Background/Purpose. In Japan, acute liver failure (ALF) has generally been described using the diagnostic term, “fulminant hepatitis”, because of the fact that most cases of ALF has been thought to occur in association with hepatitis mainly due to a hepatitis virus infection. New diagnostic criteria for ALF, including ALF other than fulminant hepatitis, were established in 2011. We therefore examined the prognostic factors of patients with liver failure from a systemic cause, including warfarin users. Material and methods. Sixty-six patients with ALF that were diagnosed according to the Japanese diagnostic criteria for ALF between 2009 and 2013 were divided into a survivor group and a non-survivor group. The data regarding demography, liver tests, coagulation tests, Sequential Organ Failure Assessment (SOFA) scores, and the use of oral warfarin or aspirin were compared between the two groups. Results. The SOFA score was significantly higher in the non-survivor group (p = 0.025). The proportion of oral warfarin users was significantly higher in the survivor group (p = 0.013) (58.1% vs. 26.1%). A multivariate logistic regression analysis showed the SOFA score (odds ratio: 0.851, 95% confidence interval (CI): 0.728-0.995, p = 0.043) and warfarin use (odds ratio: 3.261, 95% CI: 1.028-10.347, p = 0.045) to be significant factors that were negatively and positively associated with the prognosis, respectively. Conclusion. In this study, among the patients with ALF other than fulminant hepatitis, those with a high SOFA score on admission exhibited a poor prognosis. In addition, oral warfarin use prior to disease onset was found to be a factor which indicated a good prognosis.
In Japan, most cases of acute liver failure (ALF) are thought to be due to hepatitis, primarily caused by viral infections; therefore, ALF has traditionally been represented by the diagnostic term, “fulminant hepatitis,” which includes cases of ALF resulting from viral hepatitis, drug allergies and acute-onset autoimmune hepatitis.1 Worldwide, however, ALF is generally considered to constitute a liver failure syndrome caused by any form of acute liver injury, regardless of the pathological mechanism.2 In order to adjust for this discrepancy, the Intractable Hepatobiliary Disease Study Group ofJapan established a new set of diagnostic criteria for ALF, which include cases of ALF other than fulminant hepatitis, in 2011.3 However, the clinical characteristics and prognosis of forms of ALF other than fulminant hepatitis remain unclear, as national surveys in Japan focused on fulminant hepatitis prior to 2011.
The diagnostic criteria for ALF are usually not applied in warfarin users because the prothrombin time is prolonged, regardless of the presence or absence of liver dysfunction, in such patients. However, ALF patients treated with warfarin should be precisely evaluated, as a substantial number of warfarin users have ALF due to the increasing number of patients with atherosclerotic and/or chronic heart disease.4
The present study aimed to elucidate prognostic factors among patients with liver failure from a systemic cause, including warfarin users, transported to our advanced critical care and emergency center.
Material and MethodsThe subjects included 66 patients with underlying diseases of internal medicine or acute poisoning who had been emergently transported to our advanced critical care and emergency center between January 2009 and December 2013. In addition, all subjects satisfied the diagnostic criteria for ALF in Japan (2011),3 excluding patients with fulminant hepatitis or cardiopulmonary arrest. In this study, hepatocellular injury was defined as an AST level of at least 200 IU/L or ALT level of at least 300 IU/L.5 The endpoint was the survival at 28 days from onset. Of the 66 patients, 43 survived and 23 had died by the time of the endpoint. The survivors and non-survivors were compared according to age at the time of emergency admission and the parameters observed on general laboratory tests, including the total bilirubin, AST, ALT, LDH, ammonia, prothrombin time-international normalized ratio (PTINR), anti-thrombin-III (AT-III) and fibrinogen values. In addition, the diagnostic criteria score for acute-phase disseminated