A). Computed tomography (Figure 2) revealed no free air, confirming the presence of isolated pseudopneumoperitoneum, due to colonic interposition between the liver and diaphragm (Chilaiditi’s sign). The patient was treated conservatively and observed with analgesia, intravenous fluids and bowel decompression to which he responded favorably. He was well and discharged home 4 days later.
Demetrius Chilaiditi was the Greek radiologist who firstly described the radiographic features of colonic interposition between the liver and the diaphragm as incidental findings in three patients in 1910.1 This relatively rare condition is currently known as Chilaiditi’s syndrome when it causes symptoms.2–5 Associated with anatomic distortion due to congenital variation or functional disorders,2 Chilaiditi’s sign (or interpositio hepatodiaphragmatica) can be present permanently or sporadically2–3 and can be misleadingly interpreted as a sign of diaphragmatic hernia, subdia-phragmatic abscess or bowel perforation, possibly leading to unnecessary exploratory laparotomies.3 Given the presence of air under the hemidiaphragm, the differential diagnosis should consider primarily every potential cause of perforation of the abdominal viscus. Despite the presence of rugal folds within the gas can suggest colonic interposition, CT is frequently crucial to confirm or refute the diagnosis.
Generally, nearly all patients are successfully managed by medical treatment with bed rest, intravenous fluids and bowel decompression. Only occasionally, patients with recurrent presentation or evidence of vascular sufferance of the interposed bowel tract are offered surgical management.2–4 When surgery is indicated the operative procedure is almost unavoidably chosen on the basis of intraoperative findings.2 Ischemic bowel segments should be extirpated, especially in the case of colonic volvulus, being transverse or right colectomies the procedures performed more often. Alternatively, the anchoring of colonic portions (colopexy) or a displaced liver (hepatopexy) to the abdominal wall is generally deemed sufficient and effective.2,4,5