intravascular coagulation (DIC) was calculated based on clinical findings and blood test results obtained at the time of emergency admission. The Sequential Organ Failure Assessment (SOFA) score was calculated as an index for multiple organ failure. The survival rate was compared between the patients who did and did not receive oral warfarin or aspirin. In 2011, the Intractable Hepato-biliary Disease Study Group of Japan developed a new set of diagnostic criteria for ALF, which include cases of ALF other than fulminant hepatitis. Patients showing prothrombin time values of 40% or less of the standardized values, or a PT-INR of 1.5 or higher due to severe liver damage within eight weeks of the onset of the symptoms are diagnosed as having ALF, where the liver function prior to the current onset of liver damage was estimated to be normal. ALF is classified into “ALF without hepatic coma” and “ALF with hepatic coma,” the latter is further classified into two sub-types, the “acute type” and the “subacute type”, in which a grade II or more severe hepatic coma develops within 10 days and between 11 and 56 days, respectively, after the onset of disease symptoms.3 In 2005, the Japanese Association of Acute Medicine established diagnostic criteria for acute-phase DIC after conducting a prospective, multicenter study. The four diagnostic items in this set of criteria include the systemic inflammatory response syndrome (SIRS) criteria score, platelet count, PT ratio (clotting time/normal value) and fibrinogen degradation product (FDP) level. A patient was diagnosed with DIC if the total score was four points or higher.6 In 1996, Vincent, et al. developed a method in which the SOFA score is used to evaluate the severity of dysfunction in six organ systems (respiratory, hepatic, renal, cardiovascular, coagulation, neurological). For the diagnosis, the SOFA score is determined using the following items, which are measurable in any institution, graded on a five-point scale: PaO2/FiO2, the bilirubin level, the serum creatinine level or urine output, mean arterial pressure or dose of administered catecholamine, platelet count and Glasgow Coma Scale (GCS).7
Statistical analysisContinuous variables with a normal distribution are expressed as the mean ± standard deviation, and the t-test was used for comparisons between the two groups. Variables with an unknown distribution are expressed as the median (range), and the Mann-Whitney U-test was used for comparisons between the two groups. The χ2 test for independence was used to test for differences in proportions. An examination was performed to evaluate the effects of various explanatory variables on the prognosis. The prognosis was used as the response variable, and all explanatory variables with a p value of < 0.1 in the univariate analysis were included in the multivariate logistic regression analysis (backward elimination likelihood ratio test). In addition, the presence or absence of heart failure was included as an explanatory variable in a multivariate analysis. The level of significance was set at 5%.
Ethical aspectsThis study was approved by the ethics committee of the School of Medicine at Iwate Medical University (approval number: H25-184) prior to study enrollment.
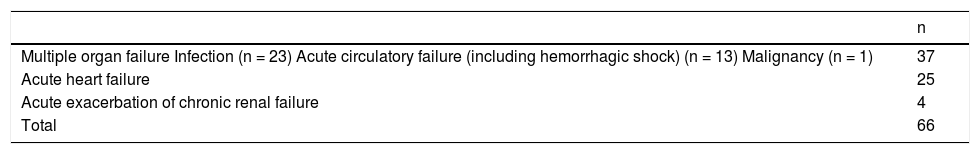
ResultsPatient background characteristicsThere were 48 males and 18 females, with a mean age of 70.0 years (range: 5 months to 100 years). The cause of ALF was multiple organ failure in 37 patients (infection in 23 patients, acute circulatory failure in 13 patients (including hemorrhagic shock) and a malignant tumor in one patient), heart failure in 25 patients and acute exacerbation of chronic renal failure in four patients (Table 1). A total of 31 patients were receiving oral warfarin and 14 patients were receiving oral aspirin at the time of admission. In the 31 patients who are on warfarin, six patients who died had discontinued warfarin, 24 patients who survived had continued after a transient discontinuation of few days and one patient who survived discontinued warfarin because of improved arrhythmia. On the other hand, in the 14 patients who were on aspirin, five patients who died had discontinued treatment and nine patients who survived had continued treatment.
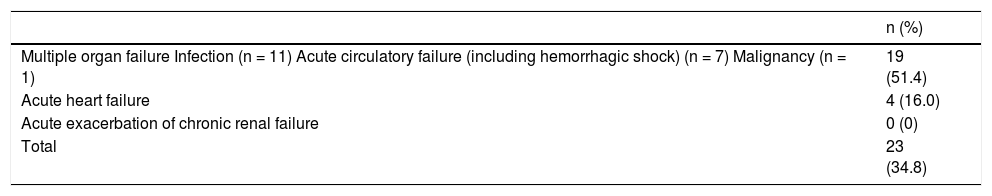
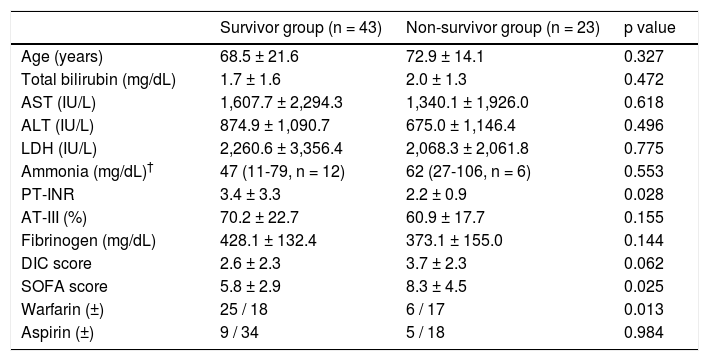
Prognosis and related factorsThe fatality rate was 34.8%. Among the 23 patients who died, the cause of death was multiple organ failure in 19 patients and heart failure in four patients (Table 2). Blood purification therapy was performed in 10 patients who survived and seven patients who eventually died, for a total of 17 patients (25.8%). There were no significant differences in age between the survivors and non-survivors. However, according to the laboratory test results, the mean PT-INR was 3.4 ± 3.3 in the survivors and 2.2 ± 0.9 in the non-survivors, indicating significantly higher values among the survivors (p = 0.028). There were no significant differences in the acute-phase DIC score between the two groups. However, the SOFA scores were significantly higher in the non-survivors, at 8.3 ± 4.5, compared with 5.8 ± 2.9 observed in the survivors (p = 0.025). There was also a significantly higher number of oral warfarin users among the survivors (p = 0.013); however, the two groups exhibited no significant differences in the number of patients using aspirin (Table 3).
Differences in clinical characteristics between the survivors and non-survivors.
| Survivor group (n = 43) | Non-survivor group (n = 23) | p value | |
|---|---|---|---|
| Age (years) | 68.5 ± 21.6 | 72.9 ± 14.1 | 0.327 |
| Total bilirubin (mg/dL) | 1.7 ± 1.6 | 2.0 ± 1.3 | 0.472 |
| AST (IU/L) | 1,607.7 ± 2,294.3 | 1,340.1 ± 1,926.0 | 0.618 |
| ALT (IU/L) | 874.9 ± 1,090.7 | 675.0 ± 1,146.4 | 0.496 |
| LDH (IU/L) | 2,260.6 ± 3,356.4 | 2,068.3 ± 2,061.8 | 0.775 |
| Ammonia (mg/dL)† | 47 (11-79, n = 12) | 62 (27-106, n = 6) | 0.553 |
| PT-INR | 3.4 ± 3.3 | 2.2 ± 0.9 | 0.028 |
| AT-III (%) | 70.2 ± 22.7 | 60.9 ± 17.7 | 0.155 |
| Fibrinogen (mg/dL) | 428.1 ± 132.4 | 373.1 ± 155.0 | 0.144 |
| DIC score | 2.6 ± 2.3 | 3.7 ± 2.3 | 0.062 |
| SOFA score | 5.8 ± 2.9 | 8.3 ± 4.5 | 0.025 |
| Warfarin (±) | 25 / 18 | 6 / 17 | 0.013 |
| Aspirin (±) | 9 / 34 | 5 / 18 | 0.984 |
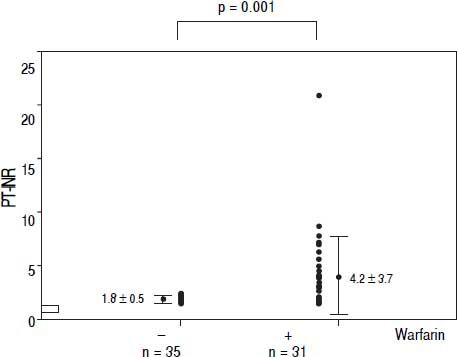
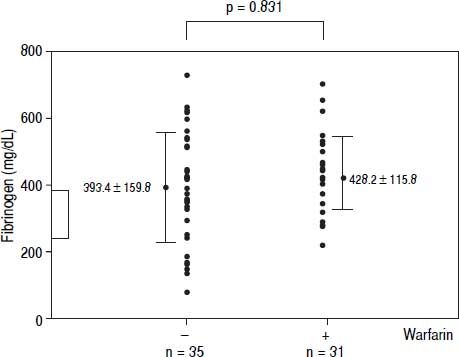
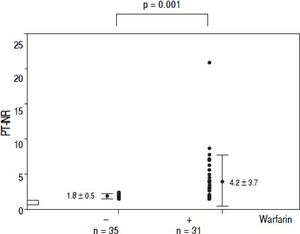
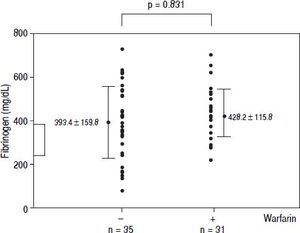
The coagulation parameters and survival rates were compared between the 31 patients who used oral warfarin and the 35 patients who did not. The mean PT-INR was 4.2 ± 3.7 and 1.8 ± 0.5 in the warfarin users and non-users, respectively, indicating higher values among the users (p = 0.001) (Figure 1). The mean fibrinogen level was 428.2 ± 115.8 mg/dL in the users and 393.4 ± 159.8 mg/dL in the non-users, with no significant differences (Figure 2). The warfarin users accounted for 32% of the patients whose cause of ALF was multiple organ failure and 60% of the patients whose cause was heart failure.
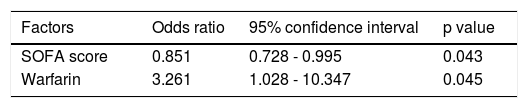
The prognosis was used as the response variable. The following explanatory variables with a p value of < 0.1 in the univariate analysis were included in the multivariate logistic regression analysis: PT-INR, DIC score, SOFA score and warfarin use. Consequently, the SOFA score [odds ratio: 0.851, 95% confidence interval (CI): 0.728-0.995, p = 0.043] and warfarin use (odds ratio: 3.261, 95% CI: 1.028-10.347, p = 0.045) were selected as significant factors associated with the prognosis (Table 4). We also examined whether warfarin use was an independent of cause of ALF by including the presence or absence of heart failure as an explanatory variable. As a result, heart failure (odds ratio: 0.257, 95% CI: 0.722-0.917, p = 0.036) and warfarin use (odds ratio: 0.296, 95% CI: 0.094-0.936, p = 0.038) were selected as independent prognostic factors.
DiscussionIn the 2011 criteria, liver failure from a systemic cause was newly added as a type of ALF. The present study examined the clinical characteristics and prognostic factors of patients with this newly added category of ALF. The results showed that patients with a high SOFA score at emergency admission have a poor prognosis. In contrast, ALF patients treated with oral warfarin have a good prognosis.
Cholongitas, et al. examined 125 patients with acetami-nophen-induced ALF and found the SOFA score to be the best prognostic indicator of the outcome. The authors reported that this finding was due to the fact the SOFA score reflects the presence of multiple organ dysfunction syndrome.8 Craig, et al. reported good prognosis associated with a SOFA score of least 7 during the first 96 h after acetaminophen overdose.9 Therefore, the SOFA score is useful as an early prognostic marker of ALF. In addition, total bilirubin is a component of ALF in the SOFA score and has low specificity for liver failure. Hence, Craig, et al. indicated that the total bilirubin level cannot be used to differentiate between patients with acute and chronic liver dysfunction.9 Previous studies have reported that ALF is the only component of the SOFA score that is not associated with the risk of mortality.10,11 The present study also found no significant differences in the total bilirubin levels between the survivors and the non-survivors. In addition, these two groups exhibited no significant differences in the level of ammonia, a causative agent of hepatic encephalopathy. Therefore, in case of ALF other than fulminant hepatitis, the prognosis is thought to be affected by factors other than the ALF component in the SOFA score.
The prothrombin time has long been used as an index of protein synthesis in the liver and is considered to be the most important index of the severity of liver failure. However, our study showed that patients with a high PT-INR have a good prognosis. The reason for this finding is thought to be due to the presence of a significantly high number of warfarin users among the survivors. Rake, et al. observed fibrin deposition in autopsy cases of viral fulminant hepatitis12 and proposed that extensive hepatic necrosis is caused by microcirculatory dysfunction due to the presence of coagulation in the hepatic sinusoids. Another study showed that the prognosis is improved by anticoagulant therapy associated with early heparin use.13 However, in ALF patients with decreased production of AT-III by hepatocytes, the effect of heparin is insufficient. Importantly, Fujiwara, et al. used an AT-III concentrate and successfully extended the survival period in patients with fulminant hepatitis.14 Meanwhile, Mochida, et al. used anticoagulation therapy consisting of an AT-III concentrate and synthetic protease inhibitor and reported improved signs of liver failure and coagulation disorders.15 As described above, anticoagulation therapy is thought to be useful for treating microcirculatory failure, a pathology of ALF.
Warfarin is an inhibitor of vitamin K and depletes vitamin-K-dependent coagulation factors II, VII, IX and X, thereby prolonging the clotting time. All clotting factors produced by hepatocytes, are depleted in patients with liver failure and then PT value exactly indicates the hepatic functional reserve.16,17 On the other hand, Bernuau, et al. showed that a decreased factor V level was the most sensitive indicator of liver failure.18 Factor V exactly reflects the liver synthetic function and is independent of vitamin K. However, because factor V measurement is very expensive and is not generally distributed in Japan, we could not measure factor V. On the other hand, PT (INR) is more commonly used as the marker for the severity of liver failure in Model for End-Stage Liver Disease (MELD) score, King’s college criteria, Child Pugh score, and American Association for the Study of Liver Diseases (AASLD) definition of acute liver failure,2,19–21 although it includes vitamin K-dependent factors. Therefore, we used PT-INR as the representative liver functional reserve and used fibrinogen as a marker of vitamin K-independent factor in this study. The results showed that the PT-INR values were significantly higher among the warfarin users than among the non-users. However, the fibrinogen levels did not differ between the groups, with a similar distribution. Therefore, no differences are believed to exist between warfarin users and non-users in terms of the severity of liver dysfunction (i.e., the ability to synthesize protein). Furthermore, in the present study, the SOFA score and warfarin use were selected as explanatory variables in the multivariate logistic regression analysis with prognosis as the response variable. Therefore, warfarin use is speculated to be a factor improving the prognosis of ALF. However, warfarin is often used to treat heart diseases, such as atrial fibrillation. This finding may thus not indicate the direct effects of warfarin, but rather reflects a good prognosis for heart failure-induced ALF. Hence, we assessed the independence of warfarin use and presence or absence of heart failure causing liver failure and performed a multivariate logistic regression analysis including the presence or absence of heart failure as a variable. As a result, heart failure and warfarin use were selected as independent prognostic factors. These results suggest that the emergency survival rates of ALF patients may be improved by treatment with warfarin.
ConclusionThe SOFA score on emergency admission is an excellent indicator of the prognosis in liver failure from a systemic cause patients. In addition, the use of warfarin use prior to disease onset is believed to be a factor improving the prognosis in this patient population.
Abbreviations- •
ALF: acute liver failure.
- •
AT-III: anti-thrombin-III.
- •
CI: confidence interval.
- •
DIC: disseminated intravascular coagulation.
- •
FDP: fibrinogen degradation products.
- •
GCS: Glasgow Coma Scale.
- •
PT-INR: prothrombin time-international normalized ratio.
- •
SD: standard deviation.
- •
SIRS: systemic inflammatory response syndrome.
- •
SOFA: Sequential Organ Failure Assessment.
None of authors has grants and other financial support in the subject of this manuscript.